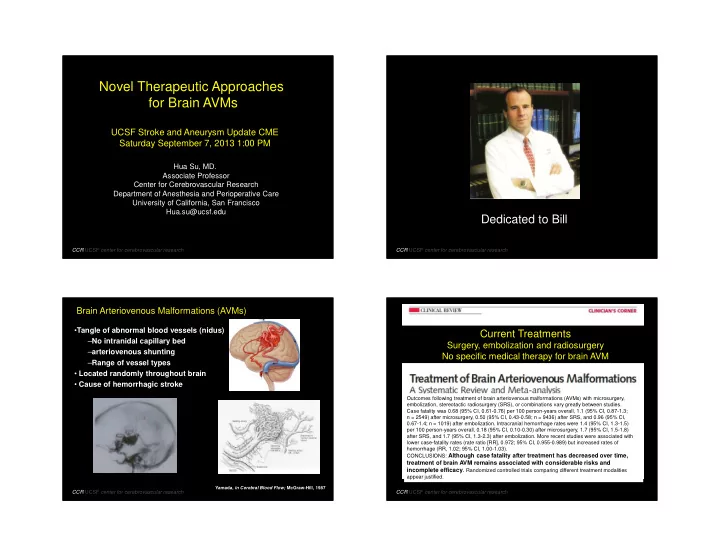
9/7/2013 Novel Therapeutic Approaches for Brain AVMs UCSF Stroke and Aneurysm Update CME Saturday September 7, 2013 1:00 PM Hua Su, MD. Associate Professor Center for Cerebrovascular Research Department of Anesthesia and Perioperative Care University of California, San Francisco Hua.su@ucsf.edu Dedicated to Bill CCR UCSF center for cerebrovascular research CCR UCSF center for cerebrovascular research Brain Arteriovenous Malformations (AVMs) • Tangle of abnormal blood vessels (nidus) Current Treatments – No intranidal capillary bed Surgery, embolization and radiosurgery – arteriovenous shunting No specific medical therapy for brain AVM – Range of vessel types • Located randomly throughout brain • Cause of hemorrhagic stroke Outcomes following treatment of brain arteriovenous malformations (AVMs) with microsurgery, embolization, stereotactic radiosurgery (SRS), or combinations vary greatly between studies. Case fatality was 0.68 (95% CI, 0.61-0.76) per 100 person-years overall, 1.1 (95% CI, 0.87-1.3; Outcomes following treatment of brain arteriovenous n = 2549) after microsurgery, 0.50 (95% CI, 0.43-0.58; n = 9436) after SRS, and 0.96 (95% CI, 0.67-1.4; n = 1019) after embolization. Intracranial hemorrhage rates were 1.4 (95% CI, 1.3-1.5) malformations (AVMs) with microsurgery, embolization, per 100 person-years overall, 0.18 (95% CI, 0.10-0.30) after microsurgery, 1.7 (95% CI, 1.5-1.8) stereotactic radiosurgery (SRS), or combinations vary after SRS, and 1.7 (95% CI, 1.3-2.3) after embolization. More recent studies were associated with lower case-fatality rates (rate ratio [RR], 0.972; 95% CI, 0.955-0.989) but increased rates of greatly between studies. hemorrhage (RR, 1.02; 95% CI, 1.00-1.03). CONCLUSIONS: Although case fatality after treatment has decreased over time, treatment of brain AVM remains associated with considerable risks and incomplete efficacy . Randomized controlled trials comparing different treatment modalities appear justified. Yamada, in Cerebral Blood Flow; McGraw-Hill, 1987 CCR UCSF center for cerebrovascular research CCR UCSF center for cerebrovascular research 1
9/7/2013 A Randomized trial of UNRUPTURED Brain Arteriovenous Malformations NIH/NINDS Grant 1UO1 NS051483 JP Mohr, AJ Moskowitz, C Stapf Best Possible vs. Deferred Invasive Treatment Unlike cancer-related chemotherapy that aims to shrink for those deemed suitable for eradication abnormal tumor tissue as cytotoxic therapy, the concept for the Randomization plan 1:1 = 400 cases treatment of brain AVM would be to stabilize vascular tissue and thereby decrease the risk of spontaneous ICH. Comparison of any invasive therapy to medical management arm (defer invasive treatment for up to 5 years). The trial stopped early due to a huge effect in favor of the medical management arm. CCR UCSF center for cerebrovascular research CCR UCSF center for cerebrovascular research Tissue assays of surgical specimens: “ angiogenesis run amok” “a healing wound” endothelium Identify Specific Targets Notch aVB3 Ki-67 -Analyzing surgical specimens Macrophage VEGF-R Tie-2 & Leukocytes Hashimoto, Neurosurgery 54: 410, 2004 -Modeling brain AVM in animals Shenkar, Neurosurgery 52: 465, 2003 MMP-9 Kilic, Neurosurgery 57: 997, 2005 VEGF Imbalance in Sure, Neurosurgery 55: 663, 2004 HIF-1 α Angiopoietin 1 & 2 Sonstein; J Neurosurg 85:838, 1996 ZhuGe, Q. et al. Brain 2009 astrocyte Notch Murphy, PA. Laboratory Investigation 2009 smooth muscle CCR UCSF center for cerebrovascular research CCR UCSF center for cerebrovascular research 2
9/7/2013 Are brain AVMs heritable? Hereditary Hemorrhagic Telangiectasia (HHT) Rendu-Osler-Weber Syndrome • Familial • Autosomal dominant disorder – Hereditary Hemorrhagic Telangiectasias (HHT) • Mucocutaneous telangiectasia – RASA1 (p120 RasGAP, is a Ras GTPase–activating • AVMs in Liver, Lung and Brain protein) capillary malformation-AVM • 80% of cases have functional heploinsufficiency of • Eerola, Am J Hum Genet 73: 1240, 2003 Endoglin (HHT1) or ALK1 (HHT2) – Non-HHT Brain AVMs Liver AVM Lung AVM • 53 patients in 25 families – van Beijnum, et al, JNNP 78: 1213, 2007 – Inoue, et al, Stroke 38: 1368, 2007 • Sporadic – 95-98% no family hx CCR UCSF center for cerebrovascular research CCR UCSF center for cerebrovascular research Alk1 Regional Conditional Deletion Plus VEGF AdCre – Regional Conditional Deletion of Alk1 Stimulation Results in Brain AVM Alk1 -/- Exon 3 Exon 7 AdCre + AAV-VEGF Angiogenesis Exons 4, 5, 6 8 wks Alk 1 gene Promoter loxp loxp AdCre CMV Promoter Cre recombinase Exon 7 Exon 3 Exons 4,5,6 are deleted from Alk1 Promoter genome loxp CCR UCSF center for cerebrovascular research CCR UCSF center for cerebrovascular research Walker et al. Ann Neurology, 2011 3
9/7/2013 VEGF Stimulation is Necessary for Brain Macrophage Infiltration AVM Formation Alk1 -/- /VEGF Alk1 -/- only Alk1 +/+ /VEGF Alk1 +/+ /VEGF Walker et al. Ann Neurology, 2011 CCR UCSF center for cerebrovascular research CCR UCSF center for cerebrovascular research Chen et al. ATVB, 2013 PDGFB Signaling Regulates Smooth Muscle Microhemorrhage Recruitment Chen et al. ATVB, 2013 Hellstrom; Development, 1999 CCR UCSF center for cerebrovascular research CCR UCSF center for cerebrovascular research 4
9/7/2013 ALK1 Knockdown Attenuates the Upregulation of PDGFB in ALK1 knockdown in HBMEC impairs the pericyte HBMEC in Response to VEGF Stimulation recruitment B A 3 B 5 A Control Fold Change 2.5 Control Alk1 mRNA Pdgfb mRNA Fold Change 4 shAlk1 Control shAlk1 2 3 VEGF 1.5 * 2 1 * shAlk1 * * 0.5 1 * * VEGF + shAlk1 * * * 0 0 VEGF 0 10 50 100 20 40 60 VEGF 0 10 50 100 (ng /ml) (ng /ml) Average Pericyte Distance µm HBMEC (human brain microvascular endothelial cell) were transfected with control shRNA or shRNA . Cells with >70% reduction of Alk1 gene expression were cultured for 18 h in the presence or absence of VEGF (0, 10, 50, and 100 ng/ml). qRT-PCR was performed for Alk1 (A) and Pdgfb (B) . All data are shown as mean and SD. *p<0.05 vs. control. CCR UCSF center for cerebrovascular research CCR UCSF center for cerebrovascular research Gene Mutation in Bone Marrow Transmits Potential Therapies for Brain AVMs the Phenotype 1. Anti-inflammation: Minocycline 2. Anti-angiogenesis: Avastin, sFLT 3. Increase PDGFB, improve vessel integrity Thalidomide 4. Bone marrow transplantation Peripheral monocyte/progenitor transfusion 50 µm CCR UCSF center for cerebrovascular research CCR UCSF center for cerebrovascular research 5
9/7/2013 Anti-Inflammation Anti-Angiogenesis Doxycycline Treatment Reduces Angiogenesis in Bevacizumab reverse brain AVM phenotype VEGF Treated Mouse Brain Walker et al. Stroke, 2012 CCR UCSF center for cerebrovascular research Lee, C. Z. et al. Stroke 2004 CCR UCSF center for cerebrovascular research Anti-Angiogenesis Anti-Angiogenesis Systemic Delivery of AAV9-sFLT Inhibited the Brain AVM Formation Stereotactic Injection of AAV2-sFLT Inhibited Brain AVM Formation Control Control Treated Treated CCR UCSF center for cerebrovascular research CCR UCSF center for cerebrovascular research 6
9/7/2013 Increase PDGFB Thalidomide Treatment Reduced the Number of Abnormal Vessels Increase PDGFB Lebrin, et al, Nat Med 16: 420, 2010 CCR UCSF center for cerebrovascular research CCR UCSF center for cerebrovascular research Increase PDGFB Summary Thalidomide Treatment Reduced Microhemorrhage 1. Invasive therapies are associated with considerable risks 2. No specific medical therapy is available 3. The concept for the treatment of brain AVM is to stabilize vascular tissue and thereby decrease the risk of spontaneous ICH. 4. Novel therapeutic approaches: A. Anti-inflammation B. Anti-angiogenesis C. Improve vascular integrity D. Correct gene mutation in BM monocyte/progenitors CCR UCSF center for cerebrovascular research CCR UCSF center for cerebrovascular research 7
9/7/2013 avm ucsf UCSF center for cerebrovascular research William L. Young Anesthesia, Neurosurg, Neurol Funding: Helen Kim Anesthesia, Epi & Biostats, IHG Hua Su Anesthesia NIH / NINDS Ludmila Pawlikowska Anesthesia, IHG NIH / ORDR AHA Tomoki Hashimoto Anesthesia Chanhung Lee Anesthesia Lesle Monzer Nerissa U. Ko Neurology Fundation Michael T. Lawton Neurosurgery Michael Ryan Charles E. McCulloch Epi & Biostats Zodda Fundation Jonathan G. Zaroff Kaiser Cardiology CCR UCSF center for cerebrovascular research 8
Recommend
More recommend