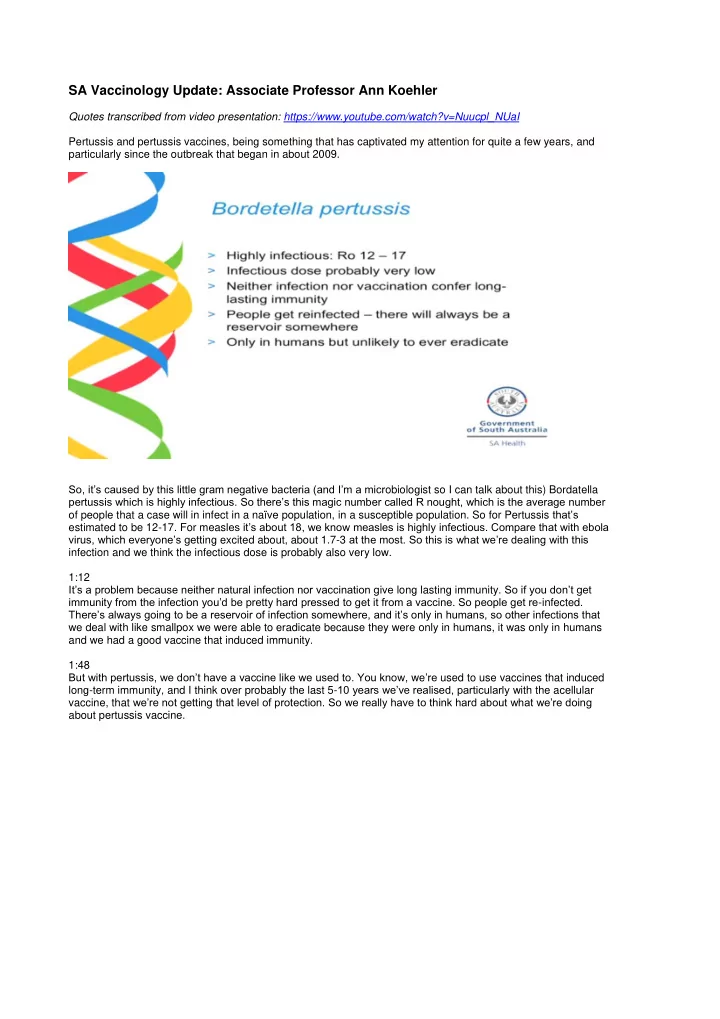
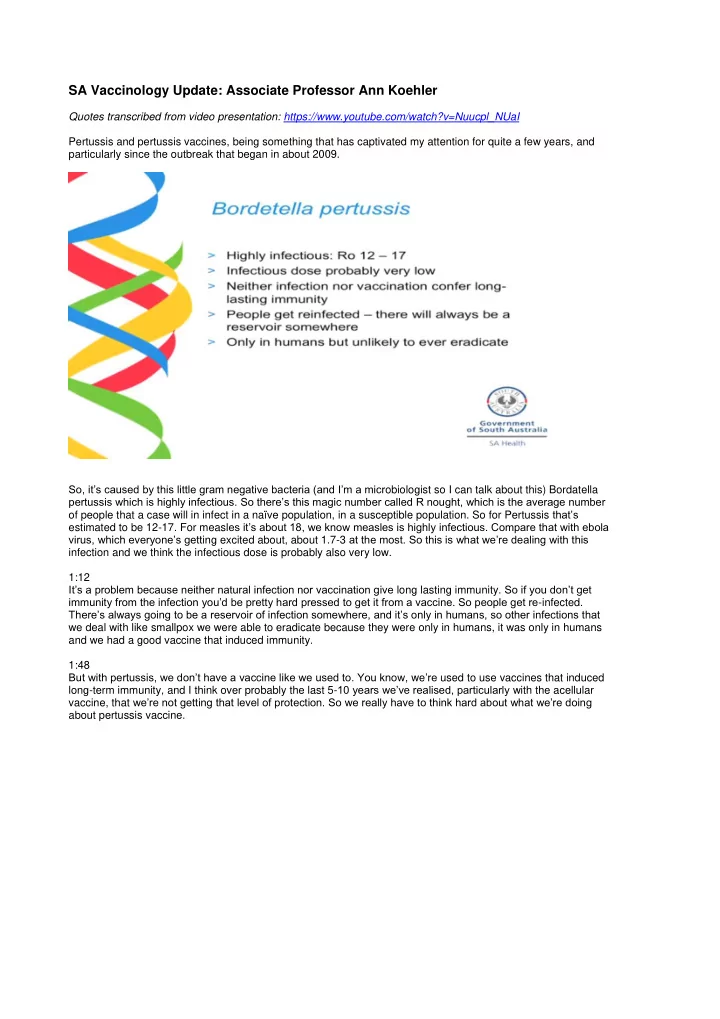
SA Vaccinology Update: Associate Professor Ann Koehler Quotes transcribed from video presentation: https://www.youtube.com/watch?v=Nuucpl_NUaI Pertussis and pertussis vaccines, being something that has captivated my attention for quite a few years, and particularly since the outbreak that began in about 2009. So, it’s caused by this little gram negative bacteria (and I’m a micr obiologist so I can talk about this) Bordatella pertussis which is highly infectious. So there’s this magic number called R nought, which is the average number of people that a case will in infect in a naïve population, in a susceptible population. So for Pertussis that’s estimated to be 12-17. For meas les it’s about 18, we know measles is highly infectious. Compare that with ebola virus, which everyone’s gett ing excited about, about 1.7-3 at the most. So this is what we’re dealing with this infection and we think the infectious dose is probably also very low. 1:12 It’s a problem because neither natural infection nor vaccination give long lasting immunity . So if you don’t get immunity from the infection you’d be pretty hard pressed to get it from a vaccine. So people get re -infected. There’s always going to be a reservoir of infection somewhere, and it’s only in humans, so other infections that we deal with like smallpox we were able to eradicate because they were only in humans, it was only in humans and we had a good vaccine that induced immunity. 1:48 But with pertussis, we don’t have a vaccine like we used to. You know , we ’re used to use vaccines that induced long-term immunity, and I think over probably the last 5- 10 years we’ve realised, particularly with the acellular vaccine, that we’re not getting that level of protection. So we really have to think hard about what we’re doing about pertussis vaccine.
2:17 Susceptibility is universal in unimmunised people and in the pre-vaccine era everybody got it by the age of five. It was one of the famous diseases of childhood, and for a long time people thought that it was only a disease of childhood. They often didn’ t recognise pertussis in older people. 2:42 There’s a secondary attack rate in households of over 90%, so you can see why really everybody got it early. The incidence is highest in the first five years, except where you’ve got r eally, really, effective infant immunisation programs. 2:58 But what we’ve seen is a shift to older age groups, which a few people have alluded to here. Howev er, I’d like to just raise in your heads the thought that maybe there’s a few diagnosis issues that are contributing to that picture. 3:14 And diagnosis is based on a number of tests. So clinical diagnosis – those of you who work in clinical practice know the three phases of the illness – so there’s that early non - specific catarrhal illness, then there’s that classic whooping cough with the inspiratory whoop and post-tussive vomiting, and then a convalescent phase that often has a relapse of that second-phase symptoms. But this classical illness, it appears, is really only in the older children – sort of infants and the older children up to adolescent age. 3:56
So babies simply might stop breathing, and adults can just have a prolonged coughing illness, (4:02) so for a long time people didn’t think that adults got pertussis because they just got this cough, and adults get coughs for lots of reasons. Then there’s culture. And this is B ordet Gengou agar plate, which is for culturing Bordatella. It has to be made up within four hours of use, and these days with laboratories all being centralis ed and often not on site, that’s just not feasible any more. And apart from that it’s a very expensive way to practice mi crobiology, so hardly anybody does culture anymore. There’s still a few good children’s hospitals who still do this, and it probably doesn’t matter except that if we start to have concerns about antibiotic susceptibility we might want to get more culture s pecimens, but even with prompt culturing at the bedside fresh cultures, it wasn’t easy to grow this bacteria. 5:10 So then serology came along. Serology is smoke and mirrors stuff I hate to tell you. It’s really very difficult to interpret and subjective for many diseases - and pertussis is one of the worst. So in early infection, often you haven’t got antibodies so it’s unreliable. When you need it the most you don’t know. Anyone who’s worked in a lab knows that getting that second serum – for ped serum to see if you have seroconversion or a four-fold rise hardly ever happens. It’s very unreliable in infants under two years of age , and they’re the ones really who are the most clinically affected group that you want the diagnosis for. And in serology it’s also difficult to distinguish past infection from current infection, from vaccination - so it’s not very useful, it’s not timely and it’s certainly not the test of choice.
6:08 So now we have Nucleic Acid Testing, which is sensitive. It ’s specific, it’s fast and it is the test of choice. But it can’t tell infection from carriage, and one thing that has come to my attention is calls from GPs who say “one chi ld in the family had pertussis and so I swabbed all the others and they’ve come up with positive PCRs, do I treat them or not?” So we do get a certain level of asymptomatic or very mild infections that probably don’t need treatment - they’re probably infec tious. What does that test result really mean? Because PCR testing is easy and not invasive – just a throat swab, or a nasopharyngeal swab you get a lot more testing than you do if you have to send that little 18 month old baby to get blood taken. Not that that’s a bad thing but it does distort our epidemiological information. 7:09 Now pertussis isn’t the most preventable of the vaccine preventable diseases, as you all know, so even though we’ve ha d this vaccine since the 1940s - it’s been in our immunisation program since the mid 50s - it is the most commonly notified vaccine preventable in Australia over the past 20 years, and probably in all of the developed world. From 2006-12 there were epidemics in all jurisdictions and we were all using acellular vaccines (and I think I saw Stephen Lambert in the audience who would have a few things to say about that) but the average annual notification rate was more than 2.8 times that of the previous decade.
7:54 In contrast though, hospitalisation and mortality rates remained the same. So we were probably just detecting a lot more pertussis as well – there were more cases but there weren’t more serious cases. 7:11 Now, if you look on our SA Health website you’ll have seen this sl ide because we put it up every week, and on the right hand side it creeps out a little further, but it shows that huge big outbreak we had starting with the pandemic in 2009 and in that pandemic we got a lot more PCR testing done, and also babies with pertussis got tested (looks at watch – “I’d better talk a bit faster”). We certainly had a lot of pertussis cases and I’m using data really from that outbreak period because as you can see there’s not r eally a lot to talk about since. But what worries me is we are here, are we going to go up again? and we must be going to. 8:56 Just to show you our testing, this was back at the end of 2010, so we were getting half of our testing from PCR and now it’s much more than that, so we’re probably detecting a lot of cases that wouldn’t have been detected previously, simply because people will do that test.
Data from that time in South Australia was in the enviable position of having an infection rate of 448 – a notification rate of 448.8 per 100,000 – for 10,000 sorry – which was many times the national average and we were the world leaders at that stage. We had four deaths over the previous 20 years, but only one death during that huge outbreak in an infant in South Australia, so even though one death is one too many, I think it was more that we had very very good data capture, and South Australia’s got the best notification system in Australia, because we have both laboratory notification and doctor notification, so we don’t very much miss a c ase, whereas other states certainly do. If a doc tor doesn’t do the test they never hear about it – they’ve only the laboratory notification. So we have very good case ascertainment and so even though we had such a big outbreak we didn’t feel terribly guilty about what we were doing. 10:24 We were under a huge amount of pressure to introduce a cocooning program and we resisted that because our data didn’t suggest that it was going to w ork. 10:35 And this was the data that I think was the most convincing. If you looked at our childhood notification – so these were previously vaccinated cases in children under 12 years of age – so 2,500 cases and more than a third of them had had five pertussis vaccinations. This was when there was still the 18 month dose. 60% had had at least four, (11:03) 90% were fully vaccinated – they’d had three vaccinations.
Recommend
More recommend