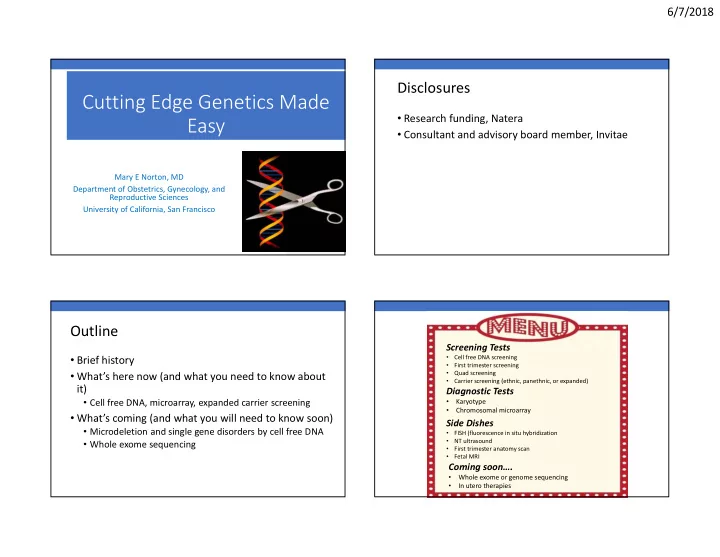
6/7/2018 Disclosures Cutting Edge Genetics Made • Research funding, Natera Easy • Consultant and advisory board member, Invitae Mary E Norton, MD Department of Obstetrics, Gynecology, and Reproductive Sciences University of California, San Francisco Outline Screening Tests • Brief history • Cell free DNA screening • First trimester screening • What’s here now (and what you need to know about • Quad screening • Carrier screening (ethnic, panethnic, or expanded) it) Diagnostic Tests • Cell free DNA, microarray, expanded carrier screening • Karyotype • Chromosomal microarray • What’s coming (and what you will need to know soon) Side Dishes • Microdeletion and single gene disorders by cell free DNA • FISH (fluorescence in situ hybridization • NT ultrasound • Whole exome sequencing • First trimester anatomy scan • Fetal MRI Coming soon…. • Whole exome or genome sequencing • In utero therapies 1
6/7/2018 Detection rate of prenatal screening for Down syndrome has improved over time The history of 120 prenatal 100 Detection Rate (%) diagnosis is 80 focused largely 60 on Down 40 syndrome 20 0 Age >35 Triple Quad First Integrated cfDNA screen screen trimester screen screen Lejeune, 1959 Tijo and Levan, Newborn vs prenatal screening 1956 Disorder is important test is developed and introduced Technology is developed test is introduced 2
6/7/2018 1997 cfDNA screening for T21: meta-analysis cfDNA screening for T21: meta-analysis ( Gil et al, Ultrasound Obstet Gynecol, 2017) ( Gil et al, Ultrasound Obstet Gynecol, 2015 Detection Rate: 99.7% False Positive Rate: 1/2500 DR: 99.2% (98.5 - 99.6) FPR: 0.09% (0.05 - 0.14) DOWN SYNDROME!! 3
6/7/2018 Spectrum of Congenital Disease Which of the following conditions are NOT detected by a chromosomal microarray? Conditions • 1/300 Autosomal recessive found by pregnancies 55% Autosomal dominant A. Down syndrome • 20% of infant microarray X-linked deaths B. 22q microdeletion syndrome Copy number Chromosomal/ karyotype C. Klinefelter syndrome variants Half of these are 16% D. Hemophilia 14% Down syndrome 8% 7% E. What is a chromosomal microarray? a e e e m m i m l . i . o o h . o p c r r r d d o m i d n n n m y y y l s e a s s H m n n r w e o o Structural Malformations t s o t i l o e D e f m l e e n o d i r o l h K r c c i a m s i q t 2 a 2 h W Microdeletions are detected by Microdeletions are genomic imbalances chromosomal microarrays (CMA) detected by microarray but not karyotype • “Lab-on-a-chip” • Detects thousands of microdeletions and duplications at the same time • Have largely replaced karyotype in pediatrics Miller et al, 2010, AJHG 4
6/7/2018 Chromosomal Microarray (CMA) Russell Silver syndrome: Small, asymmetric for Prenatal Diagnosis Mild learning disabilities Ch 7 Prader-Willi : Hypotonia, significant Ch 15 learning disabilities, obesity Indication for Testing Clinically Relevant (N=96) Angelman syndrome : Some Microdeletion U/S Anomaly ( N=755) 6.0% Severe intellectual Syndromes disability and speech AMA ( N=1,966) 1.7% impairment Positive Screen ( N=729) 1.7% Ch 5 Cri du chat syndrome : Other ( N=372) 1.3% Poor feeding and growth, microcephaly, severe learning difficulties Rate of abnormalities by maternal age (Microarray abnormalities) • “In patients with fetal structural abnormalities undergoing prenatal diagnosis, microarray is recommended.” • Microarray should be available to all pregnant women. • Patient acceptance limited by concern about uncertain findings , fear of diagnostic testing, and lack of adequate insurance coverage Increasing maternal age 5
6/7/2018 Abnormalities found by microarray Chromosomal microarray: bottom line • Diagnostic testing with chromosomal microarray is the best test for pregnant women who want as much information as possible about their fetus. 1-6% • Women should be counseled about the chance of finding a variant of uncertain significance • Cell free DNA can detect only a tiny number of the total microdeletions Availability of Genetic Tests Ethnicity Based Carrier Screening Most of these are for inherited disorders Ashkenazi Jews Tay Sachs disease, Canavan disease, cystic fibrosis, familial dysautonomia Louisiana Cajun, Tay Sachs disease Fr Canadian Caucasians Cystic fibrosis Africans, African Sickle cell anemia, beta Americans thalassemia Southeast Asians Alpha thalassemia Mediterraneans Beta thalassemia 6
6/7/2018 Traditional Carrier Screening Multiplex Panel Screening: Universal (Expanded) Carrier Screening • Focus on ancestry and family history • Small number of diseases • High frequency in a certain subpopulation • Multiplex screening now allows carrier testing for many • Severe morbidity or mortality (hundreds) disorders at once • Fetal, neonatal or early childhood onset • Well-defined phenotype • This is relatively inexpensive ($100-350) • Should it be recommended for everyone? Sickle Cell Tay-Sachs disease What is on expanded panels and how are disorders chosen? Disorders should be: What criteria are required by laboratories • Severe before including gene variants on panels? • Common • Have a well-described natural history and phenotype • Have a high detection rate 7
6/7/2018 Expanded Carrier Screening: The Wild West • Evaluated commercially available panels • 27% of included disorders meet criteria per ACMG and ACOG ACOG 2017 Updated Screening ACOG 2017 Updated Screening Recommendations Recommendations • Screening should be offered to all women before or during • Fragile X screening should be offered to all women with: pregnancy for: • a family history of FraX related disorders • Cystic fibrosis • unexplained ovarian insufficiency or failure • Spinal muscular atrophy • Tay Sachs screening should be offered to those who are: • MCV should be offered to all women who are currently • French Canadian pregnant • Cajun • Ashkenazi Jewish • To those at risk for hemoglobinopathies , Hb electrophoresis should be offered (African, Mediterranean, Middle Eastern, SE Asian, West Indian) or if MCV is low 8
6/7/2018 Is expanded carrier screening The Question: accurate? Molecular DNA testing is not the recommended screening approach for certain conditions • Tay-Sachs disease • Hexosaminidase A enzyme analysis is best test for non- Jewish individuals • Hemoglobinopathies • Gold standard is MCV and hemoglobin electrophoresis • Carrier screening platforms do not include all mutations for alpha and beta thalassemia The Answer: Not always!! How Often Do Tests Find Something? 9
6/7/2018 What Then? A real patient story • Patient reports that she carries SMA 24-45% will have something • Partner has expanded carrier screening through panel covered 1. Explain to the patient by his insurance • Carries Fanconi Anemia, group A 2. Test the partner (he might not have insurance) • Patient undergoes expanded carrier screening with panel 3. He will often be a carrier for something else covered by her insurance 4. If low detection rate on original panel, do • She carries Pompe disease but was not tested for Fanconi group A, just group C (updated panel) gene sequencing • They are frustrated and seek a second opinion 5. Explain all this to the patient • He undergoes gene sequencing for this condition • All he really needed was testing for SMA 10
6/7/2018 What should you do? Non-Invasive Single Gene Tests It is acceptable to offer either: • Maternal and fetal cell free DNA cannot be easily 1. Ethnicity based screening distinguished 2. Pan ethnic screening (offer everyone CF, SMA, and assess MCV, regardless of ancestry) • However, can identify de novo or paternal gene mutation 3. Expanded carrier screening • Offer everyone the same thing • This includes blood type if mother is Rh negative and fetus is • Consider creating a custom panel Rh positive 37 yo G1P0 at 27 wks 11
6/7/2018 • N=47 cases • Correct in 46 (96.2%) • Useful tool in 3 rd trimester to distinguish IUGR from achondroplasia Chitty LS, et al. Prenat Diagn 35:656, 2015 • De novo mutations • Many associated with advanced paternal age • No prospective data on performance • Not ready for routine use 12
6/7/2018 What is the future? Whole Genome and Whole Exome Sequencing • Whole Genome Sequencing • Obtaining the complete sequence of all 3 billion base pairs of DNA in any individual • Whole Exome Sequencing • Obtaining the complete sequence of the ~2% of the genome containing the exons that encode proteins What is whole exome sequencing? A genome is like watching the game An exome is like reading the from beginning to end highlights whole exome sequencing (WES), is a genomic technique for sequencing all of the protein- coding genes in a genome (known as the exome ). 13
6/7/2018 The future: Noninvasive whole genome sequencing? What is “CRISPR”? What is “CRISPR”? • Clustered • Regularly • Interspaced • Short • Palindromic • Repeats 14
Recommend
More recommend