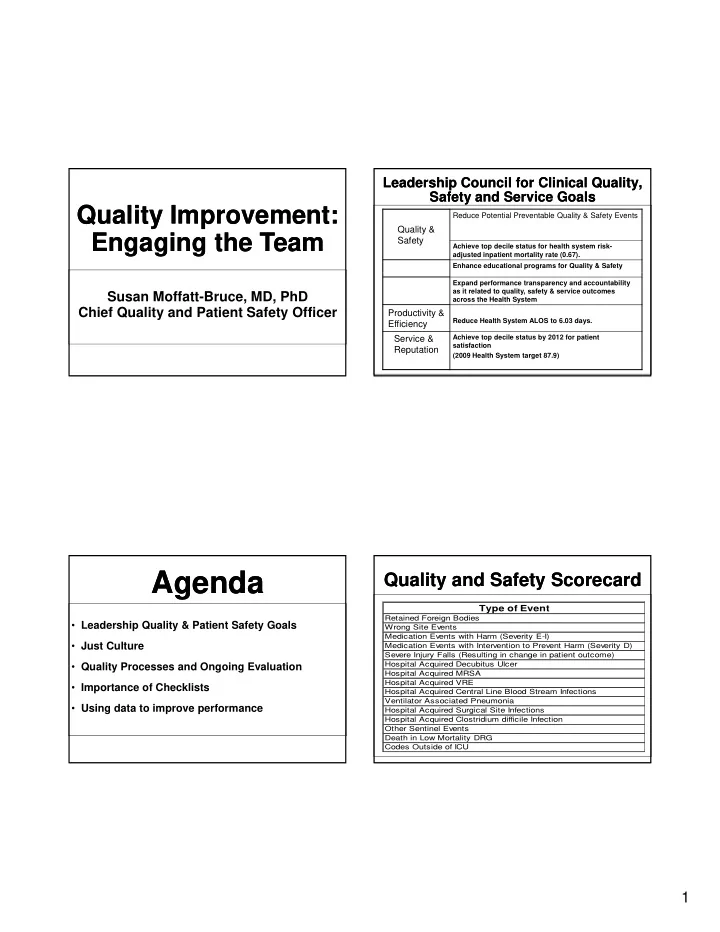
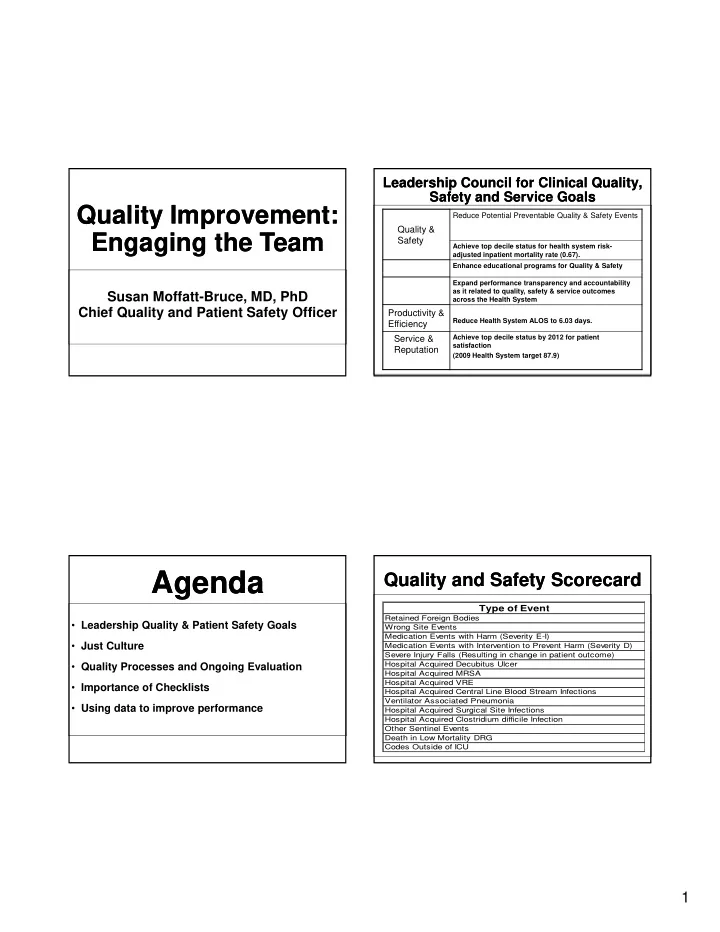
Leadership Council for Clinical Quality, Leadership Council for Clinical Quality, Safety and Service Goals Safety and Service Goals Quality Improvement: Quality Improvement: Reduce Potential Preventable Quality & Safety Events Quality & Engaging the Team Engaging the Team Safety Achieve top decile status for health system risk- adjusted inpatient mortality rate (0.67). Enhance educational programs for Quality & Safety Expand performance transparency and accountability as it related to quality, safety & service outcomes Susan Moffatt-Bruce, MD, PhD across the Health System Chief Quality and Patient Safety Officer Productivity & Reduce Health System ALOS to 6.03 days. Efficiency Service & Achieve top decile status by 2012 for patient satisfaction Reputation (2009 Health System target 87.9) Agenda Agenda Quality and Safety Scorecard Quality and Safety Scorecard Type of Event Retained Foreign Bodies • Leadership Quality & Patient Safety Goals Wrong Site Events Medication Events with Harm (Severity E-I) • Just Culture Medication Events with Intervention to Prevent Harm (Severity D) Severe Injury Falls (Resulting in change in patient outcome) • Quality Processes and Ongoing Evaluation Hospital Acquired Decubitus Ulcer Hospital Acquired MRSA Hospital Acquired VRE • Importance of Checklists Hospital Acquired Central Line Blood Stream Infections Ventilator Associated Pneumonia • Using data to improve performance Hospital Acquired Surgical Site Infections Hospital Acquired Clostridium difficile Infection Other Sentinel Events Death in Low Mortality DRG Codes Outside of ICU 1
Just Culture Just Culture Accountability Accountability To guide organizations when making fair decisions, “ Just Culture ” – Balance system and process decision algorithms have been developed. These issues with accountability for expected behaviors algorithms typically ask a series of questions: • The just culture is not a blame-free culture. It • Were the actions intended? merely tries to provide a consistent guide to merely tries to provide a consistent guide to • Was the person under the influence of unauthorized determine: substances? 1) When a person is truly at fault for a specific act • Did the person knowingly violate existing policies, 2) Reasonable consequences that will best serve procedures, or expectations? the individual’s and the organization’s interests • Would another person in the same situation perform in the same manner? • Does this person have a history of unsafe acts? Just Culture Just Culture The four key categories of fault in a just culture are: • Human error: Unintended slips, lapses, and mistakes • Negligent conduct: Failure to exercise care expected of a prudent worker • Reckless conduct: Conscious disregard for a known risk • Knowing violations: conscious disregard for known rules Reason, J: Managing the Risk of Organizational Accidents 2
Practitioner Performance Practitioner Performance Quality Processes and Quality Processes and Evaluation Evaluation Ongoing Review Ongoing Review • To evaluate the competency and professional performance of an • Partnership between individual practitioner � Department Chairs � Quality Department � Initial applicant -FPPE � Credentialing Department � New privilege request-FPPE � Chief Quality and Patient Safety Officer � Concern has been identified-FPPE � Chief Medical Officer � Ongoing basis-OPPE Physician Executive Council Role (PEC) Quality Review Process Quality Review Processes Practitioner Performance Practitioner Performance 1. Review determinations from prior levels of review, including OPPE & FPPE OPPE (Profile) 2. Obtain additional clinical expertise from Global/SSI outlier internal/external physician or trends 3. Notify practitioner of any preliminary Evaluation Evaluation issues/concerns & request input prior to final disposition Morbidity & Triggers for Mortality 4. Final disposition to DMA/CMO as appropriate further review 1 Review outcome (s) • Six core competencies that were PEC Chair notifies Practitioner notified PEC Chair Dept Chair, Case reviewed Mortality Review reviews that case going at PEC originally developed for the Graduate (single egregious or trends in high to PEC severity outcome) Medical Education: PEC Potential Recommendations Insurance/ Managed Care Quality Notice No action – 1) Patient care continue OPPE Dept Chair – Event Report process process ( i (single egregious l i improvement [sentinel] 2) Medical knowledge or trends) plan Dept Chair – observation No Requires Professionalism Notify practitioner & 3) Practice-based learning and Council Dept Chair – recommendation Close case Dept. Chair proctoring to CMO/ of findings DMA/Chair? Committee for improvement FPPE (new privilege/ LIHP Health new practitioner) indicator outlier Yes or trends Dept Chair – 4) Interpersonal and communication simulation Professionalism CMO initiates formal Dept Chair Council peer review process referral as outlined in Bylaws skills Engage 5) Systems-based practice Terry Zang, RN DMA/CMO 1 Trigger cases follow determined processes & Quality & Operations 06.11.10 are peer reviewed prior to forwarding to Chief Contact: Susan Moffatt-Bruce Quality & Pt. Safety Officer 3
FPPE – Initial Privilege FPPE – Initial Privilege FPPE – For Cause FPPE – For Cause (New Applicant) (New Applicant) • Appropriate when questions arise regarding a • Initial privilege request – new Applicant currently privileged practitioner’s ability to provide safe, high quality patient care • Requires evidence of competency in 10 clinical • Triggers include but are not limited to: encounters (outpatient or inpatient; office visit) � Event Reporting trends or single egregious case • Initial period of FPPE is 6 months (provisional � Patient/Family complaint period) � Referral from the Department Chair • Must be pertinent to the privileges requested � Unprofessional behavior • Evidence is reviewed by the Chief Quality & � Outliers identified in FPPE for applicant or privilege Safety Officer and Credentials Committee prior to � Outliers identified during OPPE moving to full active appointment Ongoing Practitioner Ongoing Practitioner FPPE – New Privilege FPPE – New Privilege Performance Evaluation Performance Evaluation • Current members of the medical staff or licensed • Biannual evaluation of each Department member with the healthcare professional staff with specifically Department Chair delineated clinical privileges who are requesting • Aligns with reappointment and data are used to a new privilege will be granted the new privilege determine: on a Provisional basis. on a Provisional basis � Maintenance of privileges � Modification of privileges • The review criteria may vary, but the review must be specifically relevant to the privilege granted � Termination of privileges • Global indicators (mortality, LOS, readmission) • Evidence is reviewed by the Chief Quality & Safety Officer and Credentials Committee prior to • Service-specific indicators as approved by the Division approving new privilege and Department • Low volume faculty- 23 / 2 years 4
Recommend
More recommend