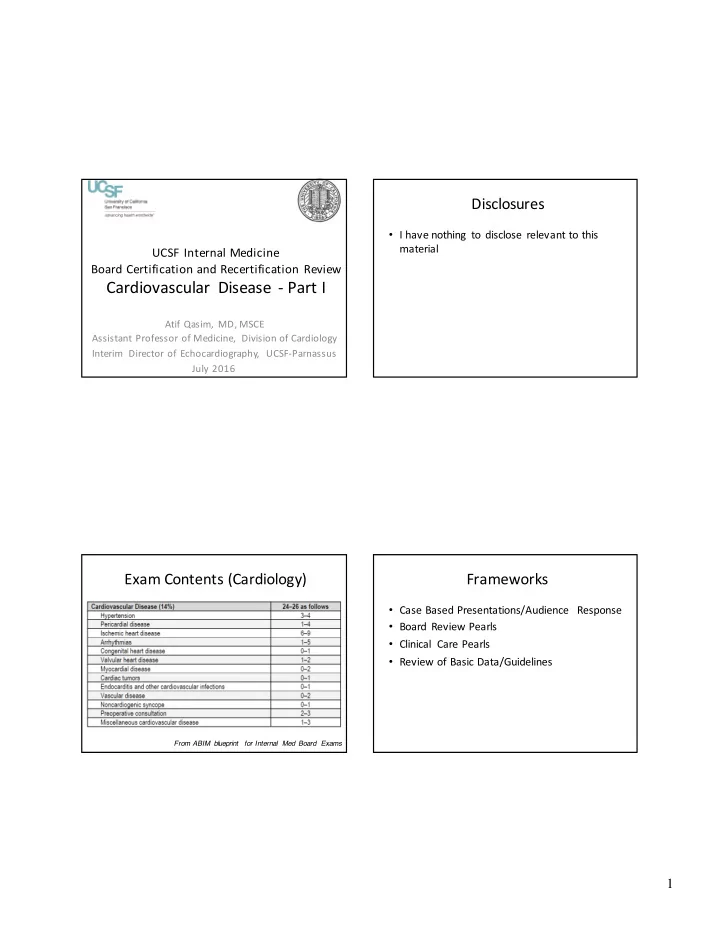
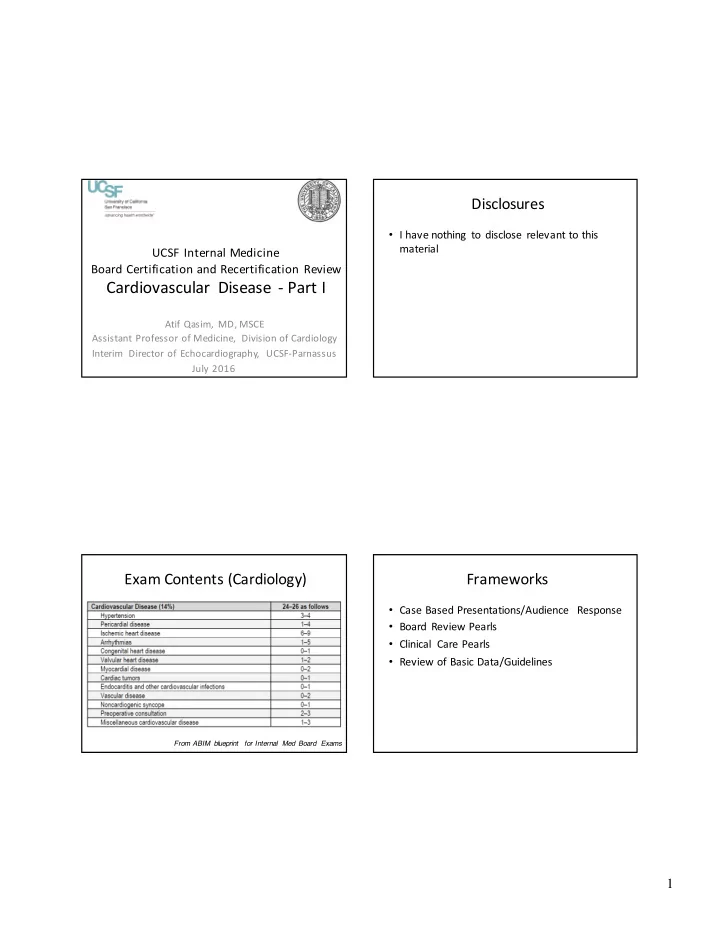
Disclosures • I have nothing to disclose relevant to this material UCSF Internal Medicine Board Certification and Recertification Review Cardiovascular Disease - Part I Atif Qasim, MD, MSCE Assistant Professor of Medicine, Division of Cardiology Interim Director of Echocardiography, UCSF-Parnassus July 2016 Exam Contents (Cardiology) Frameworks • Case Based Presentations/Audience Response • Board Review Pearls • Clinical Care Pearls • Review of Basic Data/Guidelines From ABIM blueprint for Internal Med Board Exams 1
Cardiac Exam Pearls Modern Medicine and the Heart 1. Blood pressure: – Severe Hypertension (e.g. 220/110) à think aortic dissection • Chest pain? Short of breath? – Large pulse pressure with low diastolic (e.g. 180/50) à think aortic regurgitation – EKG 2. Carotids: – Labs (BNP, troponin) – Weak and slow (a.k.a. parvus et tardus ) à think aortic stenosis – Bifid (double peak) pulse à think HOCM – Chest X-Ray 3. JVP: – CT scan – Large V wave à tricuspid regurgitation – Echo – Rapid Y descent à constriction 4. PMI – Stress T esting - Laterally displaced à a dilated heart, systolic heart failure – Cardiac Cath - Sustained, non displaced à a thick heart, diastolic heart failure Cardiac Exam Pearls (2) Cardiac Exam Pearls (3) 1. First heart sound ( closure of mitral and tricuspid valves ) : Murmurs: Soft S1 à think mitral (or tricuspid) regurgitation – Location, location, location A P Loud S1 à think mitral stenosis – Location and timing in cardiac T 2. Second heart sound (closure of aortic and pulmonic valves) : M cycle will tell you the cause Physiologically split i.e. split only during inspiration à norma l – Fixed splitting à think ASD – Holosystolic – MR, TR, VSD Loud P2 à think pulmonary hypertension – – Soft A2 (or Single S2) à Severe Aortic stenosis. Ejection – AS, PS, HCM Mid to late systolic –MVP with MR 3. S3 à think volume overload, dilated heart Rare* non-valvular murmurs: 4. S4 à think pressure overload, thick heart Continuous “machinery” think patent ductus arteriosus (PDA) 2
Dynamic Maneuvers HOCM and Valsalva Maneuver Effect Reason Inspiration Augments right-sided Due to increased venous murmurs filling of right heart Valsalva AugmentsHOCM murmur . Increases intrathoracic Makes MVP (mitral valve pressure, compresses LV prolapse) click earlier and reducing LV volume. longer associated MR Reduces preload and murmur . LVEDP Squatting MakesHOCM murmur Increases arterial softer, MVP click later, all resistance, venous return other murmurs louder . (preload) and stroke volume and chamber size Rapid standing Opposite of squatting Opposite of squatting Image courtesy of www.studyblue.c om Cardiac Examination Pearls (4) MVP and Valsalva • There are often clues in the history!!!! – Young patients à think congenital heart disease – Old patients à think degenerative valve disease – Foreign patients à think rheumatic heart disease – Post-MI à think mechanical complications (VSD or mitral regurgitation) – Cancer patients à think about pericardial Valsalva disease, chemo related cardiomyopathy From O'Rourke RA, Crawford MH. The systolic click-murmur syndrome: clinical recognition and management. Curr Probl Cardiol 1976;1:1–60 . 3
Approach to Tachycardia Approach to ECGs for the boards • Rate, rhythm, axis Irregular = AFIB Narrow = • P-Q-R-S-T conducts via normal Regular or pathways (i.e. irregular? Check P-waves: • P= atrial depolarization supraventricular Regular = 1. normal = in origin) Sinus Sinus tach , QRS • PR = AV conduction tach, A 2. sawtooth = narrow Flutter or Aflutter , or wide SVT 3. none or • QRS = ventricular Wide = abnormal = SVT ventricular origin VT or SVT depolarization or conducts via with abnormal aberrancy • T = ventricular pathway repolarization Approach to Bradycardia Approach to Cases Really only 3 things it is likely to be on this exam: • Read the question first • Sinus bradycardia • Heart block (AV nodal block) – I will present this way • Slow Afib • Figure out what question type So ask yourself: – which diagnostic test 1. Are there P waves? – management decision – If no, it is probably Afib 2. Is every P wave followed by a QRS complex? – you make the diagnosis – If yes, sinus brady • Read vignette with question in mind, highlight st or 2 nd degree heart block If no, complete heart block >> 1 – any clues. Exam pearl: Examiners like to stop meds – may need to stop beta-blockers 4
Case 1: 22 year old man with Case 1: What is the next best test? exertional syncope A. T readmill Exercise ECG Stress Presented to ER after an episode of sudden loss of consciousness immediately after a 3 mile jog. He B. Cardiac Event monitor awoke completely after 3-4 minutes. Denied chest pain, shortness of breath or palpitations. C. Dobutamine stress echocardiography • FH: positive for sudden death in a cousin D. T ransthoracic echocardiogram E. Serial troponin I levels and EKGs • PMH: Uncomplicated rotator cuff repair • PE: HR =60, BP = 90/60, JVP = 6 cm, S4 gallop, no murmur. Lungs clear. No edema. Case 1: EKG Case 1: What is the next best test? A. T readmill Exercise ECG Stress B. Cardiac Event monitor C. Dobutamine stress echocardiography D. T ransthoracic echocardiogram E. Serial troponin I levels and EKGs 5
Case 1: EKG Review Case 1: What is the next best test? A. T readmill Exercise ECG Stress B. Cardiac Event monitor C. Dobutamine stress echocardiography D. Transthoracic echocardiogram E. Serial troponin I levels and EKGs Case 1: Educational Objectives Overall Causes of Syncope – Know the causes and recommended evaluation • Cardiac: 18% for syncope • Neurologic: 10% • Vasovagal: 24% – Recognize the symptoms and signs of hypertrophic cardiomyopathy • Orthostatic: 8% • Medications: 3% – Know the risk factors for sudden death in a patie nt • Unknown: 37% with hypertrophic cardiomyopathy 6
Cardiac Syncope Syncope Evaluation • Structural causes • Arrhythmic causes • Careful history and physical examination crucial in work-up of syncope – Common – Bradycardia – Reveals probable cause in 50% of patients • AS - usually exertional • Sinus bradycardia • Hypertrophic obstructive – Vasovagalsyncope is strongly suggested by characteristic • AV block cardiomyopathy - often prodrome and may be confirmed by Tilt table test • Carotid sinus post-exercise or due to hypersensitivity • EKG arrhythmias – Tachycardia – Less common • Echo indicated with h/o heart disease, abnormal exam or • SVT (rare) abnormal EKG or elderly • PE, dissection, tamponade • VT – Uncommon • Holter or event monitor • Tilt Table • Pulmonary HTN, atrial myxoma Exertional syncope often ominous Hypertrophic Cardiomyopathy(HCM) • Differential diagnosis: • Autosomal dominant inheritance pattern with – Obstruction to left ventricular outflow (aortic stenosis an d variable penetrance. 1/500 incidence. hypertrophic cardiomyopathy [HOCM]) • Usually presents in adolescent or young adult – Ventricular tachycardia but can present at any age – Pulmonary hypertension • Triad of symptoms: – Neurocardiogenic syncope • T readmill Exercise ECG Stress T esting should be Chest pain, Dyspnea and Syncope delayed until structural causes excluded 7
HCM: Physical Examination HCM (cont’d) • EKG: L VH with repolarization abnormalities • Non-obstructive: S4, sustained apical impulse • Echocardiogram: • Classic: Left ventricular hypertrophy with septal >>posterior wa ll • Obstructive: thickness (asymmetric septal hypertrophy) • Obstruction: associated with systolic anterior motion (SAM) of • Bisferiens carotid pulse (“spike and dome”) the mitral valve. Sometimes there is associated MR. • Double or Triple apical impulse • Pharmacologic treatment • Systolic murmur that increases with standing or strain phase of • Beta-blocker Valsalva and decreases with passive leg raising or squatting, • Calcium channel blocker (Verapamil, Diltiazem) increases post-PVC • Avoid any vasodilator or positive inotropic agent (Dobutamine • Dynamic obstruction: echocardiography relatively contraindicated) • Occasionally may hear murmur only with maneuver • Avoid dehydration • See obstruction only with exercise HOCM and systolic anterior motion HCM: Other Treatment • Avoid high intensity sports • Surgical myomectomy or alcohol septal ablation in obstructive form only in pts refractory to med Rx • ICD for those at high risk for sudden death if : • Prior cardiac arrest • One or more family members with sudden death caused by HCM, • Syncope otherwise unexplained, especially if related to physical activity, occurs repeatedly, or appears in young people. • Ventricular tachycardia on Holter monitor • Blood pressure fails to rise during exercise testing, esp if younger than 50 years. • Extreme thickness of LV septum (30 mm or more) on echo. 8
Recommend
More recommend