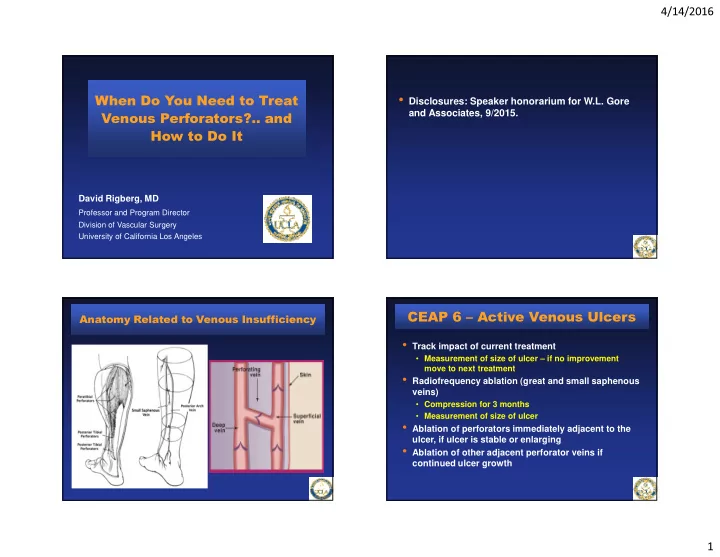
4/14/2016 • Disclosures: Speaker honorarium for W.L. Gore When Do You Need to Treat and Associates, 9/2015. Venous Perforators?.. and How to Do It David Rigberg, MD Professor and Program Director Division of Vascular Surgery University of California Los Angeles CEAP 6 – Active Venous Ulcers Anatomy Related to Venous Insufficiency • Track impact of current treatment • Measurement of size of ulcer – if no improvement move to next treatment • Radiofrequency ablation (great and small saphenous veins) • Compression for 3 months • Measurement of size of ulcer • Ablation of perforators immediately adjacent to the ulcer, if ulcer is stable or enlarging • Ablation of other adjacent perforator veins if continued ulcer growth 1
4/14/2016 Duplex Ultrasound Evaluation Duplex Ultrasound Evaluation • Reversed Trendelenberg position on an electronic tilt table • A GE Logiq-e portable duplex scanner used for imaging • The incompetent vein adjacent to the ulcer with both reflux and a diameter above 3 mm selected for Rx Duplex Ultrasound Evaluation Duplex Ultrasound Evaluation • RFS catheter placed at a 45°angle – transverse and longitudinal • Leg dressed with compression transducer dressing • Confirm stylet in vein at fascia • Confirmation of closure of the • Inject local anesthetic to eliminate vein at next clinic visit (48-72 pain hours postop) • • Independent vascular lab Trendelenberg position technician • Vein treated with RF energy for 1 minute in each quadrant; repeated • Repeat procedure if incompletely above the fascia if possible closed • Confirmation of ablation due to compression from local anesthetic 2
4/14/2016 Process of Perforator Closure There Is A Learning Curve! Perforator Closure Success Rate 80% 70% 60% 50% 40% success rate 30% 20% 10% 0% 2007 2008 2009 2010 Learning curve of a Single Vascular Surgeon 80% 70% 60% 50% success 40% rate 30% 20% 10% 0% 2007 2008 2009 2010 J Vasc Surg 2011;54(3):737-742 Method of Tracking Ulcer Healing Choosing the Right Modality for Perforator Ablation Vein Ablation Procedure 16.00 Mean Success Rate 14.00 12.00 • Ultrasound guided Ulcer Size (cm^2) 10.00 Ulcer growth = foam sclerotherapy +2.66 cm 2 /mo 8.00 (UGFS) = 65% Ulcer closure = 6.00 -6.08 cm 2 /mo • Radiofrequency = 83% 4.00 2.00 • Laser = 75% 0.00 0.00 0.10 0.20 0.30 0.40 0.50 0.60 • SEPS = 87% Time (Years) Green: Treatment with compression therapy alone Orange: Ongoing compression after vein ablation *Studies in last 5 years Current State of the Treatment of Perforating Veins. JVS 2015. 3
4/14/2016 Perforator Ablation for Venous Ulcers - RCT Impact of Perforator Ablation on Ulcer Healing Rates Ablation Procedures Ulcer Locations • Mean ulcer healing = 81% • Mean ulcer recurrence = 10% Current State of the Treatment of Perforating Veins. JVS 2015. In-Press J Vasc Surg 2012;55:458-464 Results – Change in Ulcer Healing Rate Ulcer Healing Rate by Specific Vein Ablation Variable Pre-ablation healing Post-ablation P-value (cm 2 /mo) ± ± ± SEM ± (cm 2 /mo) ± ± ± ± SEM rate healing rate Healed + 1.02 ± .11 - 4.45 ± .13 Healed Ulcers Ulcers ALL VEINS <.001 N = 84 + 1.18 ± .12 - 6.44 ± .17 Axial + 1.06 ± .13 - 4.82 ± .14 GSV <.001 SSV <.001 + .89 ± .09 - 2.92 ± .10 Perforators PTV <.001 Unhealed Ulcers + .96 ± .07 - 4.60 ± .11 + 1.09 ± .08 - 6.26 ± .16 ALL VEINS <.001 Healing Ulcers + .99 ± .10 - 4.57 ± .11 GSV <.001 N = 26 + .80 ± .06 - 2.79 ± .06 SSV <.001 PTV <.001 4
4/14/2016 Conclusions • Perforator ablation is difficult and takes practice • Venous ulcers can all be healed with an aggressive approach to incompetent superficial axial veins, perforating veins, and occasionally correction on deep venous obstruction and/or reflux • The status of the ulcer is the key to determining if there is “ambulatory venous hypertension” • If an ulcer in not healing with optimal compression or heals and then recurs, there is a mechanical reason – we find it and treat it! 5
Recommend
More recommend