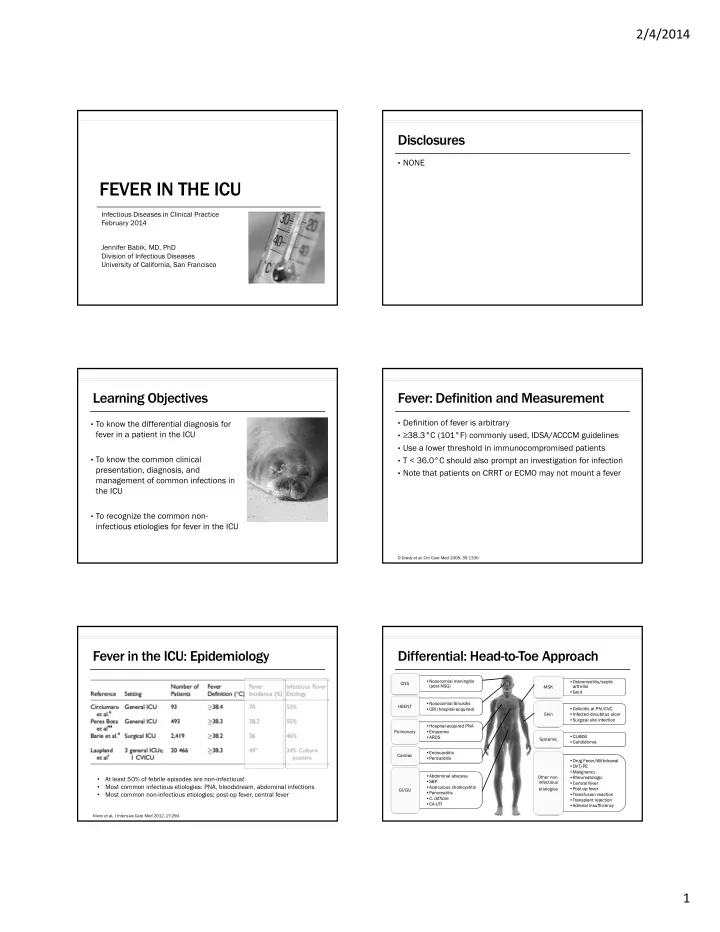
2/4/2014 Disclosures • NONE FEVER IN THE ICU Infectious Diseases in Clinical Practice February 2014 Jennifer Babik, MD, PhD Division of Infectious Diseases University of California, San Francisco Learning Objectives Fever: Definition and Measurement • Definition of fever is arbitrary • To know the differential diagnosis for fever in a patient in the ICU • ≥ 38.3°C (101°F) commonly used, IDSA/ACCCM guidelines • Use a lower threshold in immunocompromised patients • To know the common clinical • T < 36.0°C should also prompt an investigation for infection presentation, diagnosis, and • Note that patients on CRRT or ECMO may not mount a fever management of common infections in the ICU • To recognize the common non- infectious etiologies for fever in the ICU O’Grady et al, Crit Care Med 2008, 35:1330. Fever in the ICU: Epidemiology Differential: Head-to-Toe Approach •Nosocomial meningitis •Nosocomial meningitis •Osteomyelitis/septic •Osteomyelitis/septic CNS (post-NSG) (post-NSG) MSK arthritis arthritis •Gout •Gout •Nosocomial Sinusitis •Nosocomial Sinusitis HEENT •Cellulitis at PIV/CVC •Cellulitis at PIV/CVC •URI (hospital-acquired) •URI (hospital-acquired) Skin •Infected decubitus ulcer •Infected decubitus ulcer •Surgical site infection •Surgical site infection •Hospital-acquired PNA •Hospital-acquired PNA Pulmonary •Empyema •Empyema •CLABSI •CLABSI •ARDS •ARDS Systemic •Candidemia •Candidemia •Endocarditis •Endocarditis Cardiac •Pericarditis •Pericarditis •Drug Fever/Withdrawal •Drug Fever/Withdrawal •DVT/PE •DVT/PE •Malignancy •Malignancy •Abdominal abscess •Abdominal abscess At least 50% of febrile episodes are non-infectious! Other non- •Rheumatologic •Rheumatologic • •SBP •SBP infectious •Central fever •Central fever Most common infectious etiologies: PNA, bloodstream, abdominal infections • •Acalculous cholecystitis •Acalculous cholecystitis etiologies •Post-op fever •Post-op fever GI/GU •Pancreatitis •Pancreatitis Most common non-infectious etiologies: post-op fever, central fever •Transfusion reaction •Transfusion reaction • • C. difficile • C. difficile •Transplant rejection •Transplant rejection •CA-UTI •CA-UTI •Adrenal insufficiency •Adrenal insufficiency Niven et al, J Intensive Care Med 2012, 27:290. 1
2/4/2014 Differential: Head-to-Toe Approach Parts of the Exam to Remember •Nosocomial meningitis •Nosocomial meningitis •Osteomyelitis/septic •Osteomyelitis/septic CNS (post-NSG) (post-NSG) MSK arthritis arthritis MSK •Back and joint exam •Back and joint exam CNS •Careful neuro exam •Careful neuro exam •Gout •Gout •Nosocomial Sinusitis •Nosocomial Sinusitis HEENT •URI (hospital-acquired) •URI (hospital-acquired) •Cellulitis at PIV/CVC •Cellulitis at PIV/CVC •Examine line sites •Examine line sites Skin •Infected decubitus ulcer •Infected decubitus ulcer •Take off bandages •Take off bandages HEENT •Look for nasal discharge •Look for nasal discharge •Surgical site infection •Surgical site infection Skin •Peri-anal exam •Peri-anal exam •Hospital-acquired PNA •Hospital-acquired PNA •Look for (drug) rashes •Look for (drug) rashes Pulmonary •Empyema •Empyema •ARDS •ARDS •CLABSI •CLABSI Systemic •Candidemia •Candidemia •Endocarditis •Endocarditis Cardiac •Pericarditis •Pericarditis •Drug Fever/Withdrawal •Drug Fever/Withdrawal •DVT/PE •DVT/PE •Malignancy •Malignancy •Abdominal abscess •Abdominal abscess Other non- •Rheumatologic •Rheumatologic •SBP •SBP infectious •Central fever •Central fever •Acalculous cholecystitis •Acalculous cholecystitis etiologies •Post-op fever •Post-op fever GI/GU •Pancreatitis •Pancreatitis •Transfusion reaction •Transfusion reaction • C. difficile • C. difficile •Transplant rejection •Transplant rejection •CA-UTI •CA-UTI •Adrenal insufficiency •Adrenal insufficiency Diagnostics Case #1 • Avoid “automatic” order sets for fever (i.e. the “pan-culture”) 35 y/o man with alcoholic cirrhosis is admitted to the ICU with severe influenza A and is intubated and eventually requires • Expensive ECMO. He was slowly improving but then over the last 2 days • Time-consuming has starting having fevers to 38.3 with increasing O2 • Patient discomfort requirement. He has trouble following commands when • Unnecessary radiation sedation is lifted. • Transfer out of the controlled unit for imaging/procedures • With more testing, you will find more colonizers/contaminants Blood and urine cultures are negative. CXR is unchanged. • Use a rational approach Head CT shows pansinusitis but is otherwise negative. • Start with a history and physical • Order labs/diagnostics based on clinical suspicion O’Grady et al, Crit Care Med 2008, 35:1330. Your Next Diagnostic Step is: Defining CAP, HAP, VAP, HCAP 1. Sinus puncture Community- acquired pneumonia (CAP) 2. Lumbar puncture PNA not acquired in association with a healthcare setting (i.e. not meeting criteria 3. Mini-BAL or endotracheal aspirate for HAP or HCAP) IDSA/ATS Guidelines, Am J Resp Crit Care Med 2005. 2
2/4/2014 Defining CAP, HAP, VAP, HCAP Defining CAP, HAP, VAP, HCAP Community- Hospital-acquired Community- Hospital-acquired Ventilator-associated acquired pneumonia (HAP) acquired pneumonia (HAP) pneumonia (VAP) pneumonia (CAP) pneumonia (CAP) PNA not acquired in PNA acquired after 48 PNA not acquired in PNA acquired after 48 PNA acquired after 48 association with a hours in the hospital and association with a hours in the hospital and hours of intubation. This healthcare setting (i.e. not incubating at the time healthcare setting (i.e. not incubating at the time is a subset of HAP. not meeting criteria of admission. not meeting criteria of admission. for HAP or HCAP) for HAP or HCAP) Risk for MDR pathogens Risk for MDR pathogens Risk by days intubated: when hospitalized for ≥ 5 when hospitalized for ≥ 5 • Days 1-5 (3%/d) days. days. Days 5-10 (2%/d) • Days > 10 (1 %/d) • IDSA/ATS Guidelines, Am J Resp Crit Care Med 2005. IDSA/ATS Guidelines, Am J Resp Crit Care Med 2005. Defining CAP, HAP, VAP, HCAP Why do we care about these distinctions? • To characterize the risk of MDR bacteria, and therefore Community- Hospital-acquired Ventilator-associated Healthcare-associated acquired pneumonia (HAP) pneumonia (VAP) pneumonia (HCAP) inform your empiric antibiotic approach pneumonia (CAP) PNA not acquired in PNA acquired after 48 PNA acquired after 48 PNA in a non-hospitalized association with a hours in the hospital and hours of intubation. This patient with any one of the • Risk of MDR organisms in PNA: healthcare setting (i.e. not incubating at the time is a subset of HAP. following: not meeting criteria of admission. Hospitalization for ≥ 2 days - • HCAP for HAP or HCAP) in the last 90 days • HAP/VAP with ≥ 5 days in the hospital - Residence in a nursing Risk for MDR pathogens Risk by days intubated: home or long-term care • Immunosuppression when hospitalized for ≥ 5 Days 1-5 (3%/d) facility • days. Days 5-10 (2%/d) Intravenous antibiotics, • - • Abx in last 90 days Days > 10 (1 %/d) wound care, dialysis, or • chemotherapy within the • High frequency of ABx resistance in a specific unit last 30d Family member with an - MDR pathogen IDSA/ATS Guidelines, Am J Resp Crit Care Med 2005. IDSA/ATS Guidelines, Am J Resp Crit Care Med 2005. VAP: Diagnosis VAP: Diagnosis ST STEP 1 1 STEP 2 ST 2 STEP 3 ST 3 • Other diagnostics : Clinical suspicion for PNA? Lower respiratory tract culture • Start empiric therapy • Sensitivity of blood cultures before ABx <25% (1) New or progressive CXR infiltrate • Quantitative cultures preferred + • Thoracentesis if an effusion • Re-evaluate each day based on • BAL (cutoff 10 4 or 10 5 ) and (2) 2 out of 3 clinical criteria: culture results, clinical course is large or the patient is toxic mini-BAL (cutoff 10 3 or 10 4 ) • F > 38 ˚ C both are ~80% sensitive and • or WBC specific • Consider stopping ABx if • Purulent secretions • Even 24 hrs of prior ABx can cultures are negative make a sample negative • 69% sensitive, 75% specific • With ARDS: consider PNA when have 1 clinical criteria b/c may not see CXR changes IDSA/ATS Guidelines, Am J Resp Crit Care Med 2005. Klompas, JAMA 2007, 297:1583. IDSA/ATS Guidelines, Am J Resp Crit Care Med 2005. Raman, Crit Care Med 2013, 41:0, 3
Recommend
More recommend