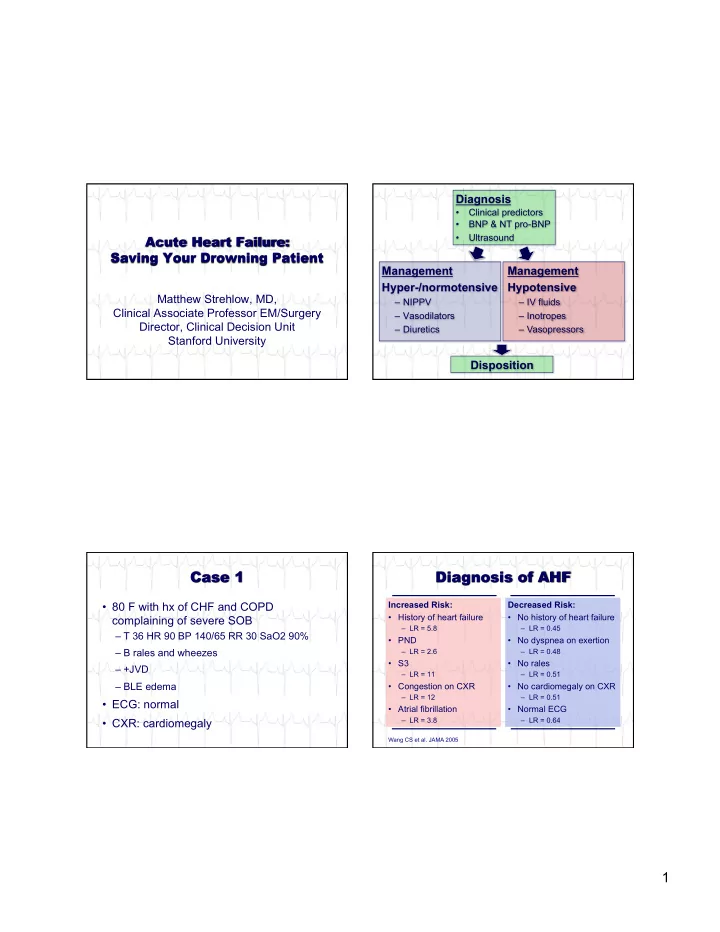
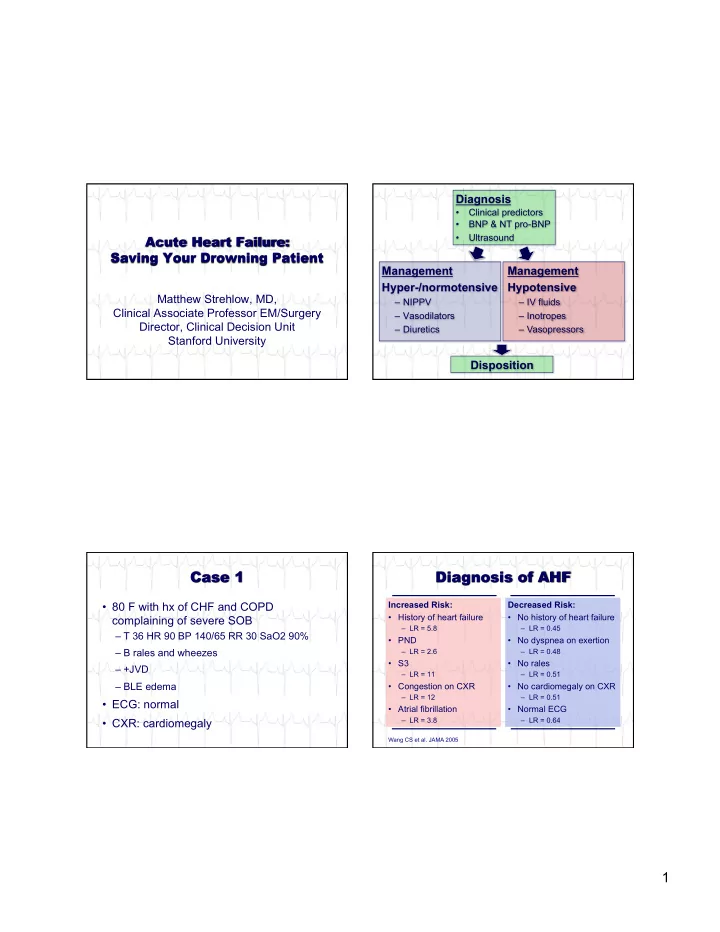
Diagnosis • Clinical predictors • BNP & NT pro-BNP Ultrasound • Management Management Hyper-/normotensive Hypotensive Matthew Strehlow, MD, – NIPPV – IV fluids Clinical Associate Professor EM/Surgery – Vasodilators – Inotropes Director, Clinical Decision Unit – Diuretics – Vasopressors Stanford University Disposition Increased Risk: Decreased Risk: • 80 F with hx of CHF and COPD • History of heart failure • No history of heart failure complaining of severe SOB – LR = 5.8 – LR = 0.45 – T 36 HR 90 BP 140/65 RR 30 SaO2 90% • PND • No dyspnea on exertion – B rales and wheezes – LR = 2.6 – LR = 0.48 • S3 • No rales – +JVD – LR = 11 – LR = 0.51 – BLE edema • Congestion on CXR • No cardiomegaly on CXR – LR = 12 – LR = 0.51 • ECG: normal • Atrial fibrillation • Normal ECG – LR = 3.8 – LR = 0.64 • CXR: cardiomegaly Wang CS et al. JAMA 2005 1
2.) Pro-BNP Secreted 1.) Stretching / 3.) Pro-BNP Cleaved Stress 1.0 NH2 COOH Post-test Post-test Sensitivity (True-Positive) COOH NH2 Pre-test BNP Probability for Probability for Probability 0.8 BNP < 105 pg/ml BNP > 300 pg/ml NT pro-BNP 10% 2% 46% 0.6 30% 5% 77% NH2 COOH COOH 0.4 50% 12% 88% NH2 Clinical Judgement 70% 25% 95% 0.2 NT-proBNP 90% 56% 99% Clinical Judgement + NT-proBNP Europa-trail.org 0.0 0.0 0.2 0.4 0.6 0.8 1.0 NH2 COOH Specificity (False-Positive) COOH NH2 Moe et al. Circulation 2007 Korenstein et al. BMC 2007 • Renal failure Age All <50 50-70 >70 – BNP as “rule out” (<100 or <200) if GFR <60 • Severe sepsis Rule Out <100 + <300* <300* <1200 ‡ – High elevations in both (BNP & NT pro-BNP) Sens/Spec 90%/74% 99%/85% 99%/85% 97%/55% • Pulmonary embolus – Moderate elevations in large PEs Rule In >400 + >450* >900* >4500 ‡ Sens/Spec 81%/90% 93%/95% 91%/80% 64%/86% ‡Berdague et al. Am Heart J 2006 +Korenstein BMC Emerg Med 2007 *Januzzi, Jr. et al Am J Cardiol 2005 2
• 80 F with hx of CHF and COPD • Greatest utility if diagnosis unclear complaining of severe SOB – T 36 HR 90 BP 140/65 RR 30 SaO2 90% • Multiple conditions cause “false” elevations – B rales and wheezes – (especially sepsis and renal failure) – +JVD – BLE edema • Know individual test characteristics! • ECG: normal • CXR: cardiomegaly • BNP: Pending B lines • Extravascular lung water – Examine lungs looking for “B lines” • Elevated right heart filling pressures – Examine IVC or IJ to estimate RAP 3
• 2 Lung Zones * – Both positive - LR 4.73 – Both negative - LR 0.3 • Alternative ^ – Sum B lines in all 8 zones, if >10 then LR 2.8 Courtesy of Anderson et al. Am J EM 2013 *Litelpo et al. Acad Emerg Med 2009 ^Anderson et al. Am J EM 2013 • Extravascular lung water – Examine lungs looking for “B lines” Distance • Elevated right heart filling pressures – Examine IVC or IJ to estimate RAP 4
• Elevated RAP (>10mmHg) * • Extravascular lung water – IVC >2cm - LR 4.7 – Examine lungs looking for “B lines” • Alternatives ^# • Elevated right heart filling pressures – Collapsibility index <20% – Examine IVC or IJ to estimate RAP – Jugular venous pressure >8 cm ^Anderson et al. Am J EM 2013 *Blair JE, et al. Am J Cardiology 2009 # Cheng et al. J Emerg Med 2012 High risk findings Low risk findings – Hx of CHF – No hx of CHF – PND – No DOE • Combined lung edema and elevated RAP – S3 – No rales – Both positive - LR 13 (for acute heart failure) – Congestion (CXR) – No cardiomegaly – A-fib – Normal ECG • BNP – consider if unsure of diagnosis • Ultrasound – B lines and elevated RAP 5
• 80 F with hx of CHF and COPD • 57 yo male with a history complaining of severe SOB of CHF c/o severe SOB. • PE: – HR 120, BP 185/110, • ECG: normal RR 30, SaO2 85% RA • CXR: cardiomegaly – Diaphoretic • BNP: 450 – Bilateral rales • US: + B lines & – BLE edema elevated RAP Which of the following methods of O2 Which of the following methods of O2 delivery decreases mortality? delivery decreases mortality? A. Non-rebreather face mask A. Non-rebreather face mask B. Bi-level positive airway pressure B. Bi-level positive airway pressure (BiPAP) (BiPAP) C. Continuous positive airway pressure C. Continuous positive airway pressure (CPAP) (CPAP) D. All of the above are equivalent D. All of the above are equivalent 6
ESTABLISHED IN 1812 JULY 10, 2008 VOL 359 NO. 2 Noninvasive Ventilation in Acute Cardiogenic Pulmonary Edema • 1069 ED patients randomized to 2 hrs of: • BiPAP • CPAP • Oxygen by NC or FM • Improves symptoms of dyspnea • Unclear effect on mortality and ETI • Consider in patients with: – Significant respiratory symptoms – O2 saturation <90% 62/367 (17%) Patients Crossed Over!!! 7
How much IV furosemide should be How much IV furosemide should be given to this patient as part of his given to this patient as part of his initial stabilization? His outpatient initial stabilization ? His outpatient regimen is 80 mg/day. regimen is 80 mg/day. A. None A. None B. 40 mg B. 40 mg C. 80 mg C. 80 mg D. 160 mg D. 160 mg 1. Low cardiac output and over-diuresis Diuretic Strategies in Patients with Acute leads to WRF Decompensated Heart Failure 2. WRF during hospitalization for AHF leads to increased mortality • Double-blind RCT with 308 patients • Administered loop diuretics for 72 hrs by • Bolus or Infusion • High or Low doses • Outcomes: symptoms & rising creatinine 8
1. Low cardiac output and over-diuresis Diuretic Strategies in Patients with Acute leads to WRF Decompensated Heart Failure 2. WRF during hospitalization for AHF leads to increased mortality • No difference between groups (bolus vs infusion or high vs low dose) • Symptoms • Creatinine • Adverse outcome (death, ED visits, and rehospitalization) How much IV furosemide should be 1. Low cardiac output and over-diuresis given to this patient as part of his leads to WRF initial stabilization ? His outpatient 2. WRF during hospitalization for AHF leads regimen is 80 mg/day. to increased mortality A. None 1. Elevated CVP and venous congestion B. 40 mg lead to worsening renal failure C. 80 mg 2. Transient WRF may not lead to increased D. 160 mg mortality 9
FUROSEMIDE EFFECT ON CARDIAC PHYSIOLOGY • Venous dilation LOOP DIURECTICS - Minutes to Onset of Action • Delayed onset – Healthy subjects PVR – Maximized at 20 mg IV – 45 to 120 minutes 120 SVR 90 • Arterial constriction • Diuretic MAP 60 – CHF patients resistance HR – Predominates early – Daily users 30 RAFP 0 Healthy CHF SV Mattu et al. Emerg Med Clin North Am 2005 • Improves symptoms of dyspnea • 25-50% of • Effect on outcomes is unknown patients in AHF are intravascularly • Adverse cardiovascular effects early volume low • Caution using as a single agent during initial stabilization 10
“ Intravenous Nitrates in the What is optimal method of nitrate Prehospital Management of Acute Nitrate Properties Pulmonary Edema ” administration in this patient? • Bertini, et al., Ann Emerg Med. 1997 Venous and A. Nitropaste “ Intravenous Nitroglycerin Boluses in arterial dilation Treating Patients with Cardiogenic 1” to chest wall Pulmonary Edema ” Recommended in • Nashed, et al., Am J Emerg Med. B. Nitro SL cardiac ischemia “ Emergency Treatmet of Severe 0.4mg Q 5 min x 3 Cardiogenic Pulmonary Edema with Rapid onset of Intravenous Isosorbide-5- C. Nitro infusion Mononitrate ” action • Harf, et al., Am J Cardiol. 1988 20 mcg/min titrated 10mcg/min Q 5 min Short half-life “ Comparison of Nitroglycerin, D. Nitro infusion Morphine and Furosemide in Minimal side Treatment of Presumed Pre-hospital 100 mcg/min titrated 20mcg/min Q 3 min Pulmonary Edema ” effects • Hoffman, et al., Chest. 1987 What is optimal method of nitrate Cotter et al. Lancet 1998 ADVERSE EFFECTS* - administration in this patient? Isosorbide Dinitrate vs. Furosemide • 3 mg isosorbide 50 A. Nitropaste dinitrate IV Q 5 min 1” to chest wall (600 mcg/min) 40 B. Nitro SL 30 0.4mg Q 5 min x 3 24 20 C. Nitro infusion 13 • No hypotension 20 mcg/min titrated 10mcg/min Q 5 min 10 requiring treatment D. Nitro infusion 0 • No SBP <85mmHg 100 mcg/min titrated 20mcg/min Q 3 min Isosorbide DiNitrate Furosemide *Death, Mechanical Ventilation, Myocardial Infarction p<0.05 11
• Nitropaste • Nitropaste – Erratic absorption – Erratic absorption – Slow onset of action – Slow onset of action • Nitroglycerin SL – Equivalent to 60 to 80 mcg/min • Nitropaste • First line therapy – Erratic absorption – Slow onset of action • Nitroglycerin SL • High doses are safe and effective – Equivalent to 60 to 80 mcg/min • Nitroglycerin Infusion – Start ≥ 100 mcg/min and rapidly titrate to: • symptom improvement • Use in patients with hyper-/normotensive • 30% reduction in MAP • MAP <90 12
Recommend
More recommend