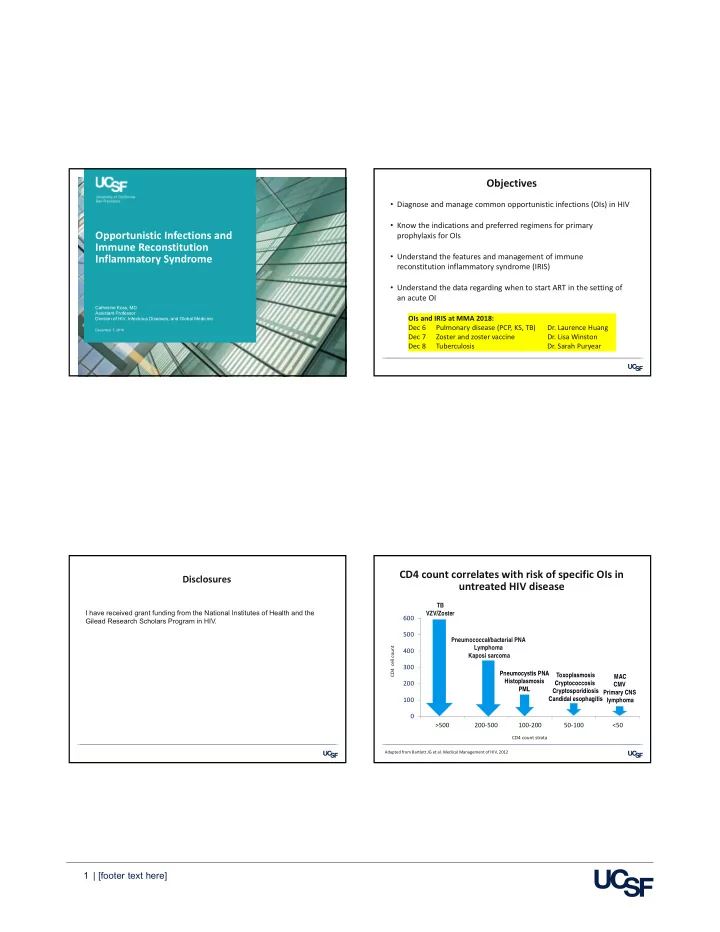
Objectives • Diagnose and manage common opportunistic infections (OIs) in HIV • Know the indications and preferred regimens for primary Opportunistic Infections and prophylaxis for OIs Immune Reconstitution • Understand the features and management of immune Inflammatory Syndrome reconstitution inflammatory syndrome (IRIS) • Understand the data regarding when to start ART in the setting of an acute OI Catherine Koss, MD Assistant Professor OIs and IRIS at MMA 2018: Division of HIV, Infectious Diseases, and Global Medicine Dec 6 Pulmonary disease (PCP, KS, TB) Dr. Laurence Huang December 7, 2018 Dec 7 Zoster and zoster vaccine Dr. Lisa Winston Dec 8 Tuberculosis Dr. Sarah Puryear CD4 count correlates with risk of specific OIs in Disclosures untreated HIV disease TB I have received grant funding from the National Institutes of Health and the VZV/Zoster 600 Gilead Research Scholars Program in HIV. 500 Pneumococcal/bacterial PNA CD4 cell count Lymphoma 400 Kaposi sarcoma 300 Pneumocystis PNA Toxoplasmosis MAC Histoplasmosis 200 Cryptococcosis CMV PML Cryptosporidiosis Primary CNS Candidal esophagitis 100 lymphoma 0 >500 200‐500 100‐200 50‐100 <50 CD4 count strata Adapted from Bartlett JG et al. Medical Management of HIV, 2012 1 | [footer text here]
With potent ART, incidence of OIs continues to decline Resources for OI management N = 63,541 U.S. patients in NA‐ACCORD, 2000‐2010 PCP Candidal esophagitis MAC https://aidsinfo.nih.gov/guidelines Ward 86 Management Recommendations http://hivinsite.ucsf.edu/InSite?page=md‐ward86‐index Buchacz K et al. JID 2016. We still see OIs in the U.S. among: Case 1 1) Patients newly diagnosed with HIV who present with an OI (late HIV dx) 44 y/o M with HIV • CD4 94 cells/mm 3 2) Patients who are aware of their HIV status but face barriers to taking ART • not on ART or prophylaxis 3) Patients for whom ART fails to achieve adequate immunologic/virologic 1 month of progressive dyspnea, • response non‐productive cough, fevers, night sweats, and weight loss CD4 <200 or OI at HIV diagnosis Globally United States, 2016 1 Exam: Afebrile, 90% RA Tuberculosis 40% 36% • • Diffuse crackles bilaterally and 33% #1 cause of AIDS deaths 27% mild wheezing 30% Cryptococcal meningitis 2 17% 20% Labs: WBC 8.3 • 223,000 cases in 2014 9% 10% • 181,000 deaths • LDH 386, Beta‐D‐glucan>500 0% • 15% of AIDS deaths • ABG: 7.44/35/59 on room air 13‐24 25‐34 35‐44 45‐54 55+ Age, years 1. CDC HIV Surveillance Supplemental Report 2018; 23(4). 2. WHO Cryptococcal Guidelines 2018. 2 | [footer text here]
CT Chest Case 1 continued • Started on empiric CTX/doxycycline + TMP‐SMX/prednisone • Could not obtain induced sputum • Bronchoscopy with BAL performed for microbiologic confirmation: - Bacterial culture: oral flora - AFB smear and culture: negative - PCP positive • TMP‐SMX + prednisone continued Which empiric therapy would you start? Pneumocystis pneumonia • PCP = Pneumocystis pneumonia A. Ceftriaxone + doxycycline • Caused by P. jirovecii B. TMP‐SMX + prednisone - ubiquitous fungus - P. carinii now refers to the organism that infects rodents C. Ceftriaxone + doxycycline + TMP‐SMX + prednisone • 90% of cases occur at CD4 <200 cells/mm 3 D. RIPE - Most cases with CD4 <100 E. Ganciclovir • Subacute presentation of nonproductive cough, progressive dyspnea, fever • Hypoxemia; normal lung exam or dry crackles DHHS OI Guidelines 2018. 3 | [footer text here]
See Dec 6 talk by PCP: Treatment PCP: Imaging Dr. Laurence Huang Disease Preference Regimen Potential toxicities • CXR pattern: Adverse effects are common severity (21 days then start secondary ppx) - Classic: bilateral, reticular interstitial infiltrates Rash, fever, leukopenia, Moderate to Preferred TMP + SMX (weight‐based) thrombocytopenia, azotemia, severe Adjust dose for renal function hepatitis, hyperkalemia - Pleural effusions, cavitation, intrathoracic adenopathy are rare IV PO after clinical improvement • Try to “treat through” reactions if PaO2 <70 possible - May be normal • Desensitization protocols available A‐a grad 35 Steroids within 72 hours for patients with allergy Prednisone 40 mg BID x 5 days • STOP and do not re‐challenge if pt Prednisone 40 mg daily x 5 days has Stevens‐Johnson syndrome or Prednisone 20 mg daily x 11 days toxic epidermal necrolysis • If normal CXR high‐resolution CT for ground glass - High negative predictive value Mild Preferred TMP + SMX (weight‐based) PaO2 70 A‐a grad <35 • Cystic disease – increased risk of spontaneous pneumothorax • PTX should prompt high suspicion for PCP DHHS OI Guidelines 2018. DHHS OI Guidelines 2018. NIH‐UC Expert Panel for Corticosteroids as Adjunctive Therapy for PCP. NEJM 1990. PCP: Laboratory diagnostics PCP: Treatment failure • Elevated LDH: Common, non‐specific • If patient not improving after 3 days, is this treatment failure? • Plasma β‐D‐glucan - Generally no; early worsening at 3‐5 days is common - Sensitivity 92%, specificity 65% 1 - (1‐3)‐β‐D‐glucan is a component of the cell wall of most fungi - Wait at least 4‐8 days for a clinical response before switching therapy for clinical failure • Other causes of positive BDG: candidiasis , histoplasmosis, cryptococcus • Dx requires microbiologic confirmation • Evaluate for concurrent infections as a cause for clinical failure • No culture system for P. jirovecii - consider repeat bronch • Sensitivity of stained respiratory specimen depends on method, experience of lab - Induced (not expectorated) sputum : <50‐90% - BAL : 95‐100% - Organisms detectable for days‐weeks after rx • Do not delay empiric therapy PCP cysts in silver‐stained 1. Sax P et al. CID 2011. DHHS OI Guidelines 2018. bronch specimen. CDC PHIL. 4 | [footer text here]
PCP: Treatment Case 2 continued Disease Preference Regimen Potential toxicities severity (21 days then start secondary ppx) Adverse effects are common Rash, fever, leukopenia, Moderate to Preferred TMP + SMX (weight‐based) thrombocytopenia, azotemia, severe Adjust dose for renal function • CT shows bulky necrotic nodes in mediastinum and retroperitoneum hepatitis, hyperkalemia IV PO after clinical improvement • Try to “treat through” reactions if PaO2 <70 possible A‐a grad 35 Steroids within 72 hours • Desensitization protocols available Prednisone 40 mg BID x 5 days for patients with allergy Prednisone 40 mg daily x 5 days • STOP and do not re‐challenge if pt Prednisone 20 mg daily x 11 days has Stevens‐Johnson syndrome or toxic epidermal necrolysis Anemia, rash, fever, diarrhea Alternative #1 Clindamycin + primaquine + steroids (rx failure/ Check G6PD toxicity) Irreversible renal and pancreatic Alternative #2 Pentamidine IV + steroids Historically preferred. Higher mortality islet cell toxicities, arrhythmias, in retrospective studies. We avoid. hypoglycemia, hypotension Mild Preferred TMP + SMX PaO2 70 Anemia, rash, fever, diarrhea Alternative Clindamycin + primaquine. Check G6PD Rash, fever A‐a grad <35 Dapsone + TMP. Check G6PD HA, nausea, diarrhea, rash, LFTs Atovaquone BID with food DHHS OI Guidelines 2018. NIH‐UC Expert Panel for Corticosteroids as Adjunctive Therapy for PCP, NEJM 1990. Ward 86 Management Recommendations, HIV InSite. Case 2 CT chest 40 yo M with HIV (CD4 420 and VL <40 on DTG + FTC/TAF 1.5 years ago), • Numerous pulmonary nodules in UL and RML, largest 1.8 cm lost to follow‐up. Presents with several weeks of progressive symptoms: diffuse abdominal pain, fever, diarrhea (10x per day), and cachexia • PMH : - HIV diagnosed 2 years ago, CD4 380, VL 80K • Social History : - Immigrated to CA from Mexico 20 years ago - Marginally housed • Labs : - Hgb 7, normal LFTs, Cr 1.0 - CD4 48 (6%), VL pending 5 | [footer text here]
What is the most likely diagnosis? Case 2 continued • Stool cultures and O&P ‐ Giardia Ag positive A. Cytomegalovirus (CMV) • Serum Cryptococcal Ag (CrAg) ‐ negative • Urine Histoplasma Ag ‐ negative B. Mycobacterium tuberculosis (TB) • Sputum AFB smear x3 ‐ negative C. Mycobacterium avium complex (MAC) • AFB blood cx drawn; started on empiric treatment for MAC D. Lymphoma • Restarted ART: Dolutegravir + FTC/ TDF - switched from FTC/TAF due to drug interaction with rifabutin When to suspect Mycobacterium avium complex Syndromic differential can help predict pathogens in patients with CD4<50 Clinical: • Fever, weight loss, +/‐ diarrhea, Short DDx in AIDS: Short DDx in AIDS: +/‐ abd pain Fever + wasting + lymphadenopathy AIDS + pulmonary nodules Laboratory: Tuberculosis Disseminated MAC • CD4 <50 Fungal (Crypto, Tuberculosis • Elevated alkaline phosphatase Coccidioidomycosis) Disseminated fungal (Histo, Crypto) • Anemia/pancytopenia due to bone Kaposi sarcoma Lymphoma Lymphoma marrow infiltration Diagnostics: Short DDx in AIDS: • AFB blood cultures* AIDS + prolonged diarrhea • Sensitivity 91% for 1 AFB BCx Parasites (cryptosporidium, microsporidium) • Sensitivity 98% for 2 AFB BCx Bacterial (Salmonella, Shigella), mycobacterial (MAC; TB ileitis) • CT abdomen often reveals HSM Viral : CMV colitis and intrabd. lymphadenopathy Fungal : Histoplasmosis • May need tissue bx Other : HIV enteropathy, Malignancy : lymphoma, Kaposi sarcoma (HHV8) Benson and Ellner. CID 1993. *draw prior to azithromycin 6 | [footer text here]
Recommend
More recommend