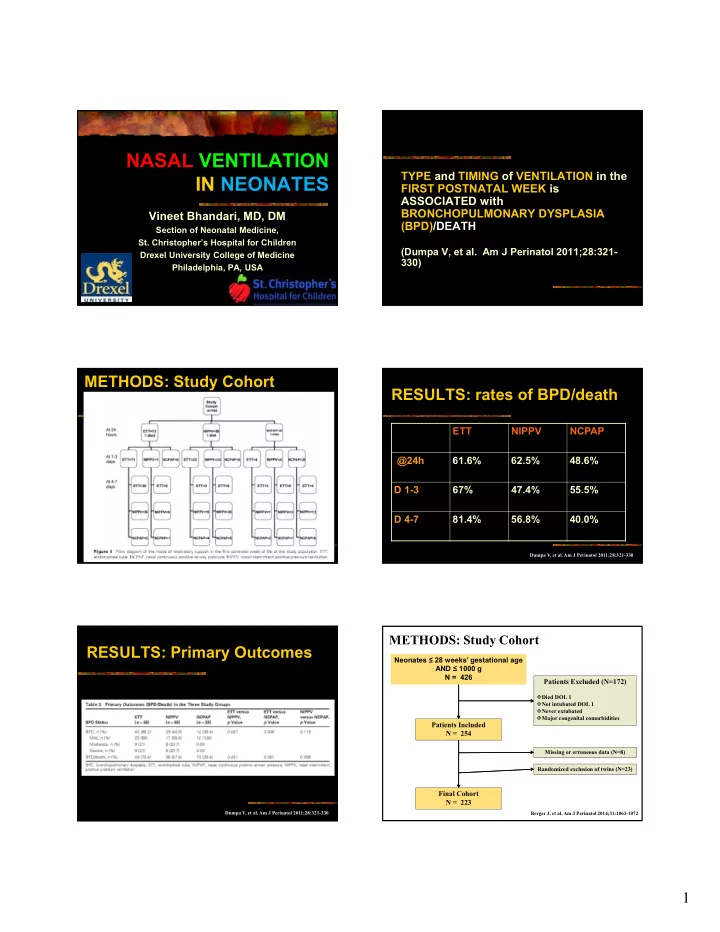
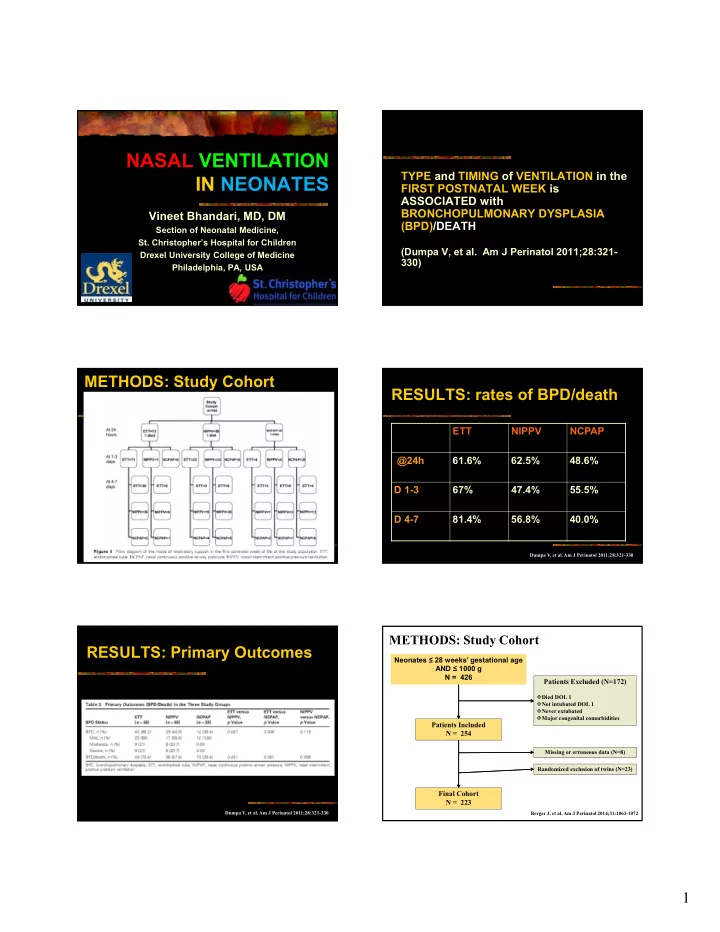
NASAL VENTILATION TYPE and TIMING of VENTILATION in the IN NEONATES FIRST POSTNATAL WEEK is ASSOCIATED with BRONCHOPULMONARY DYSPLASIA Vineet Bhandari, MD, DM (BPD)/DEATH Section of Neonatal Medicine, St. Christopher’s Hospital for Children (Dumpa V, et al. Am J Perinatol 2011;28:321- Drexel University College of Medicine 330) Philadelphia, PA, USA METHODS: Study Cohort RESULTS: rates of BPD/death ETT NIPPV NCPAP @24h 61.6% 62.5% 48.6% D 1-3 67% 47.4% 55.5% D 4-7 81.4% 56.8% 40.0% Dumpa V, et al. Am J Perinatol 2011;28:321-330 METHODS: Study Cohort RESULTS: Primary Outcomes Neonates ≤ 28 weeks’ gestational age AND ≤ 1000 g N = 426 Patients Excluded (N=172) Died DOL 1 Not intubated DOL 1 Never extubated Major congenital comorbidities Patients Included N = 254 Missing or erroneous data (N=8) Randomized exclusion of twins (N=23) Final Cohort N = 223 Dumpa V, et al. Am J Perinatol 2011;28:321-330 Berger J, et al. Am J Perinatol 2014;31:1063-1072 1
Overall unadjusted survival varies Compared to early extubation, late significantly by day of first extubation extubation increases risk of BPD Unadjusted Survival: BPD Unadjusted Survival: BPD Extubation Group Hazard Ratio 95% Confidence Interval P-value DOL 4-7 vs DOL 1-3 1.441 0.877, 2.370 0.1496 -- Extubated DOL 1-3 Probability of No BPD DOL 8+ vs DOL 1-3 5.353 3.601, 7.956 < 0.0001 -- Extubated DOL 4-7 -- Extubated DOL 8+ DOL 8+ vs DOL 4-7 3.7137 2.3823, 5.7891 < 0.0001 Adjusted Survival: BPD Overall Log-rank p < 0.0001 Extubation Group Hazard Ratio 95% Confidence Interval P-value DOL 4-7 vs DOL 1-3 1.908 1.067, 3.412 0.0292 DOL 8+ vs DOL 1-3 12.671 7.564, 21.228 < 0.0001 DOL 8+ vs DOL 4-7 6.6398 3.9808, 11.0749 < 0.0001 Adjusted for gestational age, race, gender, antenatal steroid use, APGAR scores, multiple gestation, mode of delivery, delivery room resuscitation efforts, surfactant delivery, neonatal comorbidities, and need for reintubation Time from First Extubation (d) Berger J, et al. Am J Perinatol 2014;31:1063-1072 Berger J, et al. Am J Perinatol 2014;31:1063-1072 Early extubation prevents BPD even RESULTS: Severity of BPD by when reintubation is necessary extubation DOL Study Cohort N = 223 DOL 1-3 DOL 4-7 DOL > 7 First N = 83 N = 34 N = 106 Extubation Yes No Yes No Yes No Extubation N = 58 N = 25 N = 27 N = 7 N = 76 N = 30 Failure (69.9%) (30.1%) (79.4%) (20.6%) (71.7%) (28.3%) Hazard ratio: 1.4648 Hazard ratio: 15.8807 Hazard ratio: 9.3911 95% CI: 0.3963, 5.4137 95% CI: 8.1679, 30.8766 95% CI: 4.9083, 17.9682 P = 0.5671 P < 0.0001 P < 0.0001 Berger J, et al. Am J Perinatol 2014;31:1063-1072 Berger J, et al. Am J Perinatol 2014;31:1063-1072 TIMING OF EXTUBATION and BPD RE-INTUBATION and BPD Reintubation rates do not When adjusting for multiple relevant significantly differ across study factors, extubation DOL 1-3 is associated with a significantly reduced hazard of groups BPD when compared to extubation DOL Babies who fail early extubation and 4-7 or extubation after the first week of life need to be reintubated are still at a Extubation DOL 4-7 is also associated lower risk of BPD than babies who with a significantly reduced hazard of are first extubated later in life and do BPD when compared to extubation after not need to be reintubated the first week of life Berger J, et al. Am J Perinatol 2014;31:1063-1072 Berger J, et al. Am J Perinatol 2014;31:1063-1072 2
RE-INTUBATION and BPD RE-INTUBATION and BPD Jensen EA, et al. JAMA Pediatr 2015;169:1011-1017 Jensen EA, et al. JAMA Pediatr 2015;169:1011-1017 RE-INTUBATION and BPD N=224, <27 weeks GA studied A PROSPECTIVE RANDOMIZED Infants who were younger at initial extubation spent CONTROLLED TRIAL COMPARING less time on the ventilator SYNCHRONIZED NASAL INTERMITTENT 64% infants had to be re-intubated POSITIVE PRESSURE VENTILATION Every day first extubation attempt is delayed: $4555 (SNIPPV) VERSUS NASAL CONTINUOUS in extra hospital charges POSITIVE AIRWAY PRESSURE (NCPAP) Older the infant at first extubation attempt, the more likely the infant will have moderate-to-severe BPD (Khalaf MN, et al. Pediatrics 2001;108:13-17) Re-intubation not associated with mortality, moderate-severe BPD, or length of stay Robbins M, et al. J Neonatal-Perinatal Med 2015;8:91-97 SELECTED SUPPORTIVE STUDIES OF SNIPPV USE IN NEONATES RESULTS SNIPPV NCPAP p Author/Year Type Mode N SNIPPV Group Control Group Outcomes (n =34) (n =30) value Friedlich RCT 2 0 41 SNIPPV^: Rate: NP-CPAP: Less failed 1999 10; PIP: same clinician extubation with as pre- discretion; SNIPPV Age at study (d) 4 (1-83) 2.5 (1-106) 0.95 extubation; FiO 2 adjusted PEEP: 4-6; Ti: for SpO 2 : 92- 0.6s; FiO 2 95% Wt. at study (gm) 1110 55 1200 75 0.32 adjusted for SpO 2 : 92-95% Pre-MAP (cm H 2 O) 4.9 0.2 5.1 0.2 0.38 Barrington RCT 2 0 54 SNIPPV: Rate: NCPAP: 6 Less failed 2001 12; PIP: 16 (to extubation with deliver at least SNIPPV Pre-FiO 2 0.30 0.02 0.30 0.01 0.84 12); PEEP: 6; Moretti RCT 2 0 63 SNIPPV: Rate: NCPAP: 3-5; Less failed AR (cm/H 2 O/L/s)* 169 16 205 21 0.18 2008 same as prior to Flow: 6-10 extubation with extubation; PIP: L/min; FiO 2 SNIPPV LC (ml/cmH 2 O)* 0.74 0.02 0.8 0.1 0.57 10-20; PEEP: 3- adjusted for 5; Flow: 6-10 SpO 2 : 90-94% L/min; FiO 2 Post-pH 7.36 + 0.03 7.34 + 0.02 0.14 adjusted for SpO 2 : 90-94% Post-CO 2 (mmHg) 37 + 1.0 40 + 2.0 0.06 Bhandari Retrospective 2 0 or for 469 SNIPPV: Rate: NCPAP: 4-6; SNIPPV group 2009 apnea same as prior to Flow: 8-10 (BW 500-750 g) extubation; PIP: L/min; FiO 2 had decreased Apnea (n) 2.24 0.8 2.03 0.7 0.84 increased by 2-4 adjusted for BPD, BPD/death, over pre- SpO 2 : 85-96% NDI and NDI/death < 0.01 Success (n, %) 32 (94) 18 (60) extubation values; PEEP: 6; Flow: 8-10 L/min; FiO 2 Data expressed as mean sem. *PFTs done on 53/64, 83% adjusted for SpO 2 : 85-96% 3
2 0 MODE: NCPAP vs NIPPV 2 0 MODE: NCPAP vs NIPPV The duration of NIV was significantly lower in NIPPV group as compared to NCPAP group (40.4 ± 39.3 hours versus 111.8 ± 116.4 hours, p = 0.003) The duration of supplementary oxygen was significantly lower in NIPPV versus NCPAP group (84.9 ± 92.1 hours versus 190.1 ± 140.5 hours, p = 0.002) The rates of BPD in NIPPV group (2/29, 6.9%) were significantly lower than in NCPAP group (9/28, 32.14%) (p = 0.02) Jasani, B et al. J Matern Fetal Neonatal Med 2016;29:1546-51 Jasani, B et al. J Matern Fetal Neonatal Med 2016;29:1546-51 NICU OUTCOMES CV SNIPPV P (n=21) (n=20) value BPD or Deaths (n, %) 11 (52) 4 (20) 0.03 A RANDOMIZED CONTROLLED TRIAL OF BPD (n, %) 7 (33) 2 (10) 0.04 Deaths (n, %) 4 (19) 2 (10) 0.66 SYNCHRONIZED NASAL INTERMITTENT Air leaks (n, %) 1 (5) 1 (5) 1.0 PDA (n, %) 3 (14) 4 (20) 0.70 POSITIVE PRESSURE (SNIPPV) IVH (n, %) 6 (29) 6 (30) 1.0 VENTILATION IN RDS PVL (n, %) 1 (5) 2 (10) 0.61 GER (n, %) 5 (25) 2 (10) 0.41 NEC (n, %) 6 (29) 6 (30) 1.0 ROP ≥ stage 2 (n, %) 1 (5) 3 (15) 0.34 (Bhandari V, et al. J Perinatol 2007;27:697-703) Total Duration of supplemental O 2 (days)* 46.8 ± 6.3 45.5 ± 6.1 0.88 Total Duration of ETTPPV (days)* 16.6 ± 3.1 12.7 ± 2.6 0.17 Total Duration of SNIPPV (days)* 9.8 ± 2.2 11.7 ± 2.1 0.27 Length of stay (days)* 65.0 ± 5.3 61.6 ± 5.2 0.65 Data expressed as *Mean sem 1 0 MODE: NCPAP vs NIPPV SELECTED STUDIES OF NIPPV USE IN NEONATES Author/Year Type Mode N NIPPV Group Control Group Outcomes Kugelman RCT 1 0 84 NIPPV: Rate: 12- NCPAP: 6-7; NIPPV group had 2007 30; PIP: 14- FiO 2 decreased BPD 22; PEEP: adjusted 6-7; Ti: 0.3s; for SpO 2 : FiO 2 88-92% adjusted for SpO 2 : 88- 92% Khorana RCT 2 0 48 NIPPV: Same as NCPAP: No differences in 2008 pre- Same as outcomes; extubation pre- however, there ventilator extubation were significant settings PEEP differences in the demographics of the 2 groups Sai Sunil RCT 1 0 76 NIPPV: Rate: 50; NCPAP: 5; Less failed Kishore PIP: 15-16; Flow: 6-7 extubation with 2009 PEEP: 5; Ti: L/min; NIPPV 0.3-0.35s; FiO 2 Flow: 6-7 adjusted L/min; FiO 2 for SpO 2 : adjusted for 88-93% SpO 2 : 88- 93% Armanian A-M, et al. Int J Prev Med 2014;5:1543-1551 4
1 0 MODE: NCPAP vs NIPPV 1 0 MODE: NCPAP vs NIPPV with MIST / LISA Armanian A-M, et al. Int J Prev Med 2014;5:1543-1551 Oncel MY, et al. Arch Dis Child Fetal Neonatal Ed 2016;101:F323-8 1 0 MODE: NCPAP vs NIPPV with MIST / LISA 1 0 MODE: NCPAP vs NIPPV with MIST / LISA Oncel MY, et al. Arch Dis Child Fetal Neonatal Ed 2016;101:F323-8 Oncel MY, et al. Arch Dis Child Fetal Neonatal Ed 2016;101:F323-8 NCPAP vs NIPPV (± MIST / LISA) FINAL THOUGHTS Attempt to extubate in the first 72h of life Efforts should focus on 24h – 72h “window” of opportunity to extubate Re-intubation at later postnatal ages does NOT worsen outcomes Oncel MY, et al. Arch Dis Child Fetal Neonatal Ed 2016;101:F323-8 5
LOSE THE TUBE FINAL THOUGHTS Secondary mode (S)NIPPV: Recommended as first choice for extubation Recommended to control apnea, escalating from NC to NCPAP to NIPPV, in an attempt to avoid intubation Primary mode (S)NIPPV - with or without LISA / MIST: additional RCTs needed for outcome of BPD St. Christopher’s Hospital for Children • Critical Care Tower • Advanced technology while incorporating families’ needs • 39 Level IV NICU beds At St. Chris things have a way of looking UP! 6
Recommend
More recommend