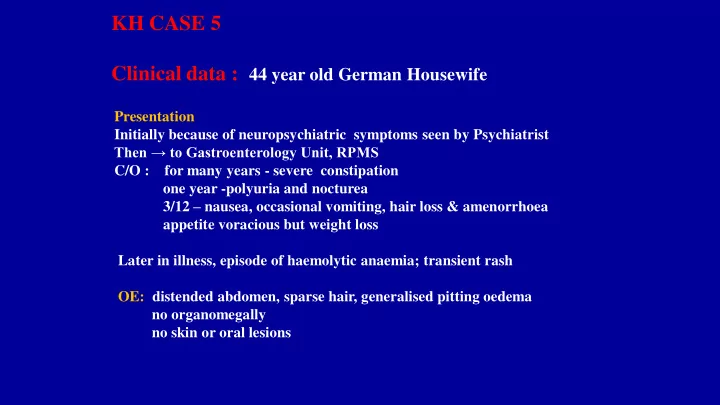
KH CASE 5 Clinical data : 44 year old German Housewife Presentation Initially because of neuropsychiatric symptoms seen by Psychiatrist Then → to Gastroenterology Unit, RPMS C/O : for many years - severe constipation one year -polyuria and nocturea 3/12 – nausea, occasional vomiting, hair loss & amenorrhoea appetite voracious but weight loss Later in illness, episode of haemolytic anaemia; transient rash OE: distended abdomen, sparse hair, generalised pitting oedema no organomegally no skin or oral lesions
Laboratoty Investigations Haematology: HB. 11.9g/100ml; mild hypochromic change WBC count 8,000/c ml – normal differential; ESR - several occasions region of 90 mm/hr Biochemistry plasma urea and electrolytes normal LFTs, bilirubin, alkaline phosphatase, lactic dehydrogenase normal Isocitric dehydrofenase 23 IU (normal 3-8 IU) Renal function- No proteinuria or haematuria. Urine occassional pus cells. Culture – E Coli Intestinal function Mild statorrhoea No protein losing enteropathy. Schilling test; Vitamin B12 malabsorption Glucose tolerance test showed mildly diabetic curve Indican excretion markedly raised
IMAGING Normal liver scan Barium meal and follow through: marked dilatation, increased caibre and thickened folds of small intestine; intestinal transit very slow
Laparotomy Marked hypertrophy, dilatation and oedema of the small intestine Gross retention of faeces in colon Jejunal biopsy: visually lengthened villi – confirmed by dissecting microscope LENNON Patient’s SI ⃪ dissecting microscope dissecting microscope → normal SI
Jejunal biopsy microscopy villi greatly lenghthened ↑1,350μ (normal 350 -750 μ ) Enterocytes normal
Post – Laparotomy developed urinary infection IVP & MRI → Rt. renal mass ? Carcinoma Nephrectomy - 7 cm tumour in mid-portion of kidney Small lymph node adjacent to IVF – contained metastasis
Renal tumour
Immunofluorecence image of tumour cells showing cross – reactivity with Mab→ glucagon. Note polar location of immunofluorescence which matched location of secretory granules in tumour cells EMS
Renal tumour - carcinoid-like histopathology
Renal tumour light microscopy- Fig. 4 Gleeson et al. Gut 12, 1971 1
EM jejunal biopsy -- neurosecretory granules consistent with size of glucagon and entero – glucagon secretory granules Note position of sec. granules at terminal aspect of enterocytes
Following renal tumour resection: A few weeks later, patient’s constipation disappeared and she developed frequent and loose stools Hair growth restored, no longer amenorrhoeic or psychotic Repeat imaging showed normal SI Repeat Jejunal biobsy showed normal villous height
Imaging of SI. Post-Op. normal pattern
Post renal tumour resection - jejunal biopsy villi now normal height
Final Diagnosis: Paraneoplastic Enteroglocagonoma Syndrome associated with a neuroendocrine carcinoid – like tumour of the kidney
Discussion Since the patient’s synptoms and investigations did not fit with those of the Enteroglucagon Syndrome, tumour cells were then reacted with specific pro-glucagon peptide of intestinal type – enteroglucagon; found to be positive The diagnosis was now made of an enteronglucagonoma There has not to my knowledge been reported a neuroendocrine tumour – carcinoid like - in the kidney of enteroglucagon type Renal carcinoids are extremely rare and so it is postulated that the tumour cells have been hijacked and co-opted to secrete pro – glucagon peptide - Enteroglucagon There is also debate on the histogenesis of renal carcinoids (see handouts)
References 1. Gleeson MH, Bloom Sr, Polak JM, Henry K, Dowling RH. Endocrine tumour in Kidney affecting small bowel structure, motility and absorptive function. Gut 1971; 12:773-782 2. McGrath M, Ungar RH, Recant L et al. A glucagonoma secreting alpha cells of pancreas. N.Eng, H Med. 1966; 274:1408 - 1413 3. Bloom SR. An enteroglucagon tumour. Gut 1972; 13:520-523 4. Werner RA, Fotourechi V, Wynne AG et al. The Glucagonoma Syndrome: clinical, and pathologic features in 21 patients. Medicine; 75: 53-63 5. Teix1era RC, Simonson Nico MM, Ghidti AC. Ncrolytic migratory Erythema with glucagonoma: a report of 2 cases. Clinica 2008; 63: 267- 270 6. Hansen MB. The enteric nervous system II. Gastrointestinal functions. Pharmacol. Toxicol. 2003; 92: 249-257 7. Drucker DJ. Gut adaptation and the peptides GLP-1 and GLP-2 enteroendocrine cells of small intestine and colon. Gut 2002; 50: 428-435 8. Livak DA. Glucagon-like peptide 2 is a potent growth factor for small intestine and colon. Gastrointestinal Surg, 1998; 2: 146-150. 9, Stevens FM, Flanagan RW. O’Gorman D, Buchanon KD. Glucagonoma syndrome demonstrating giant villi. Gut 1984; 25:784-791 10. Shurtleff BT, Schvants O, Rajfer J. Carcinoid tumour of the kidney; a case report and review of the literature. Rev. Urol 2005; 7:229-2332005 ; 7: 229 -233
Take home message Early recognition of a paraneoplastic syndrome by clinicians – including pathologists- is of paramount importance since it will lead to earlier diagnosis of the tumour with improved therapy and prognosis and avoid misdiagnoses
Recommend
More recommend