Mechanisms of macrolide resistance Ribosomal modification by - PowerPoint PPT Presentation
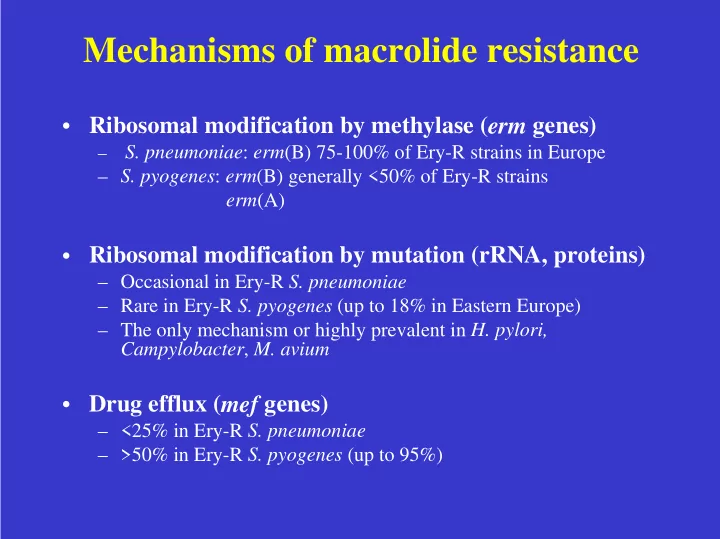
Mechanisms of macrolide resistance Ribosomal modification by methylase ( erm genes) S. pneumoniae : erm (B) 75-100% of Ery-R strains in Europe S. pyogenes : erm (B) generally <50% of Ery-R strains erm (A) Ribosomal modification by
Mechanisms of macrolide resistance • Ribosomal modification by methylase ( erm genes) – S. pneumoniae : erm (B) 75-100% of Ery-R strains in Europe – S. pyogenes : erm (B) generally <50% of Ery-R strains erm (A) • Ribosomal modification by mutation (rRNA, proteins) – Occasional in Ery-R S. pneumoniae – Rare in Ery-R S. pyogenes (up to 18% in Eastern Europe) – The only mechanism or highly prevalent in H. pylori, Campylobacter , M. avium • Drug efflux ( mef genes) – <25% in Ery-R S. pneumoniae – >50% in Ery-R S. pyogenes (up to 95%)
Genotypes and phenotypes of macrolide resistance in pneumococci Gene Phenotype Phenotype acronym 14-15-M 16-M erm (B) MLS B (i) R R(I-S) MLS B (c) R R mef (A) M R S Rarely erm (A) gene
MICs of macrolides against S. pneumoniae according to resistance phenotypes/genotypes MIC (mg/L) MLS B or erm (B) M or mef (A) range MIC50 MIC90 range MIC50 MIC90 Azithromycin 8->128 >128 >128 2-32 16 16 Clarithromycin 2->128 >128 >128 1-64 8 8 Erythromycin 8->128 >128 >128 1-64 8 8 Roxithromycin 2->128 >128 >128 1-32 8 8 Josamycin 0.5->128 16 >128 0.03-0.025 0.06 0.12 Miocamycin 4->16 2-16 >128 0.25-0.5 - - Spiramycin 16->128 8-128 >128 0.06-1 0.25 0.5 Descheemaker (agar CO2),Fitoussi (agar), Ip (agar), Montanari (NCCLS broth microdil), Nishijima (agar)
MICs of macrolides against S. pyogenes with erm genes Genotype Antimicrobial MIC (mg/L) Range MIC50 MIC90 erm (B) Erythromycin 1->128 >128 >128 Azithromycin 2->128 >128 >128 Clarithromycin 0.5->128 >128 >128 Roxithromycin 2->128 >128 >128 Josamycin 2->128 >128 >128 Miocamycin 16->16 >16 >16 Spiramycin 64->128 >128 >128 erm (A) Erythromycin 1->128 2->128 4->128 Azithromycin 2->128 8->128 32->128 Clarithromycin 0.5->128 1->128 2->128 Roxithromycin 2->128 16->128 16->128 Josamycin 0.06-1 0.03-0.25 0.06- 0.25 Miocamycin 0.06-0.5 0.25 0.25 Spiramycin 0.03-1 0.06-0.25 0.12-0.5 Bingen (NCCLS), Descheemaker (agar), Giovanetti (broth microdil.), Kataja (agar NCCLS)
MICs of macrolides against S. pyogenes with mef genes Genotype Antimicrobial MIC (mg/L) Range MIC50 MIC90 mef (A) Erythromycin 1-32 8 8-16 Azithromycin 2-32 2-8 2-8 Clarithromycin 0.5-16 2-8 4-8 Roxithromycin 2-64 16 16 Josamycin 0.01-1 0.03-0.25 0.12-0.5 Miocamycin 0.06-0.5 0.25 0.25 Spiramycin 0.03-1 0.06-0.25 0.12-0.5 Descheemaker (agar), Giovanetti (broth microdil.), Kataja (agar NCCLS)
Ribosomal mutation and macrolide resistance in pneumococci Azi Cla Ery Rox A2058U/G >32 16->32 >32 >32 A2059G >32 2 8 16 C2610U 0.125 0.03 0.06 0.125 C2611U 0.5 0.03-0.06 0.06-0.12 0.06-0.5 L22 protein 0.06-1 0.12-1 0.25-1 0.5-2 L4 protein 0.5 0.12 0.25 0.5 Canu et al., 2002
Population analysis of erythromycin-susceptible and resistant S. pneumoniae No of strains 50 45 40 35 30 25 20 15 10 5 MIC of 0 erythromycin (mg/L) 0.03 0.06 0.12 0.25 0.5 1 2 4 8 16 32 64 128 Phenotype M MLS B S
Microbiological breakpoint • Easy to determine for macrolides • May differ by one or two dilutions according to the methodology used (national committees), but equivalence exists • Clinical significance ? • Two kinds of breakpoints: microbiological and clinical? ! In fact for macrolides, the lower breakpoint is often the microbiological breakpoint Erythromycin and S. pneumoniae S: BSAC: <=0.5mg/L, CA-SFM: <=1mg/L, NCCLS: <=0.25mg/L
Different levels of resistance to macrolides • S. pneumoniae and S. pyogenes with erm (B) generally highly cross-resistant to all macrolides • S. pneumoniae and S. pyogenes with efflux or erm (A) generally moderately resistant to 14-15-Md macrolides MIC50 (mg/L) S. pyogenes S. pneumoniae Erythromycin 8 16 Azithromycin 2-8 8 Clarithromycin 2-8 8 Roxithromycin 16 8
Various significances of a moderate level of resistance to macrolides • Streptococcus pyogenes with MIC of erythromycin equal to 8 mg/L may contain – mef (A) gene: 16-Md macrolides and clindamycin active (« safe » use) – Inducible erm (A) gene: 16-Md macrolides and clindamycin active but risk for selection of constitutive mutants (10 -7 ) – Inducible erm (B) gene: MIC of erythromycin increases after culture in the presence of erythromycin (in vivo?) ! detection of the resistance phenotype ! interpretive reading of the susceptibility test ! answer to the clinician
Azithromycin 10 vs 20 mg/kg/d for 3 days in acute GAS pharyngitis (1) • Inclusion – Children between 2-12 years of age – Acute tonsillopharyngitis – Positive card test for streptococcal antigen confirmed by positive throat culture for GAS • Exclusion – Antibiotics within 8 days – Hypersensitivity to beta-lactams or macrolides, severe underlying disease, previous inclusion, symptoms suggestive of viral infection • Treatment – Azithromycin 10 mg/kg/d vs 20 mg/kg/d; 3 days (double-blinded) – Penicillin V 45 mg/kg/d; 10 days (open) – Clinical and bacteriological follow-up: days 14 and 30 Cohen R et al. Pediatric Infectious Diseases Journal, in Press
Outcome on day 14 (ITT-assessable patients) AZM AZM Penicillin V 10 mg/kg/d 20 mg/kg/d Microbiological outcome Total no of patients 158 157 154 No of failures (%) 79 (50) 22 (14) 27 (17.5) Clinical outcome Total no of patients 169 165 167 No of failures (%) 28 (16.6) 14 (8.5) 12 (7.2)
Pre- and post-treatment GAS isolates Isolate MIC of (mg/L) Mechanism Ery Azi Jos of R Pre-treatment 0.064 0.12 0.5 None strains -0.25 Post-treatment Strains 11 V2 0.5 2 1 L4 mutation 124 V2 0.5 1 1 L4 mutation 390 V2 1 2 2 L4 mutation 286 V2 >128 >128 >128 erm (B) 133 V2 8 8 2 unknown 323 V2 32 >128 128 unknown 508 8 8 0.5 mef (A) All pre- and post-treatment strains were related (PFGE and RAPD). Strains 286 and 508 acquired a DNA fragment with erm (B) and mef (A), respectively
Resistance by ribosomal mutation in Helicobacter , Campylobacter , M. avium • H. pylori : mutation of 23S rRNA – MIC of clarithromycin: 8-256 mg/L, depending on the mutation • M. avium : mutation of 23S rRNA – MIC of clarithromycin > 8 mg/L (generally >128 mg/L) (some strains with MIC=1 mg/L) • Campylobacter : mutation of 23S rRNA and… – MIC of erythromycin 1->128 mg/L
Chlamydia trachomatis -Three strains: 2 with clinical failure and relapse after treatment with azithromycin MIC of azithromycin >4 mg/L Somani et al., J Infect Dis 2000;181:1421-7
Recommend
More recommend
Explore More Topics
Stay informed with curated content and fresh updates.

![[G OOGLE F ILE S YSTEM ] Shrideep Pallickara Computer Science Colorado State University CS555:](https://c.sambuz.com/705979/g-oogle-f-ile-s-ystem-s.webp)