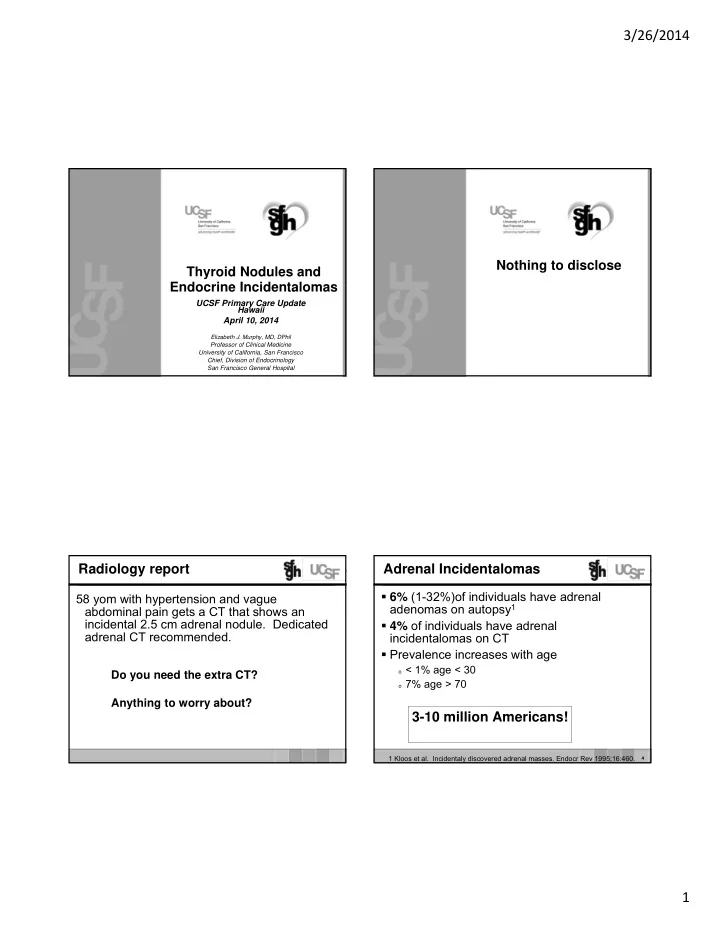
3/26/2014 Nothing to disclose Thyroid Nodules and Endocrine Incidentalomas UCSF Primary Care Update Hawaii April 10, 2014 Elizabeth J. Murphy, MD, DPhil Professor of Clinical Medicine University of California, San Francisco Chief, Division of Endocrinology San Francisco General Hospital Radiology report Adrenal Incidentalomas 6% (1-32%)of individuals have adrenal 58 yom with hypertension and vague adenomas on autopsy 1 abdominal pain gets a CT that shows an incidental 2.5 cm adrenal nodule. Dedicated 4% of individuals have adrenal adrenal CT recommended. incidentalomas on CT Prevalence increases with age o < 1% age < 30 Do you need the extra CT? o 7% age > 70 Anything to worry about? 3-10 million Americans! 1 Kloos et al. Incidentaly discovered adrenal masses. Endocr Rev 1995;16:460. 4 1
3/26/2014 Common Adrenal Masses Why Adrenal Specific CT 1. Thin cuts (2-3 mm) through the adrenals Adrenalocortical Adenoma 90+% which are quite small. Pheochromocytoma 5% 2. Determine pre contrast Hounsfield Units (HU) Adrenalocortical Carcinoma <5%? • HU < 10-15 very specific for benign adenoma Metastatic Lesion 2.5% 3. Determine % washout of contrast • Washout % > 60 is very specific for benign adenoma Incidence of carcinoma 3000/year Corresponding prevalence 1/1000 (0.1%) Prevalence really 5%? 5 Mansmann et al, Endocrine Reviews , 2004, 25:309-340) Adrenal Nodule – Imaging Concerning features o Hemorrhage, Calcification, Necrosis o no fat (high HU) Concerning size o > 4 cm : 70% malignant (excluding adrenal myelolipomas and pheochromocytomas) o > 6 cm : 85% malignant 7 8 2
3/26/2014 Radiology report What to do? 58 yom with hypertension and vague 1) Wish you hadn’t ordered the original CT in abdominal pain gets a CT that shows an the first place. incidental 2.5 cm adrenal nodule. Dedicated adrenal CT recommended. 2) Be thankful everything is good and tell the patient it’s nothing to worry about. 3) Wish you hadn’t gone to that CME course IMPRESSION: in Hawaii as now you know #2 isn’t correct 1.3 cm nodule in the left adrenal gland. This and you have more work ahead. has Hounsfield units and enhancement characteristics consistent with a benign adrenal adenoma. No additional follow-up is recommended. 10 Adrenal Gland - Hormones Adrenal Gland - Hormones Catacholamines (Medulla) Catacholamines (Medulla) o Pheochromocytoma o Pheochromocytoma Mineralocorticoids (aldosterone/glomerulosa) Mineralocorticoids (aldosterone/glomerulosa) o Aldosterone secreting adenoma o Aldosterone secreting adenoma 1+ %? o Adrenal hyperplasia o Adrenal hyperplasia o Adrenal carcinoma o Adrenal carcinoma Glucocorticoids (cortisol/fasiculata) Glucocorticoids (cortisol/fasiculata) o Adrenal adenoma o Adrenal adenoma 5- %? o Adrenal carcinoma o Adrenal carcinoma o Bilateral hyperplasia o Bilateral hyperplasia Androgens (DHEA/reticularis) Androgens (DHEA/reticularis) o Adrenal carcinoma o Adrenal carcinoma 3
3/26/2014 Common Adrenal Masses Hormonal Evaluation Everyone: Adrenalocortical Adenoma 90+% o Dexamethasone suppression test o Aldosterone secreting 1%? 1 mg dex at 11-MN night before with 8 am cortisol o Cortisol secreting 5%? • Cortisol > 5 mcg/dl is abnormal • Pheochromocytoma 5% o Fractionated urinary metanepharines and Adrenalocortical Carcinoma < 5%? catecholamines or plasma metanepharines Metastatic Lesion 2.5% If Hypertension o Hyperaldo screening test with morning plasma aldosterone and plasma renin activity Ratio > 20 AND aldo > 15 consider hyperaldo • 13 14 Endocrine Referral Primary Hyperaldosteronism - Etiologies 66 yow with DM2, HTN on a beta-blocker, HCTZ, and amlodipine. Got aldo and renin because K Steady rise in prevalence (5-10% of hypertensive was 3.4. Elevated ratio. Abdominal CT with 1.4 patients?) cm adenoma on left. Please assist in referral to Adrenal adenoma (75%) surgery. LABS usually very small tumors Aldo 4 treat/ cure with surgical resection PRA 0.1 Bilateral adrenal hyperplasia (25%) Aldo/PRA ratio: 40 H (nl < 20) treat medically with aldosterone antagonist (spironolactone or Patient with hypoaldo, hyporenin state due to eplerenone) Adrenal carcinoma (rare %) age and DM2. Ratio is high (low renin). Aldo very, very poor prognosis, more often secrete DOC, is not high. Now there is the need to w/u the mineralocorticoid excess least of concerns incidental nodule. 15 4
3/26/2014 Effect of Antihypertensives on Aldo-Renin Ratio Confirmatory Tests for Hyperaldo Confirmatory testing DIAGNOSING ENDOCRINE DISORDERS Screening test is elevated Aldo/ PRA ratio Discern a clinical syndrome 1. Confirmatory Tests Make the biochemical diagnosis of hormone excess 2. 24 hour urine aldosterone testing after a salt load or deficiency Saline suppression test 3. Determine the etiology of the hormone excess or Fludracortisone suppression test deficiency Captopril (ACE-I) challenge test Problems with Testing in Hypertensive Patients Consider appropriate imaging to localize the site of 4. Stopping BP meds pathology Massive salt loading Testing is really difficult… . Once confirmed need to consider need for adrenal vein sampling 5
3/26/2014 Adrenal Gland Biopsy Radiology report Per radiology recommendation you send the 58 yom with hypertension and vague abdominal pain patient to IR for FNA of the adrenal lesion. gets a CT that shows an incidental 2.5 cm adrenal You get called the day of the procedure by nodule. Dedicated adrenal CT recommended. radiology who tells you the patient coded and died during the procedure. You have to call IMPRESSION: the patient’s wife to explain what happened. Indeterminate 15 mm nodule in left adrenal gland. For further evaluation a biopsy is recommended if clinically indicated. What did happen??? What did happen??? (findings section: HU 32, washout 9%) 22 Pheochromocytoma/ Paraganglioma Adrenocortical Carcinoma Rule of 10s: 10% bilateral, 10% extra-adrenal, 10% Typically present with pain and are very large malignant, 10% genetic >25% genetic Invasive Associated Genetic Syndromes: Can secrete a lot of different hormones Multiple Endocrine Neoplasia 2 (RET) Cortisol Familial Paraganglioma Syndrome (SDHA, SDHB, SDHC, Deoxycorticosterone (mineralocorticoid) SDHD, SDHAF2) Androgens (Testosteron, Dehydroepiandrosterone (DHEA-S)) Von Hippel-Lindau Syndrome (VHL) Can have Cushings, huirsuitism, virulization Neurofibromatosis Type 1 (NF1) TMEM127 Very poor prognosis Pheo Crisis/ HTN Crisis/ Catecholamine Storm NEVER EVER (hardly ever) BIOPSY AN ADRENAL MASS 6
3/26/2014 Frequency of Follow-up Imaging for Benign Lesion (< 10 HU) Algorithm for adrenal incidnetalomas Never (one of many) Once in 6-12 months (may reassure the physician and the patient) At 6, 12, and 24 months Zieger et al, JCEM 96:2004-2015, 2011. ? Case Pituitary Incidentaloma 34 yow with worsening migraine HA and gets • Pituitary adenoma (50-90%) an MRI. She was noted to have an incidental 6 mm pituitary adenoma. What • Craniopharyngioma now? • Rathke’s cleft cyst • Other primary tumors in the pituitary • Metastases Pituitary Incidentaloma • 11% prevalence on autopsy data • 10% prevalence on MRI (10-38%) 27 7
3/26/2014 ANTERIOR PITUITARY PITUITARY GLAND: Sagittal View Testing for Hypofunction o History and exam o Laboratory testing if suspicion - test end- organ function as basal levels of pituitary hormones are often normal in hypopituitarism Testing for Hyperfunction o History and exam o Laboratory testing for everyone – often dynamic GH testing with suppression tests ADH ACTH TSH LH, FSH Prolactin Pituitary Hypofunction Pituitary Hyperfunction GH (rarely tested) Prolactin level (most common) o IGF-1 level IGF-1 o GH stimulation test (insulin induced hypoglycemia) Gonadotrophs (FSH/LH) o Low Testosterone level without elevated LH o Amenorrhea in a young woman or lack of FSH elevation in a post-menopausal woman ( estradiol not useful) TSH o good history and exam for hypothyroidism o Low f ree T4 level without elevated TSH ACTH o Cosyntropin (synthetic ACTH) stimulation test 8
3/26/2014 Pituitary Hyperfunction Pituitary Incidentaloma Prolactin level (most common) Microadenoma < 1 cm IGF-1 Macroadenoma ≥ 1 cm o VF testing if near abutting or compressing the Screening for glucocorticoid excess?? optic nervers or chiasm o Only if clinical suspician Follow-up imaging for non-secreting micro- o Dex suppression and not ACTH incidentaloma o Repeat MRI yearly for 3 years and then less frequently 34 Case Five things Physicians and Patients Should Question 29 yow comes to your office complaining of amenorrhea, anxiety, weight loss and tremors. You get a TSH which is < 0.01. You then order a thyroid US which shows a 1.2 mm hyperechoic nodule and diffuse increased vascularity. 36 9
Recommend
More recommend