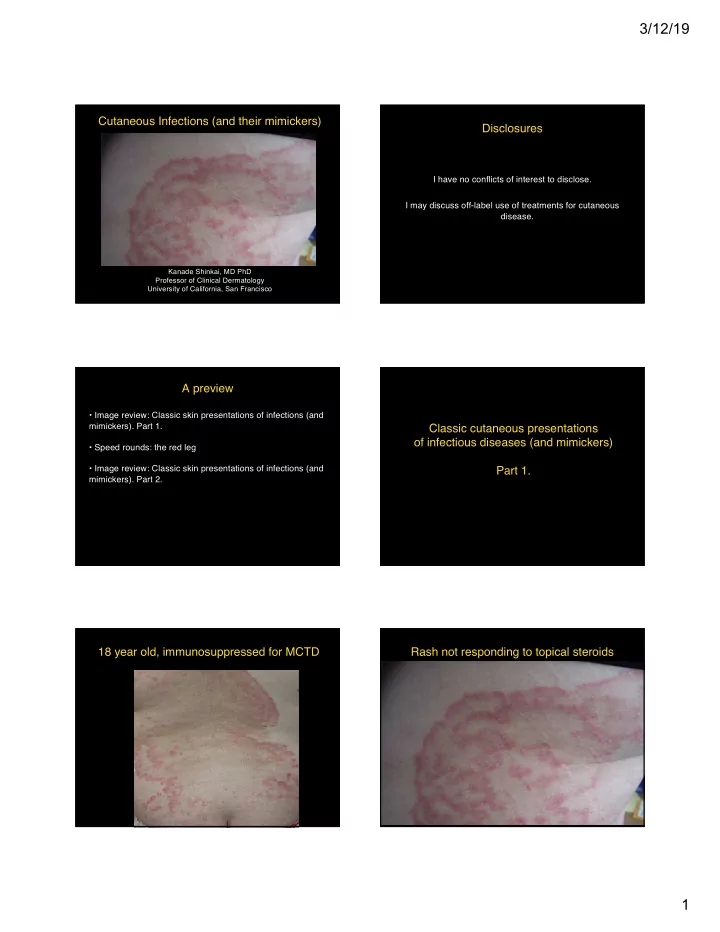
3/12/19 Cutaneous Infections (and their mimickers) Disclosures I have no conflicts of interest to disclose. I may discuss off-label use of treatments for cutaneous disease. Kanade Shinkai, MD PhD Professor of Clinical Dermatology University of California, San Francisco A preview • Image review: Classic skin presentations of infections (and mimickers). Part 1. Classic cutaneous presentations of infectious diseases (and mimickers) • Speed rounds: the red leg • Image review: Classic skin presentations of infections (and Part 1. mimickers). Part 2. 18 year old, immunosuppressed for MCTD Rash not responding to topical steroids 1
3/12/19 Best first test to be performed in clinic: Best first test to be performed in clinic: 1 Bacterial culture 1 Bacterial culture 2 Viral culture 2 Viral culture 3 Viral direct fluorescence antibody (DFA) 3 Viral direct fluorescence antibody (DFA) 4 Skin biopsy 4 Skin biopsy 5 KOH test 5 KOH test Annular scaly eruption with central “clearing” Tinea corporis Trichophyton rubrum Trichophyton mentagrophytes Microsporum canis (inflammatory) Microsporum audouinii Diagnosis: KOH Morphology on mold cultures (low yield) Lactophenol plates (higher yield) Skin biopsy (PAS-D) HIV+ man, CD4 nadir = 4 Most likely infection is: 1 Molluscum contagiosum 2 Cryptococcus neoformans 3 Pseudomonas aeruginosa 4 Herpes simplex virus 5 Penicillium marneffei 2
3/12/19 Most likely infection is: Molluscum contagiosum 1 Molluscum contagiosum 2 Cryptococcus neoformans 3 Pseudomonas aeruginosa 4 Herpes simplex virus 5 Penicillium marneffei All except for pseudomonas are in the differential diagnosis in setting of HIV+, Chronic atopic dermatitis with acute flare CD4<50 1 Molluscum contagiosum: umbilicated papules 2 Cryptococcus neoformans: umbilicated papules 3 Pseudomonas aeruginosa 4 Herpes simplex virus: unusual morphology in immunosuppressed patients 5 Penicillium marneffei: umbilicated papules Please note: This is not an ARS question Best first test to be performed in clinic: Best first test to be performed in clinic: 1 Bacterial culture 1 Bacterial culture 2 Fungal culture 2 Fungal culture 3 Viral direct fluorescence antibody (DFA) 3 Viral direct fluorescence antibody (DFA) 4 Skin biopsy 4 Skin biopsy 5 KOH test 5 KOH test 3
3/12/19 Eczema herpeticum SLE on prednisone, mycophenolate mofetil J Murase, MD Best diagnosis is Best diagnosis is 1 Acne vulgaris 1 Acne vulgaris 2 Steroid-induced acne/ folliculitis 2 Steroid-induced acne/ folliculitis 3 Rash of systemic lupus erythematosus 3 Rash of systemic lupus erythematosus 4 Demodex folliculitis 4 Demodex folliculitis 5 Staphylococcal folliculitis 5 Staphylococcal folliculitis Demodex folliculitis in rosacea Demodex folliculorum, Demodex brevis 4
3/12/19 Bedside test Immunosuppressed liver transplant recipient Most likely infectious cause is Most likely infectious cause is 1 Staphylococcus aureus 1 Staphylococcus aureus 2 Streptococcus viridans 2 Streptococcus viridans 3 Borrelia burgdorferii 3 Borrelia burgdorferii 4 Bartonella henselae 4 Bartonella henselae 5 Vibrio vulnificus 5 Vibrio vulnificus Common d/dx of vascular neoplasm Immunosuppressed SCT recipient • Hemangioma/ angiomas • Glomus tumors • Kaposi Sarcoma • Bacillary angiomatosis • Pyogenic granuloma • Angiosarcoma • Melanoma (amelanotic) • Spitz tumor • Squamous cell carcinoma B Schwartz, MD 5
3/12/19 Most likely cause is Most likely cause is 1 Nocardia asteroides 1 Nocardia asteroides 2 Fusarium oxysporum 2 Fusarium oxysporum 3 Herpes simplex virus 3 Herpes simplex virus 4 Leukemia cutis 4 Leukemia cutis 5 Squamous cell carcinoma 5 Squamous cell carcinoma Immunosuppressed patient, 3 day ulcer Most likely cause of a rapid-forming ulcer is: 1 Factitial ulcer 2 Pyoderma gangrenosum 3 Herpes simplex 4 Pseudomonas aeruginosa 5 Capnocytophaga canimorsus Ahronowitz I, Harp J, Shinkai K (2012) Am J Clin Derm, 13: 191-211 Most likely cause of a rapid-forming ulcer is: Pyoderma gangrenosum 1 Factitial ulcer Inflammatory (not infectious) ulcer with neutrophils Diagnosis of exclusion 2 Pyoderma gangrenosum Violaceous rim, undermined border 3 Herpes simplex Can begin with pustule or � boil � 4 Pseudomonas aeruginosa Pathergy: triggered by (or worsens with) trauma 5 Capnocytophaga canimorsus Associated with: inflammatory bowel disease malignancy (myeloma, IgA) connective tissue disease 6
3/12/19 Ulcer with violaceous border, culture negative Ahronowitz I, Harp J, Shinkai K (2012) Etiology and management of pyoderma gangrenosum, Ahronowitz I, Harp J, Shinkai K (2012) Etiology and management of pyoderma gangrenosum, Am J Clin Derm, 13: 191-211 Am J Clin Derm, 13: 191-211 Most likely cause is 1 Acute generalized exanthematous pustulosis 2 Streptococcus viridans 3 Coxsackie A6 virus 4 Herpes simplex virus 5 Varicella zoster virus Most likely cause is 1 Acute generalized exanthematous pustulosis 2 Streptococcus viridans 3 Coxsackie A6 virus 4 Herpes simplex virus 5 Varicella zoster virus 7
3/12/19 Most common cause of “football” shaped vesiculopustules: 1 Herpes simplex virus 2 Erythema multiforme 3 Coxsackie A16 4 Varicella zoster virus 5 Chilblains lupus Most common cause of “football” shaped vesiculopustules: 1 Herpes simplex virus 2 Erythema multiforme 3 Coxsackie A16 – Hand, foot, mouth disease 4 Varicella zoster virus 5 Chilblains lupus Consult question: eczema management 8
3/12/19 Best diagnosis is: Best diagnosis is: 1 Severe atopic dermatitis 1 Severe atopic dermatitis 2 Psoriasis 2 Psoriasis 3 Drug eruption 3 Drug eruption 4 Retention hyperkeratosis 4 Retention hyperkeratosis 5 Scabies 5 Scabies Scabies: sarcoptes scabei 9
3/12/19 Speed rounds: the red leg Best diagnosis is: Best diagnosis is: 1 Bilateral cellulitis 1 Bilateral cellulitis 2 Bilateral erysipelas 2 Bilateral erysipelas 3 Vasculitis 3 Vasculitis 4 Venous stasis dermatitis 4 Venous stasis dermatitis 5 Pyomyositis 5 Pyomyositis No fever, no leukocytosis, bilateral itchy red legs D/dx of the red leg? • erysipelas • cellulitis • DVT • vasculitis • pyomyositis • necrotizing fasciitis • asteatotic dermatitis • stasis dermatitis • contact dermatitis Red Leg: Speed rounds 10
3/12/19 Fever, leukocytosis, red leg Stasis dermatitis Key features: • bilateral erythema, edema (L>>R) • varicose veins • brawny (golden) hyperpigmentation • no WBC, LAD, lymphangitis Rx: compression topical steroids Fever, leukocytosis, red leg Cellulitis • Unilateral • GAS, Staph aureus • Rapid spread • Toxic-appearing patient • WBC up, LAD, streaking Fever, leukocytosis, minimally � red � leg Erysipelas not responding to antibiotics • Superficial cellulitis (leg, face) • Strep (GAS > GBS) • F>M • Involves lymphatics • Clue: raised, shiny plaques 11
3/12/19 Pyomyositis • bacterial infection of muscle -S aureus (77%), strep (12%) • risk factors: -trauma -travel (tropics) -immunocompromised • Dx: MRI • Rx: surgical drainage psoas, gluteus, quadriceps* Necrotizing fasciitis • Strep/ staph infection of fascia • post-surgical • 20% mortality • pain out of proportion to exam • rapid spread (minutes to hours) • Dx: MRI • Rx: surgical debridement IV antibiotics Fever, leukocytosis, bilateral � red � legs Vasculitis • Clue: palpable purpura (bumps!) • favors dependent areas • bilateral • fever, malaise, arthralgias • may involve vessels of other organs -kidneys, joints, gut 12
3/12/19 No fever, no leukocytosis, but a red leg Contact dermatitis history of topical neomycin for � rash � • clue: red, angry, weeping, itch>pain • patient looks well • history is key • neomycin is top contact allergen • also: poison oak (rhus) topical diphenhydramine Red leg: Pearls Not all red legs are cellulitis Classic cutaneous presentations of infectious diseases (and mimickers) Bilateral cellulitis is rare. Reconsider diagnosis Many treatments for the � red leg � are exclusive Part 2. Superficial proximal onychomycosis due to: 1 Trichophyton rubrum 2 Fusarium oxysporum 3 Candida albicans 4 Penicillium marneffei 5 Pseudomonas aeruginosa 13
3/12/19 Superficial proximal onychomycosis due to: Also note purple nodules of Kaposi sarcoma 1 Trichophyton rubrum 2 Fusarium oxysporum 3 Candida albicans 4 Penicillium marneffei 5 Pseudomonas aeruginosa Differential diagnosis includes all but: Differential diagnosis includes all but: 1 Basal cell carcinoma 1 Basal cell carcinoma 2 Pyoderma gangrenosum 2 Pyoderma gangrenosum 3 Leishmania ulcer 3 Leishmania ulcer 4 Squamous cell carcinoma 4 Squamous cell carcinoma 5 Spider bite 5 Spider bite 14
3/12/19 Best next step: 1 Skin biopsy 2 Liquid nitrogen 3 Topical imiquimod cream 4 Podophyllin 5 Reassurance Pearly pink papules of the penis/ vulva Best next step: 1 Skin biopsy 2 Liquid nitrogen 3 Topical imiquimod cream 4 Podophyllin 5 Reassurance Bylaite M and Ruzicka T. N Engl J Med 2007;357:691 Traveler to Costa Rica Differential diagnosis for this ulcer: 1 Pyoderma gangrenosum 1 Herpes simplex virus 2 Mycobacterium marinum 3 Leishmania panamensis 4 Vasculitis 15
Recommend
More recommend