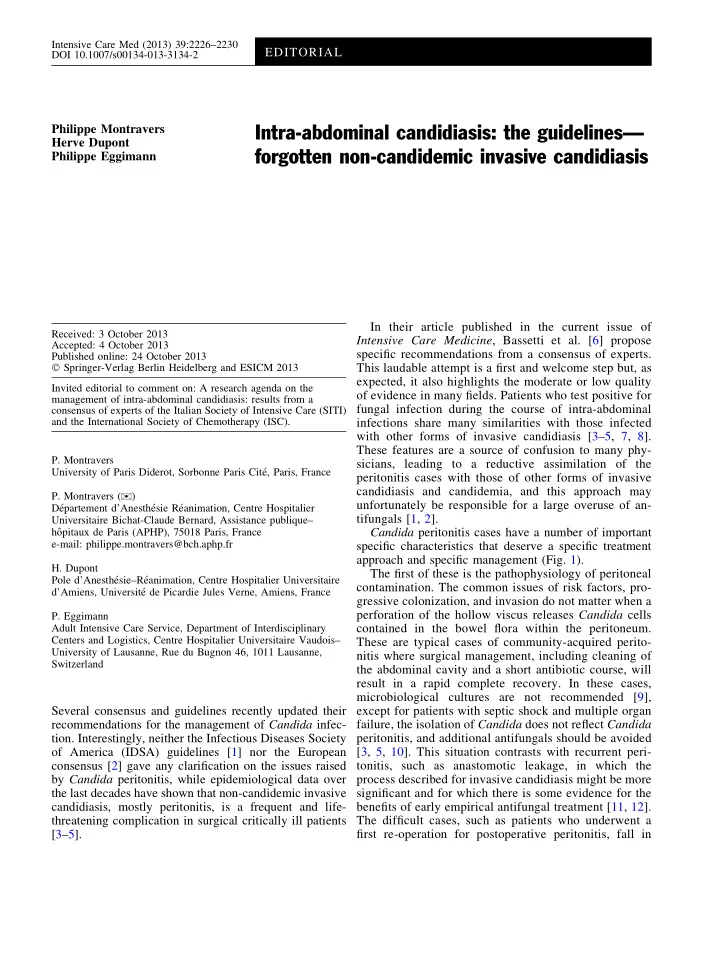
Intensive Care Med (2013) 39:2226–2230 EDITORIAL DOI 10.1007/s00134-013-3134-2 Philippe Montravers Intra-abdominal candidiasis: the guidelines— Herve Dupont forgotten non-candidemic invasive candidiasis Philippe Eggimann In their article published in the current issue of Received: 3 October 2013 Intensive Care Medicine , Bassetti et al. [6] propose Accepted: 4 October 2013 specific recommendations from a consensus of experts. Published online: 24 October 2013 � Springer-Verlag Berlin Heidelberg and ESICM 2013 This laudable attempt is a first and welcome step but, as expected, it also highlights the moderate or low quality Invited editorial to comment on: A research agenda on the of evidence in many fields. Patients who test positive for management of intra-abdominal candidiasis: results from a fungal infection during the course of intra-abdominal consensus of experts of the Italian Society of Intensive Care (SITI) and the International Society of Chemotherapy (ISC). infections share many similarities with those infected with other forms of invasive candidiasis [3–5, 7, 8]. These features are a source of confusion to many phy- P. Montravers sicians, leading to a reductive assimilation of the University of Paris Diderot, Sorbonne Paris Cite ´, Paris, France peritonitis cases with those of other forms of invasive candidiasis and candidemia, and this approach may P. Montravers ( ) ) unfortunately be responsible for a large overuse of an- De ´partement d’Anesthe ´sie Re ´animation, Centre Hospitalier tifungals [1, 2]. Universitaire Bichat-Claude Bernard, Assistance publique– ho ˆpitaux de Paris (APHP), 75018 Paris, France Candida peritonitis cases have a number of important e-mail: philippe.montravers@bch.aphp.fr specific characteristics that deserve a specific treatment approach and specific management (Fig. 1). H. Dupont The first of these is the pathophysiology of peritoneal ´sie–Re ´animation, Centre Hospitalier Universitaire Pole d’Anesthe contamination. The common issues of risk factors, pro- ´ de Picardie Jules Verne, Amiens, France d’Amiens, Universite gressive colonization, and invasion do not matter when a perforation of the hollow viscus releases Candida cells P. Eggimann Adult Intensive Care Service, Department of Interdisciplinary contained in the bowel flora within the peritoneum. Centers and Logistics, Centre Hospitalier Universitaire Vaudois– These are typical cases of community-acquired perito- University of Lausanne, Rue du Bugnon 46, 1011 Lausanne, nitis where surgical management, including cleaning of Switzerland the abdominal cavity and a short antibiotic course, will result in a rapid complete recovery. In these cases, microbiological cultures are not recommended [9], Several consensus and guidelines recently updated their except for patients with septic shock and multiple organ failure, the isolation of Candida does not reflect Candida recommendations for the management of Candida infec- tion. Interestingly, neither the Infectious Diseases Society peritonitis, and additional antifungals should be avoided of America (IDSA) guidelines [1] nor the European [3, 5, 10]. This situation contrasts with recurrent peri- consensus [2] gave any clarification on the issues raised tonitis, such as anastomotic leakage, in which the by Candida peritonitis, while epidemiological data over process described for invasive candidiasis might be more the last decades have shown that non-candidemic invasive significant and for which there is some evidence for the candidiasis, mostly peritonitis, is a frequent and life- benefits of early empirical antifungal treatment [11, 12]. threatening complication in surgical critically ill patients The difficult cases, such as patients who underwent a [3–5]. first re-operation for postoperative peritonitis, fall in
2227 Fig. 1 Specific characteristics Secondary peritonitis Scheduled surgery of Candida peritonitis. Secondary perforation of the Candida spp hollow viscus releases Candida Gram positive cells within the peritoneum. Gram negative Except for patients with septic shock and multiple organ failure, antifungals are not recommended in this setting. In recurrent peritonitis, such as Postoperative anastomotic leakage, invasive ileus candidiasis might be more significant, and early empirical (2-5 days) antifungal treatment might be beneficial. Intermediate Recovery between these situations, such as patients who underwent a first re-operation for Upper postoperative peritonitis, the digestive tract prediction of Candida peritonitis is challenging, and an emergency antifungal Septic shock treatment is not a validated with MOF approach. ICU Intensive Care ICU stay Unit Empiric Antibiotics > 3 days antifungal Parenteral nutrition treatment ? Persistent sepsis Empiric antifungal treatment ? Candida peritonitis Candidemia (7-15 days) ( 7-15 days) Persistent ileus Septic shock Anastomosis leak New digestive surgery Empiric antifungal treatment ? between these two sketched situations and represent to treat these cases but rather ‘‘when’’ should we initiate situations where the prediction of Candida peritonitis is the antifungal treatment. In these circumstances, infection challenging. will not develop within hours but over days [3, 5, 13], and The second specific characteristic of Candida perito- except for candidemia reported in a minority of the nitis is that additional circumstances have been reported peritonitis cases [4, 5], an emergency antifungal treatment where Candida cells emerge progressively, influenced is not a validated approach, as would be the case in the through combined exposure to well-known risk factors, treatment of sepsis of bacterial origin. A large part of the such as broad-spectrum antibiotic pressure, previous common confusion lies in these different clinical situa- abdominal surgery, parenteral nutrition, renal replacement tions, as they complicate the decision-making process of therapy, central venous catheter, among others. In these the experts in coming to a consensus regarding the ‘‘at high risk’’ cases, the issue is no longer ‘‘do we need’’ diagnosis and treatment.
Recommend
More recommend