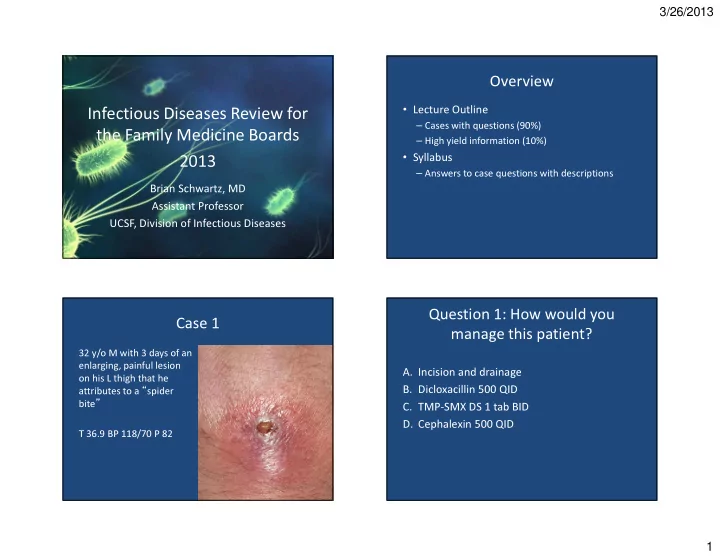
3/26/2013 Overview • Lecture Outline Infectious Diseases Review for – Cases with questions (90%) the Family Medicine Boards – High yield information (10%) • Syllabus 2013 – Answers to case questions with descriptions Brian Schwartz, MD Assistant Professor UCSF, Division of Infectious Diseases Question 1: How would you Case 1 manage this patient? 32 y/o M with 3 days of an attributes to a “ spider enlarging, painful lesion A. Incision and drainage bite ” on his L thigh that he B. Dicloxacillin 500 QID C. TMP-SMX DS 1 tab BID D. Cephalexin 500 QID T 36.9 BP 118/70 P 82 1
3/26/2013 Abscesses: Do antibiotics provide Antibiotic therapy is recommended benefit over I&D alone? for abscesses associated with: • Severe disease, rapidly progressive with 100% associated cellulitis or septic phlebitis 80% % patients cured • Signs or symptoms of systemic illness Placebo 60% • Associated comorbidities, immunosuppressed Antibiotic 40% p=.52 p=.25 p=.12 • Extremes of age 20% Cephalexin TMP-SMX TMP-SMX • Difficult to drain area (face, hand, genitalia) 0% Rajendran '07 Duong '09 Schmitz '10 • Failure of prior I&D Liu C. Clin Infect Dis . 2011 1 Rajendran AAC 2007; 2 Schmitz G Ann Emerg Med 2010; 3 Duong Ann Emerg Med 2009 Microbiology of Purulent SSTIs Empiric oral antibiotic Rx for uncomplicated purulent SSTI unknown non-B hemolytic 9% Drug Adult Dose strep other 4% 8% TMP/SMX DS 1-2 BID B-hemolytic strep Doxycycline, Minocycline 100 BID 3% MRSA MSSA Clindamycin 300-450 TID 59% 17% Linezolid 600 BID *Rifampin is NOT recommended for routine treatment of SSTIs Moran NEJM 2006 2
3/26/2013 Question 2: How would you Case 2 manage this patient? 28 y/o woman presents with erythema of her left A. Watch closely for self-resolution foot over past 48 hrs B. Cephalexin 500 mg QID, monitor clinically No purulent drainage, with addition of TMP/SMX if no response exudate , or fluctuance. C. TMP/ SMX 2 DS BID D. Doxycycline 100 BID T 37.0 BP 132/70 P 78 Eels SJ et al Epidemiology and Infection 2010 Empiric treatment of uncomplicated Summary: empiric management of SSTIs nonpurulent cellulitis? Non-purulent Purulent • Anti- β -hemolytic strep antibiotic (+/- anti-MSSA) (MRSA) (β-hemolytic strep) Cephalexin 500 QID Drug Adult Dose I&D Dicloxacillin 500 QID Uncomplicated Consider addition of anti-MRSA Cephalexin 500 QID Consider addition of MRSA active antibiotic in select situations 1 agent if no response 1 Dicloxacillin 500 QID I&D plus vancomycin Vancomycin Clindamycin* 300-450 TID Complicated (or alternative) 2 (or alternative) 2 Linezolid* 600 BID 1. Systemic illness, purulent cellulitis/wound infection, comorbidities, extremes of age, *Have activity against MRSA abscess difficult to drain or face/hand, septic phlebitis, lack of response of to I&D alone. PO antibiotic : TMP-SMX 1 DS BID, Clindamycin 300 mg TID, Doxycycline 100 PO BID • If poor response, add anti-MRSA antibiotic 2. Daptomycin, linezolid, telavancin, ceftaroline 3
3/26/2013 Case 3: A slight alteration… Question 3: What do you do? • 34 y/o comes in with A. Send home on cephalexin, TMP/SMZ, pain meds the similar symptoms B. Give IV vancomycin and cefazolin • Temp 38.9, HR 105, SBP C. Give IV vancomycin and cefazolin. Call 100, RR 20 surgery for morning consult. • Appears ill and in more D. Call surgery immediately. Give IV clindamycin, piperacillin-tazobactam, and pain than what you vancomycin would expect for cellulitis Necrotizing Fasciitis Necrotizing Fasciitis: Treatment • Clues: pain out of proportion to exam, toxic • Surgical debridement! appearing, blistering, rapidly spreading, • Empiric antibiotics decreased sensation – Pip/tazo or mero-, imipenem ( strep, GNR, anaerobes) plus • Bugs? - 2 forms – Clindamycin (protein synthesis inhibitor) – Monomicrobial: Group A Strep most common plus – Vancomycin (MRSA) – Polymicrobial: GNR, anaerobes • Narrow antibiotics based on cultures 4
3/26/2013 Question 4a: Does he need a CT Case 4 scan before getting an LP? • 61 y/o diabetic presents to ED with, fever, stiff • Febrile to 39 ° C with stable vital signs. neck, and new onset seizure. A. Yes B. No • Lethargic but able to answer questions. • Nuchal rigidity and photophobia seen but no focal neurological abnormalities. Question 4b: Which is the preferred Who needs a head CT before LP? Who is at high risk for herniation from LP? antibiotic regimen for this patient? • Patients at high risk for mass lesions or ( 61 y/o male ) increased intracranial pressure can be identified A. Ceftriaxone clinically and should then undergo CT scan B. Ceftriaxone and Vancomycin • Who are high risk patients? C. Ceftriaxone and Ampicillin – New-onset seizure – Immunocompromised D. Vancomycin and Ceftriaxone – Focal neurological finding and Ampicillin – Papilledema – Moderate-severe impairment of consciousness Hasbun R. NEJM. 2001. Gopal AK. Arch Int Med. 1999. 5
3/26/2013 Thigpen MC. NEJM.2011 Thigpen MC. NEJM.2011 IDSA algorithm for management of Empiric antimicrobial therapy bacterial meningitis Risk factor Pathogens Antimicrobials Indication for head CT < 1 month GBS, E. coli, Ampicillin + cefotaxime NO YES L. monocytogenes 1-23 months S. pneumoniae, Vancomycin + 3rd gen ceph Blood cx Blood cx + Lumbar puncture N. meningitidis, H. influenzae Steroids and empiric Steroids and empiric 2-50 yrs N. meningitidis, Vancomycin + 3rd gen ceph antimicrobials antimicrobials S. pneumoniae Head CT w/o mass lesion or > 50 yrs S. pneumoniae, Vancomycin+ 3rd gen ceph + CSF suggestive of bacterial herniation N. meningitidis, ampicillin meningitis L. monocytogenes Refine therapy Lumbar puncture Adapted from Tunkel AR. CID 2004; GBS=group B strep (Strep agalactiae), 3rd gen ceph=ceftriaxone or cefotaxime Tunkel AR. CID 2004 6
3/26/2013 Question 5: What do you Case 5 recommend? • 65 y/o diabetic woman presents to clinic for A. No antibiotics routine evaluation. She has been feeling well. B. Empiric ciprofloxacin and await A urinalysis and culture are sent. susceptibilities • UA: WBC->100, RBC-0, Protein-300 C. Repeat culture in 1 week and if bacteria still present then treat • The next day you are called because the urine culture has >100,000 Klebsiella pneumoniae Asymptomatic bacteriuria in Treatment of asymptomatic diabetic women bacteriuria? • Clear benefit • No benefit • Asymptomatic bacteriuria ~ 25% of diabetic – Pregnant women – Postmenopausal women (pyuria is usually present) – Pre traumatic ambulatory women • RCT, placebo controlled of 105 diabetic women – Institutionalized urologic • 1 ° endpoint: symptomatic UTI • 14 days of antibiotic vs. placebo – Spinal cord injuries interventions with mucosal bleeding – Patients with urinary • Possible benefit catheters – 42% antibiotic group vs. 40% placebo – Diabetics – neutropenic – RR 1.19 (0.28–1.81),p=0.42 Harding GKM. NEJM 2003 7
3/26/2013 Question: According to the updated Case 6 Infectious Diseases Society of America she has “ a urinary tract infection, again ” Guidelines - what is the 1 st line treatment • A 21 year-old college student, calls to say that for an uncomplicated UTI? • You have treated her for uncomplicated A. Ciprofloxacin 250mg BID x 3d B. Nitrofurantoin 100mg BID x 5d cystitis 2 times in the past year • You obtain a UA: C. TMP-SMX DS BID x 7d – Leukocyte esterase 3+, RBC 1+ D. Cephalexin 500 mg QID x 7d “ complicated? ” IDSA guidelines for uncomplicated What would make the UTI Goal: Low resistance and low “ collateral UTI treatment damage ” • Anatomic abnormality How would you treat? – Fluoroquinolones for • Indwelling catheter empiric therapy • Recent instrumentation – Obtain cultures • Men – Duration 7-14 days • Nitrofurantoin 100 mg PO BID x 5 days • Healthcare-associated • TMP-SMX DS PO BID x 3 days • Recent antimicrobial use – avoid if resistance >20%, recent usage • Symptoms > 7 days • Diabetes or immunosuppression • Fosfomycin 3 gm PO x 2 • History of childhood UTI Gupta K. CID 2011 8
3/26/2013 Prevention of recurrent UTIs Question 6b: If this same patient • Prevent vaginal colonization w/ uropathogens presented with pyelonephritis what – Avoid spermicide would be the best regimen? – Intra-vaginal estrogen (post-menopausal) A. Ceftriaxone 1 gm IV q24 • Prevent growth of uropathogens in bladder B. Moxifloxacin 400 mg IV/PO q24 – Cranberry juice C. Nitrofurantoin 100 mg PO q12 – Methenamine hippurate D. Cefpodoxime 200 mg PO q12 – Postcoitol or daily antibiotics • Correct anatomic/neurologic problems – Select cases consider urology evaluation (elevated Cr, hematuria, recurrent proteus infection) Case 7 Empiric treatment of pyelonephritis • Recommended • 60 y/o woman with HTN presents with 3 days – Ciprofloxacin 500 mg q12 (7 days if uncomplicated) of cough with green sputum, dyspnea on • Levofloxacin OK but not Moxifloxacin exertion, fever, pleuritic chest pain. She • Exam: 38.5 ° , 145/90, 100, 18, 95% RA – Ceftriaxone 1 gm IV q24 (14 days) otherwise has no past medical history. • Not recommended – TMP-SMX (high resistance rate so not good empiric) • • Chest: crackles at left base – Nitrofurantoin (does not get into kidney parenchyma) • WBC: 15.5 CXR: LLL infiltrate • Health-care associated pyelonephritis – Use antipseudomonal agent other than fluoroquinolone 9
Recommend
More recommend