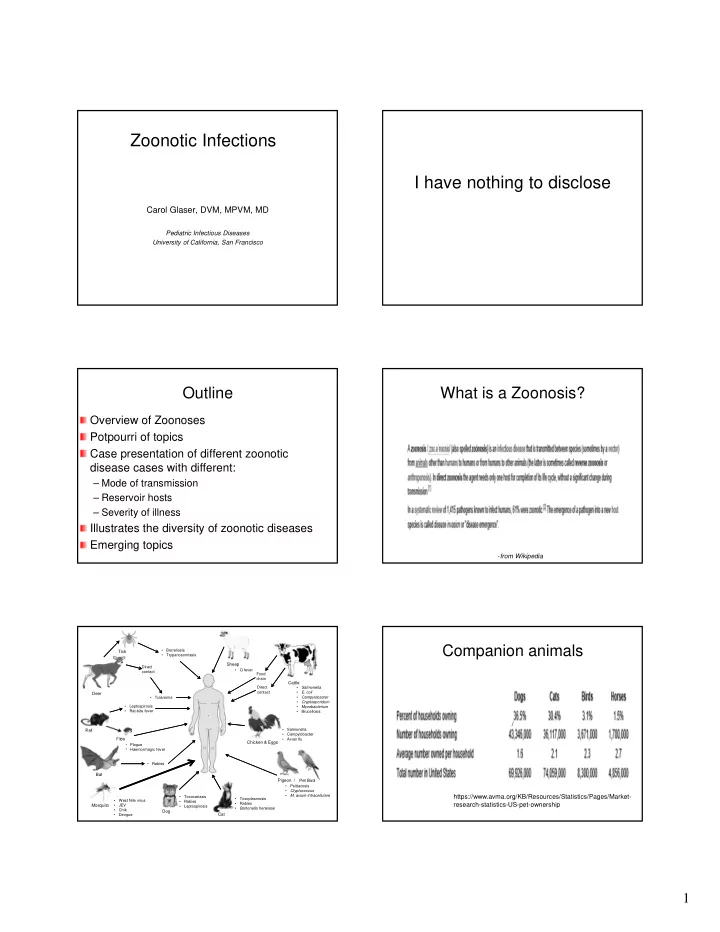
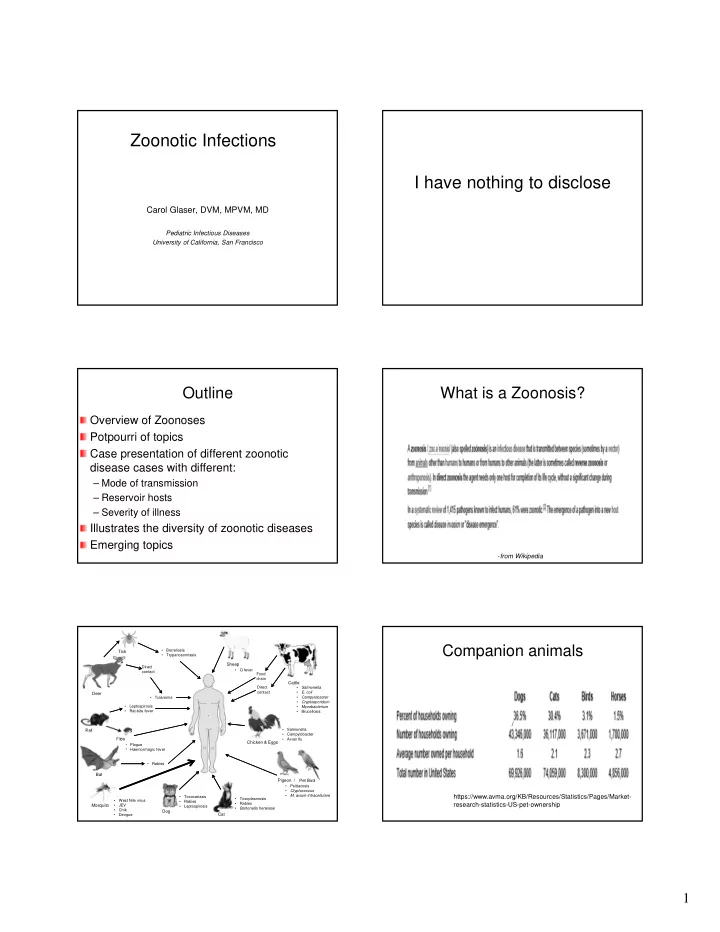
Zoonotic Infections I have nothing to disclose Carol Glaser, DVM, MPVM, MD Pediatric Infectious Diseases University of California, San Francisco Outline What is a Zoonosis? Overview of Zoonoses Potpourri of topics Case presentation of different zoonotic disease cases with different: – Mode of transmission – Reservoir hosts – Severity of illness Illustrates the diversity of zoonotic diseases Emerging topics - from Wikipedia Companion animals • Borreliosis Tick • Trypanosomiasis Sheep Direct • Q fever contact Food chain Cattle Direct • Salmonella contact • E. coli Deer • Tularemia • Campylobacter • Cryptosporidum • Leptospirosis • Mycobacterium • Rat-bite fever • Brucellosis / • Salmonella Rat • Campylobacter • Avian flu Flea Chicken & Eggs • Plague • Haemorrhagic fever • Rabies Bat Pigeon / Pet Bird • Psittacosis • Ctyptococcus • M. avium-intracellulare https://www.avma.org/KB/Resources/Statistics/Pages/Market- • Toxocariasis • Toxoplasmosis • West Nile virus • Rabies • Rabies research-statistics-US-pet-ownership Mosquito • JEV • Leptospirosis • Bartonella hensleae • Chik Dog Cat • Dengue 1
Specialty and Exotic Animals Zoonosis: General Many are missed because of vague clinical presentation –’viral’ Lack of awareness Diagnosis is often problematic – Tests not widely available – Orphan diseases “new twists” https://www.avma.org/KB/Resources/Statistics/Pages/Market-research- - Handout slightly different > PowerPoint statistics-US-pet-ownership.aspx#exotic A Partial List of When you hear hoof beats… Bacterial Zoonoses Psittacosis Anthrax Q Fever Brucellosis Rat-bite Fever Campylobacteriosis Relapsing Fever Cat Scratch Disease Rocky Mountain Spotted Ehrlichiosis Fever E. coli 0157:57 Salmonellosis Glanders Tularemia Leptospirosis Typhus Fever Listeriosis Yersiniosis Zoonotic Tuberculosis Lyme Disease Melioidosis Plague A Partial List of A Partial List of Viral Zoonoses Parasitic Zoonoses Protozoa Helminths: (roundworms, Herpesvirus B Arenaviruses (LCMV, Lassa, S. tapeworms, flukes)* American hemorrhagic fevers) Influenza (avian) Babesiosis Bat lyssaviruses Anisakiasis Japanese encephalitis Cryptosporidiosis* Cysticercosis Colorado tick fever Nipah Leishmaniasis* Hydatidosis Ebola Rabies Giardiasis* Mesocestoidiasis Equine encephalitides (WEE, Rift Valley fever Toxoplasmosis* Schistosome Dermatitis EEE, VEE) SARS Trypanosomiasis (Swimmer’s Itch) Hantaviruses (Hantaan, Sin Vesicular stomatitis Trichinosis* Nombre) West Nile Virus Visceral Larval Migrans* Hendra Toxocariasis/ Baylisascaris 2
Emerging infectious diseases Estimated that 75% are zoonotic – Many viral Case 1 – Many vector borne (e.g., West Nile virus) -Chomel et al., Emerg Inf Dis 2006 Girl with Fever & Rash 8 year old female – Developed headache, fever , sore throat – 4 days later: macular rash on hands/feet--later petechial – 1 week: severe arthralgias, refusal to walk – Seen by several physicians; primary MD, rheumatologist, oncologist, dermatologist – Pediatric ID consulted just before bone marrow Girl with Fever & Rash Girl with Fever & Rash When asked specifically about rodents - CBC, urinalysis: normal patient owned a rat but no bite history (mother Blood / urine culture negative didn’t consider it a “pet”) Unremarkable PMH except allergy to PEN Blood culture repeated with RBF diagnosis in No recent travel mind (micro lab can optimize isolation of No tick bites, denied pet ownership organism with special techniques): No unusual dietary history – Blood culture positive for Streptobacillis moniliformis 3
Rat Bite Fever Rat Bite Fever: Microbiology Streptobacillus moniliformis: Epidemiology Two distinct disease syndromes Typically transmitted by bite or scratch of rats, – Streptobacillus moniliformis: most cases in US mice, squirrels, carnivores that prey on rodents Incidence unknown since not a reportable disease Can be acquired through handling of dead rats Probably rare but likely underdiagnosed 50-100% wild and lab rodents harbor organism Relatively difficult to isolate Food/water contaminated with infected rat – Spirillum minor : not generally found in US excreta (cases called Haverhill) Mostly in Asia Different syndrome 40% of cases no history of bite Sodoku or relapsing fever Rat Bite Fever: Clinical Incubation: ~ 7 days (range 1-10 days) Abrupt onset fever (irregular relapsing fever) Chills, headache Migratory arthralgias, myalgias Clinical features similar to other diseases Diagnosis usually requires high index of suspicion Rat Bite Fever Complications – Endocarditis, myocarditis, pericarditis Case 2 – Meningitis – Pneumonia – Abscesses in “virtually every organ” Untreated: 7-13% mortality Treatment – Penicillin or Doxycycline Elliot et al., Clin Microbiol Rev, 2007 Dijkmans et al., Infection, 1984 Pins et al., Clin Inf Dis, 1996 4
11 m/o male with Encephalopathy 11 m/o male with Encephalopathy Examination findings History of present illness – Right eye – 5 days PTA: developed irritability deviated medially – 2 days PTA: unable to sit diffuse serpiginous lesions Other history – Hypertonicity extremities – no major illnesses; vaccines UTD Lab findings – 1 older sibling, both parents healthy – CBC: 18K WBCs, 50% lymph, 17% eosin – travel to Sierra Nevada 4 weeks PTA – CSF: 50 WBCs, 45% eosin – lives in Pacific Grove Cranial MRI – spends much time outdoors; occasional pica noted – “patchy” disseminated white matter 11 month old male with 11 m/o male with Encephalopathy Encephalopathy Hospitalized for workup and treatment Serology/PCR: negative Serum sent to Purdue University: – Toxocara, Coccidioides, Varicella, HSV – Positive for Baylisascaris procyonis Cultures: negative – blood, CSF, urine Treatment – acyclovir, erythromycin, steroids, clonazepam, albendazole Baylisascaris procyonis Balamuthia vs. Bayilsascaris Intestinal nematode Balamuthia: Free-living amoeba Natural hosts – adult raccoons Bayliascaris: a worm Transmission – eggs shed in feces (millions of eggs shed) Both can cause CNS illness but very – require 3-4 weeks to become infectious different – ova extremely resistant to dessication/destruction; may remain viable in the environment for years 5
Baylisascaris procynosis Baylisascaris procynosis Human infections rare 3 forms – Despite high potential for exposure, few cases reported A. organs: visceral larva migrans (VLM) – Infected animals shed millions eggs/day, ~90% [only one documented case] juvenile raccoons infected in some areas B. brain: neural larval migrans (NLM) [typically – ~20 human cases reported young children, but case reports of older individuals] Risk factors for infection C. eye: Ocular larva migrans (OLM) [adults ] – Contact with raccoon feces or an environment contaminated by infected feces and geophagia or pica – “Suspect vehicles” include soil, wood, leaves and other vegetation, bark, and stone - Chun et al., Pediatr Inf Dis, 2009 Gavin et al., Clin Microbiol Rev 2005 Wise et al., Microbes and Infection, 2005 Wise et al., Microbes and Infection 2005 An emerging parasite.. Who is at risk? Contact with raccoon feces or an environment contaminated by infected feces and geophagia or pica Typically young children, males > female Other cases; Developmental delay with history of pica Teenager with substance abuse 73 year old with Alzheimer-type dementia -Hung et al., Emerg Infect Dis, 2012 -Chung et al., Pediatr Infect Dis J, 2009 Epidemiology Baylisascaris NLM Raccoon defecate in “latrines” Often devastating outcome with death or severe neurologic sequelae -outside or inside: However, a few ‘promising’ case reports – 14 month old boy with NLM from MA, some residual deficits and Eggs of Baylisascaris very hardy moderate speech delay but overall good – 4 year old boy from New Orleans, LA with NLM, “full recovery” – Highly resistant to desiccation – Both Rxed with steroids and anti-helminthic – Viability not affected by freeze/thaw – However relatively low thermal death point (<62 C) Peters et al., Pediatrics, 2012 Pai et al., Emerg Inf Dis, 2007 -Shafir et al., Emerg Infect Dis, 2011 6
Baylisascaris procynosis More severe than Toxocara – larger larvae (1-2 mm) Male – extensive migration (brain, eye, heart) Clinical – eosinophilic meningoencephalitis – death or long-term DD in children Pathology – deep cerebral white matter granulomas Female Adult Baylisascaris procyonis Other potential hosts opossums Kinkajous Olingos 72 y/o male with lethargy and ascending paralysis Case 3 Onset of headache/fever 5 days later hospitalized with lethargy, somnolence and ascending paralysis Clinician thought it was probably a stroke but wanted to rule out encephalitis 7
Recommend
More recommend