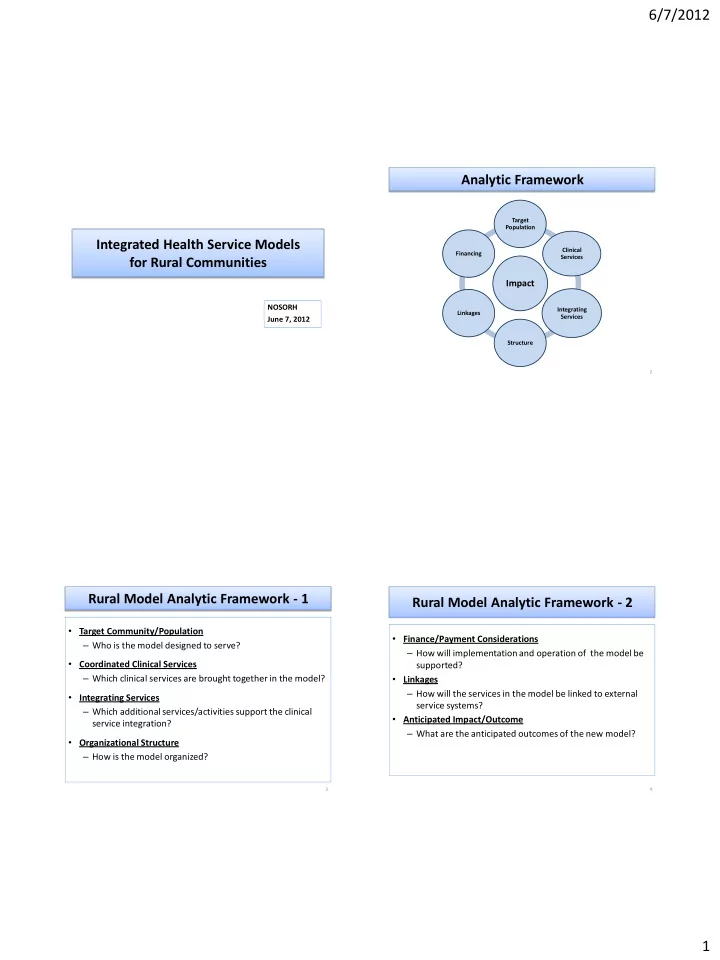
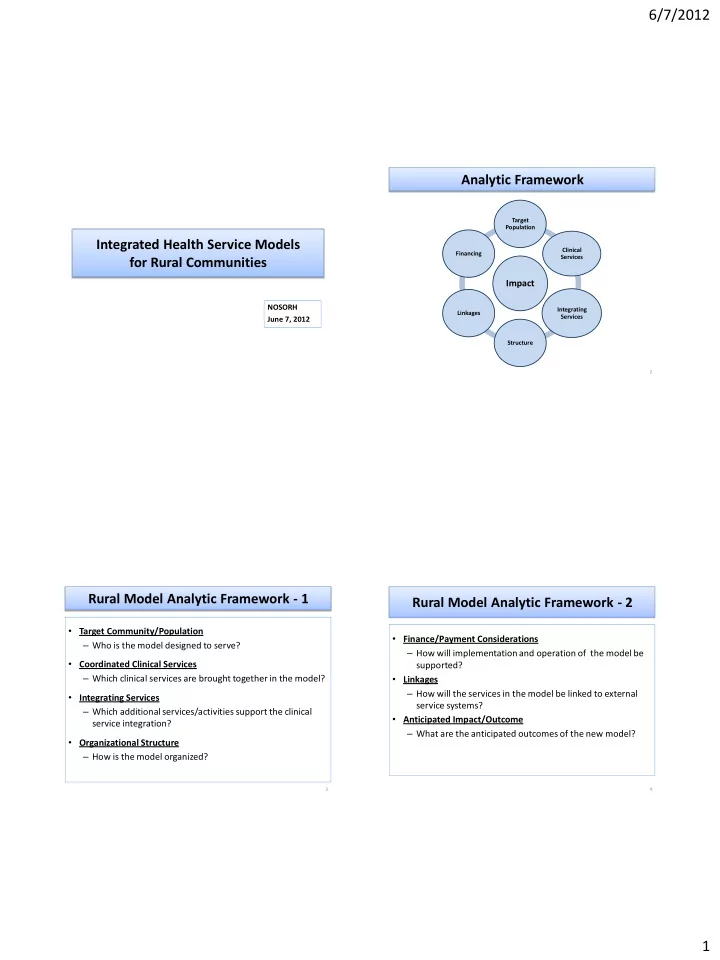
6/7/2012 Analytic Framework Target Population Integrated Health Service Models Clinical Financing Services for Rural Communities Impact NOSORH Integrating Linkages Services June 7, 2012 Structure 2 Rural Model Analytic Framework - 1 Rural Model Analytic Framework - 2 • Target Community/Population • Finance/Payment Considerations – Who is the model designed to serve? – How will implementation and operation of the model be • Coordinated Clinical Services supported? – Which clinical services are brought together in the model? • Linkages – How will the services in the model be linked to external • Integrating Services service systems? – Which additional services/activities support the clinical • Anticipated Impact/Outcome service integration? – What are the anticipated outcomes of the new model? • Organizational Structure – How is the model organized? 3 4 1
6/7/2012 Health Reform Impacts Models Examined • Health Service • Frontier Health System Model (MT, WY, AK,ND) – Improve health service effectiveness. – A CAH-based integrated service model. – Improve health service quality. • Hidalgo Plan Model (NM) • Health Status – A primary care/public health centered integrated service – Improve patient health. model. – Improve population health. • Coordinated Care Organization Model (OR) • Health Utilization – A more general purpose integrated service model. – Improve health service access. – Reduce inappropriate health care use. – Reduce unnecessary health care expenditures. 5 6 Frontier Health System Model (FHS) FHS: Clinical Services • Background/Overview • Clinical care services aggregated into the new Frontier Health System include: – The Frontier Health System model is an outgrowth of the Frontier Community Health Integration Demonstration Program . – Hospital-based services (new CAH 35 bed limit) – The Demonstration program was authorized by the Medicare • Hospital inpatient Improvements to Patients and Providers Act ( MIPPA ), and expanded • Hospital swing beds by the Patient Protection and Affordable Care Act ( PPACA ) • Hospital outpatient – The Model is the basis of a Medicare demonstration program that • hospital ER (at a Level IV Trauma center certification) would create a new Medicare classification and conditions of – Ambulance services participation for networks of health services in certain eligible – Expanded rural health clinic services communities in four states ( MT, AK, ND, WY ). – Home health services – Extended care – Each network would be centered around a Critical Access Hospital • Visiting nurse services that may provide and include additional health services. – physical, occupational or speech therapy in the frontier – A separate Medicare reimbursement mechanism would be patient’s home established for the integrated services of the participating network. • Home hospice services – Prevention services 7 8 2
6/7/2012 FHS: Integrating Services FHS: Financing and Reimbursement • Integrating Services included in the FHS model: • Financial Support for FHS operations will come from several – Clinical Care Coordination: Patient-centered medical home for the sources : coordination and delivery of services to Medicare patients: – Medicare cost-based reimbursement for integrated • Preventive services • Primary care, services. This will be a new mechanism. • Extended care (including Visiting Nurse Services (VNS) with – Payment incentives for quality improvement therapies), – Shared savings with CMS for cost/utilization reduction • Long term care • Specialty care. – Financing is anticipated to be largely budget-neutral . – Transition Management: Management of patient transition between • Most included services are currently cost-based. care providers. – Chronic Care Management : Monitoring and treatment of patients • Some additional services will pay for themselves with chronic conditions, including services to the homebound. through savings. – Practice Quality Improvement: Pay for Outcome (P4O). 9 10 FHS: Anticipated Outcomes/Impact FHS: Target Population and Replicability • Key target outcome is reduction of Medicare payment • Target population per patien t – Medicare patients in eligible communities of 4 states. – Achieved through reduction of preventable events - unnecessary admissions and readmissions to – Isolated communities as small as 1,000 population. inpatient, ER and long term care settings. – Could be translated to other communities with – Additional savings from quality improvement. CAHS, both frontier and non-frontier. – Also achieved by improved clinical preventive • CMS would need to modify current rules to permit services. implementation: – All savings to be shared with FHS to help offset non- – Increase in CAH bed limit from 25 to 35 cost based services – similar to ACO model. – Include coverage of preventive and care management • Additional outcome - improved access to key services , services for reimbursement. including long term care and home health. – Modify several other conditions, including distance limits. 11 12 3
6/7/2012 Hidalgo Plan Model (HP) HP: Service Components - 1 • Clinical Services • Overview/Background – Primary Care – Developmental approach from a frontier community with • Medical no hospital and a single provider of primary care and • Oral Health public health services . • Behavioral Health – Seeks to implement an expanded coordination of – Preventive Care outpatient care for local residents with a public health – • Integrating Services health improvement effort . – Clinical care coordination – Also implements coordinated outreach and service to – Chronic care management high risk and chronic care patients . – High risk patient engagement/health improvement – Seeks multi-payer participation in model reimbursement , – Social support services emphasizing Medicaid and public health funding sources. 13 14 Center for HP: Service Components - 2 Health Innovation The Preferred Flow of Health Systems and Costs – Health Education Tertiary V Tertiary Care • Community education Sub- E Specialty R • Patient education – including self-care Current T PC Model I – Patient Communication Secondary and C A Subspecialty Care – Service Improvement L • Quality Integrated Primary Care C O • Effectiveness O R • Health Outcome D I N – Integrated Informatics A Community Engagement / Accountability T I Social Determinants O N Horizontal – Actual / Virtual Team Support 15 16 4
6/7/2012 HP: Service Intervention Alignment Interventions Based on Spectrum of Health Services – Broad Focus Virtual Face to Face • • Population / Community Level Prevention Community Prevention Engagement – – Mass Media Outreach Health Fairs – Promotion / Early ID – Public Information Campaigns – Access - Eligibility – Community Infrastructure – Nutrition Support – Economic Development • Viva NM, Grocery Store Tours / Label • Patient Population Communication Reading – Health Information / Reminders – Exercise Classes / Support Management w/ – Organizational Promotion • Diagnosis and Treatment Team Interventions – Social Media – Social / Behavioral Assessments • Categorical Patient Support – Clinical Preventive Services Diagnosis & – Condition Specific Information – One On One Support – Prescription Assist – Treatment Tele-Communications / Texting Cost/Complexity – – Self-Management and Referral Follow-up Email, Text Messages, Social Media Prevention % Population – • Patient Level Communication Non-Visit Contacts – Auto-Reminders / Scheduling • Care Management – Patient Portals – Care Coordination – Internal and External Referral Systems – Decision Support / Home Visits – Social Support 17 18 HP: Anticipated Outcomes/Impacts New Types of Health Professionals Clinical Support Staff Administrative Support Staff • Improved health status : • • Researchers and Evaluators Community Health Workers (Global) – General population – EMR Utilization to Support – Outreach – High risk sub-population Patient Care Priorities and – Community Health Program Development – Chronically ill. – Prevention Campaigns – Geographic Analyses • Improved care coordination: • Community Health Navigators – Move from Process Problems – General patient population (Horizontal) to Outcomes Improvements – Patient Support / Eligibility • Virtual Patient Systems – Patients with chronic disease Communicators – Education • Improved clinical practice – Community / Patient – Social Determinants Population Levels • Reduction of unnecessary service utilization • Care Coordinators (Vertical) – EMR Infrastructure Support • Reduction of service cost for target community • (MA) Patient Communication • UNM HEROs Specialists – Clinical Preventive – Resource Linking Services – Scheduling / Reminders 19 20 5
Recommend
More recommend