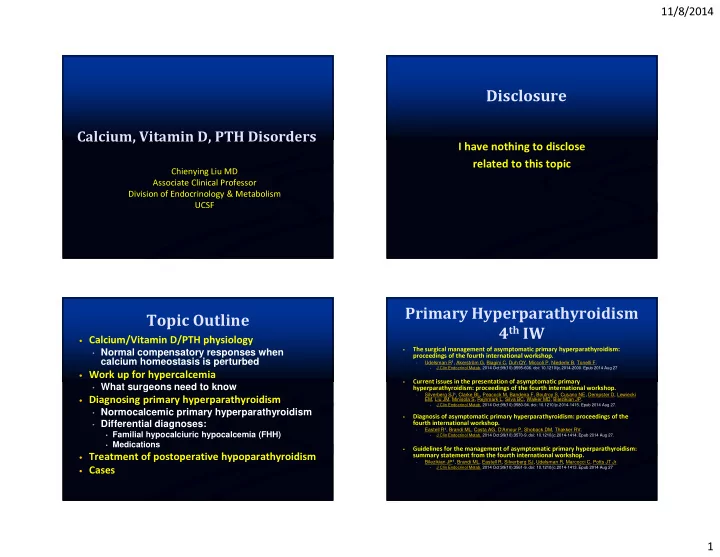
11/8/2014 Disclosure Calcium, Vitamin D, PTH Disorders I have nothing to disclose related to this topic Chienying Liu MD Associate Clinical Professor Division of Endocrinology & Metabolism UCSF Primary Hyperparathyroidism Topic Outline 4 th IW • Calcium/Vitamin D/PTH physiology • Normal compensatory responses when The surgical management of asymptomatic primary hyperparathyroidism: • proceedings of the fourth international workshop. calcium homeostasis is perturbed Udelsman R 1 , Akerström G, Biagini C, Duh QY, Miccoli P, Niederle B, Tonelli F. • J Clin Endocrinol Metab. 2014 Oct;99(10):3595-606. doi: 10.1210/jc.2014-2000. Epub 2014 Aug 27 • • Work up for hypercalcemia Current issues in the presentation of asymptomatic primary • • What surgeons need to know hyperparathyroidism: proceedings of the fourth international workshop. Silverberg SJ 1 , Clarke BL, Peacock M, Bandeira F, Boutroy S, Cusano NE, Dempster D, Lewiecki • EM, Liu JM, Minisola S, Rejnmark L, Silva BC, Walker MD, Bilezikian JP. • Diagnosing primary hyperparathyroidism J Clin Endocrinol Metab. 2014 Oct;99(10):3580-94. doi: 10.1210/jc.2014-1415. Epub 2014 Aug 27. • • Normocalcemic primary hyperparathyroidism Diagnosis of asymptomatic primary hyperparathyroidism: proceedings of the • • Differential diagnoses: fourth international workshop. Eastell R 1 , Brandi ML, Costa AG, D'Amour P, Shoback DM, Thakker RV. • • Familial hypocalciuric hypocalcemia (FHH) J Clin Endocrinol Metab. 2014 Oct;99(10):3570-9. doi: 10.1210/jc.2014-1414. Epub 2014 Aug 27. • • Medications Guidelines for the management of asymptomatic primary hyperparathyroidism: • summary statement from the fourth international workshop. • Treatment of postoperative hypoparathyroidism Bilezikian JP 1 , Brandi ML, Eastell R, Silverberg SJ, Udelsman R, Marcocci C, Potts JT Jr • J Clin Endocrinol Metab. 2014 Oct;99(10):3561-9. doi: 10.1210/jc.2014-1413. Epub 2014 Aug 27 • • Cases 1
11/8/2014 PTH & Calcium Role of Vitamin D & Calcium Normal Physiology Modified from Holick JCI 2006 PTH secretion • Regulated by ica ++ • in the blood (major regulator) Response within • seconds to minutes 25 OHD – vitamin D store • ½ life 2 weeks • Correlates with secondary • Others: Active calcium absorption – D dependent hyperparathyroidism • Mg ++ 1, 25 D – Most active form 2- • PO 4 • Not typically measured • 1, 25(OH)D when assessing for D def • 1 α hydroxylase enzyme – tightly regulated Chen & Goodman 2004 Defining Vitamin D Sufficiency PTH, Vitamin D, Calcium Modified from Holick JCI 2006 Endocrine Society Guidelines PTH: direct renal effects • Sufficiency: > 30 ng/ml *↑Ca reabsorption PTH: direct bone effect *↑Phos excretion 32 ug/mL indirect bone effect • Insufficiency: 20 - 30 ng/ml * ↑ 1 α hydroxylase • Deficiency : < 20 ng/ml PTH: indirect GI effect • Institute of Medicine ↑Ca/Phos absorption 290 consecutive pts via 1,25 D • Sufficiency: ≥ 20ng/mL on a general medical ward MGH • Insufficiency: 10-20 ng/mL • Deficiency: < 10 ng/mL 2
11/8/2014 Secondary Summary of PTH Effects Calcium sensing receptor Hyperparathyroidism • Major effects • Directly: bone and kidney • Indirectly: small intestine • Bone • Mobilizes calcium from bone • Diseased forms of hyper-secretion: bone resorption -> osteopenia/osteoporosis (cortical bone more affected than trabecular bone) • Kidney 1 alpha hydroxylase • ↑ 1, 25 vit D production (up-regulates 1 alpha hydroxylase) • ↑ calcium reabsorption Serum Calcium • ↑ phosphate excretion • Small Intestine • ↑ calcium/phosphate absorption (via Kidney : ↑ 1, 25 vit D production) Modified from Stubbs et al. Seminars in Dialysis 20, 2007. Hyperparathyroidism Secondary Hyperparathyroidism • Primary • Vitamin D related • Renal Leak Hypercalciuria • Parathyroid adenoma or hyperplasia Sun/Diet deprivation ‒ ‒ ↑↑ 24 hr urine calcium • Rarely carcinoma Malabsorption (fat) ‒ ‒ Small bowel, pancreatic, hepatic biliary diseases • Medications • Secondary ‒ Celiac disease • Compensatory mechanism to restore normal (Anticonvulsants, HAART, steroids) Medica�ons ↑ metabolism ‒ ‒ ‒ Anticonvulsants, HAART, ionized calcium level Bisphosphonates, denosumab steroids ‒ • Normal or low normal or low calcium, with Lithium ‒ elevated PTH • Impaired Absorption GI disorders ‒ • Tertiary ‒ calcium and/or vitamin D • Other causes malabsorption • Usually due to longstanding chronic kidney Hungry bone syndrome ‒ Aging, corticosteroid treatment disease, on dialysis ‒ Pseudo-hypoparathyroidism ‒ • Parathyroid hyperplasia → autonomous Resistance to PTH (bone and/or • Chronic Kidney Disease ‒ production → ↑ calcium and PTH kidney) ↓1,25 (OH) D, hyperphosphatemia ‒ High PTH, low Ca ++ /high PO 4 2- ‒ 3
11/8/2014 Primary Hyperparathyroidism Hypercalcemia Biochemical Profiles PTH unmeasurable PTH measurable Simultatenously measured PTHrp malignancy • Primary • Calcium PTH Presentation ↑1.25(OH) D from granulomatous • hyperparathyroidism disease or leukemia ↑ ↑ Classic/usual • Familial hypocalciuric ↑ 25(OH) D from vitamin D toxicity • Milk alkali syndrome (excessive hypercalcemia • calcium intake with renal ↑ Normal (inappr) Also PHPT • Medications insufficiency) (Inappropriate PTH ( intermi�ently ↑) (intermi�ently ↑) • Lithium and Thiazide Immobilization • when hypercalcemic) Vitamin A toxicity • • Rare malignancy Theophylline toxicity Normal ↑ Normocalcemic • making PTH Endocrine causes • PHPT Hyperthyroidism • • Tertiary Acute adrenal insufficiency • hyperparathyroidism Pheochromocytoma • Acromegaly • Primary Hyperparathyroidism(PHPT) Evaluation • PTH, Calcium, albumin, phosphate, Cr/GFR (alkaline phosphatase) • Albumin corrected calcium: calcium (in mg/dL) + (0.8x (4-albumin in g/dL) • Ionized calcium Reliable lab • Helpful if ↑ albumin, paraproteinemia, perturbed acid/base patients, making serum calcium less reliable • 4-10% patients may have normal serum Surgery 2012; 152:635-42 calcium but elevated ionized calcium in PHPT 4
11/8/2014 Familial Hypocalciuric Hypercalcemia ( FHH) PHPT- Evaluation • PTH inappropriately • Autosomal dominant • Measuring 25 (OH)vitamin D in all patients with PHPT • Inactivating mutations normal or mildly elevated – recommended by 3 rd & 4 th IW in the CaSR gene 80%: PTH normal/ ↑ calcium • • Vitamin D deficiency may worsen clinical picture 20%: PTH mildly ↑/ ↑ calcium • • Relative • Normalizing vitamin D lowers PTH hyposensitivity to • Relative low urine calcium calcium level excretion • Correct vitamin D deficiency prior to definitive • Normal or low urine • Lifelong hypercalcemia decision on management of PHPT calcium (<100mg) (Also important for definitive diagnosis of PHPT ) • Surgery is NOT indicated • Low calcium to • Localization studies can creatinine clearance • Maintain vitamin D > 20ng/mL (3 rd & 4 th IW) be misleading ratio (<0.01) • Higher vitamin D threshold may lower PTH further • Asymmetry in the size of the glands in FHH Work with Your Endocrinologist Eastell et al JCEM 2014 IW=International Workshop Christensen, et al PHPT vs FHH Clinical Endocrinology PHPT - Evaluation (2008) 69 , 713–720 • 54 patients with FHH & 97 patients with PHPT Stopped calcium, diuretics(thiazide/loop) for • Look for prior Ca levels • Assess urine calcium excretion 3-6 days. Excluded patients on lithium Nl → PHPT • To differentiate Familial Hypocalciuric Hypercalcemia • Significant overlap in urine calcium excretion • 24 hour urine calcium excretion or CCC ratio 3 rd and 4 th IW CCC ratio best diagnostic value • < 0.01 → FHH >0.02: 65% PHPT and 2% FHH. If < 0.02, • Calcium to creatinine clearance ratio (CCC ratio) • > 0.02 → PHPT genetic studies • PHPT typically higher CCC > 0.02, > 90% likelihood of PHPT Genetic studies in-between • FHH typically low CCC < 0.01, >95% likelihood of FHH • Vitamin D replete – important to interpreter the result Uca U-Ca X S-creat S-Ca X U-creat Ucr 1mmol = 40mg Sca Scr 400mg Overlap Spot or timed urine collections Simultaneous urine/serum measurements 250mg 0.01 100mg Eastell et al JCEM 2014 5
Recommend
More recommend