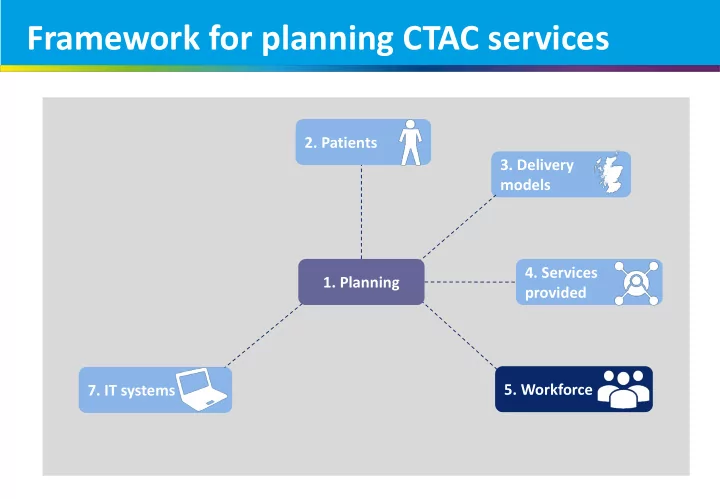
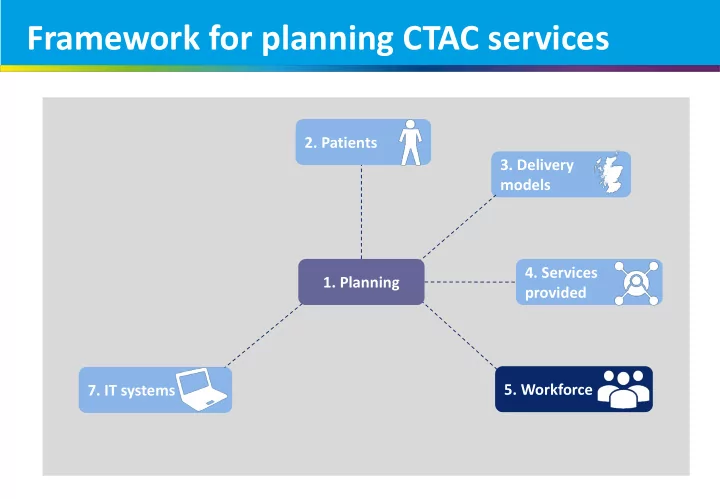
Framework for planning CTAC services 2. Patients 3. Delivery models 4. Services 1. Planning provided 5. Workforce 7. IT systems
#ctacQI 5. Workforce Jenny Wilson Assistant Director of Quality Improvement, NHS Ayrshire & Arran Nursing Clinical Lead for CTAC Services, ihub
Jennifer Wilson Assistant Director of Quality Improvement
WORKFORCE
Six Step methodology
Principles for Integrated Community Teams Principles for the Workforce A senior clinician, capable of Small self-organising, Health and care professionals making decisions about the geographical-based teams . working in partnership correct course of action, is available to patients as early in the process as possible Professional autonomy Primary care is delivered by a multidisciplinary team in which full use is made of all the team members, and the form of the clinical encounter is tailored to the need of the patient Primary care has professional and expert management, leadership and organisational support Primary care practitioners have immediate access to common Nuka diagnostics, guided by clinical eligibility criteria Canterbury Health System House of Care Neighbourhood care principles Nuffield Trust and Kings fund
Principles for Integrated Community Teams Principles for the People Building relationships with people to Putting the person at the centre of Services should enable people to take make informed decisions about their holistic care more responsibility for their own own care, which promotes wellbeing health and wellbeing and independence with active T ogether with the customer-owner as involvement of family, neighbours and an active partner the wider community, where Engaged, informed individuals and appropriate carers Care for frail people with multi- morbidity is tailored to the individual R elationships between the customer- Where possible, patients are supported needs of patients in this group, in owner, the family, and provider must to identify their own goals and manage particular people in residential or be fostered and supported their own condition and care nursing homes People should stay well in their own H ub of the system is the family Organisational and clinical processes homes and communities as far as structured around the person possible I nterests of the customer-owner drive E mphasis on wellness of the whole the system to determine what we do person, family and community and how we do it including physical, mental, emotional, and spiritual wellness.
Principles for Integrated Community Teams Principles for the System Everyone, including Patients are offered continuity of relationship S ervices are financially sustainable and viable support functions, where this is important, and access at the right enabling person- time when it is required centred care at the point of delivery. N ot complicated but simple and easy to use There is a single electronic patient record that is accessible by relevant organisations and can be read and, perhaps in future added to, by the P opulation-based systems and services patient I nternational whole system design to maximize coordination and minimize duplication Commissioning O utcome and process measures to continuously evaluate and improve Primary care organisations make information about the quality and outcomes of care publicly available in real-time When complex care is required it should be Patients have the minimum number of separate timely and appropriate visits and consultations that are necessary, with access to specialist advice in appropriate locations Patients can benefit from access to primary care A ccess is optimised and waiting times are limited advice and support that is underpinned by systematic use of the latest electronic L ocations that are convenient for the customer- communications technology owner and create minimal stops for the customer-owner
Model of Integrated Teams in Scotland Enabling Population Access Based Leadership Integrated Senior Clinician teams Person - centred Coproduced Professional Autonomy
5. Workforce Key points • Workforce is one of the key enablers for delivering the GMS contract. However, Resources concerns about the workforce issues were raised in the majority of our interviews. • See the CNO Transforming Nursing, Workforce planning Midwifery and Health Professions • Workforce planning for CTAC services is paramount to determine the staffing levels (NMaHP) roles papers here. required for CTAC delivery. • There needs to be an understanding of the demand, current workforce and their roles . Requirements for admin support should not be overlooked. Recruitment issues, not enough staff to go • 4 out of the 6 priority areas of the contract involve nursing staff. A joined approach round, taking staff from every area (this will should be considered. result in) major workforce issues • Concerns were raised about recruitment and the risk of destabilising the workforce across the system. We will all be fighting for the same people • There is an opportunity to share and learn how workforce planning is being approached by different areas. We are already doing stuff that is expected of these PN of the future but can’t necessarily prove qualifications Right skill mix • The right skill mix for delivering CTAC services should be defined. Decision makers CTAC need to be staffed by people competent to need to be part of the skill mix. Many areas are considering a mixture of nursing bands fulfil the role (competency based) rather than role and healthcare assistants to staff the services. based (task orientated) so staff can holistically treat • Concerns were raised around CTAC services being task based rather than viewing the patient rather than just fulfil tasks. patients holistically and therefore potentially de-skilling nurses . On the other hand, there were also concerns about not having the ‘right skills ’ for CTAC services. CTAC will provide a better career pathway for • At the same time, CTAC services could enable development opportunities and a career current treatment room nurses with better opportunities to progress and more access to pathway , which would make recruitment for these posts more attractive. training.
5. Workforce Key points Clinical governance How do you get the balance: robust central • Regardless of the model chosen to deliver CTAC services, clear governance structures governance and clarity of service provision but and appropriate clinical decision making should be ensured. with a level of devolved responsibility? • Appropriate skills and processes should be available to escalate issues when required. Change management / staff engagement People are moving on because of uncertainty. Nobody knows what’s happening and that breeds • The human side of change can be hard to navigate and having difficult conversations unrest may be required. Some of the already established CTAC services mentioned that from conception of the idea to fruition took much longer than expected and generated My job will be completely more opposition than they anticipated. taken away if CTAC services are running • Uncertainty around change is normal but should be managed properly to prevent unintended consequences (for example early retirement). These are some examples of what could be done to ease the transition: staff engagement and involvement Vital to provide training and helpline and re-training if necessary. Convince clear communication of shared vision and plans them what they are going to do is not visible and supportive leadership, and going to take up any more time providing additional capacity. • The philosophy of the contract is to free up practice capacity so that they can focus on Team is very visible so people are used to the management of chronic diseases. However, some expressed concerns that GPs seeing them and communication is open may reduce the staff employed within practices . Transfer of staff • Examples Some practice staff might need to have their employment transferred ( TUPE*) to the Health Board. This can be challenging both technically and emotionally. However, TUPE See here for examples of what people are could also bring new opportunities, including career development opportunities. doing to manage change. • There is an opportunity to share and learn how teams are addressing TUPE. * TUPE refers to the "Transfer of Undertakings (Protection of Employment) Regulations 2006”
How are you approaching workforce planning ?
Recommend
More recommend