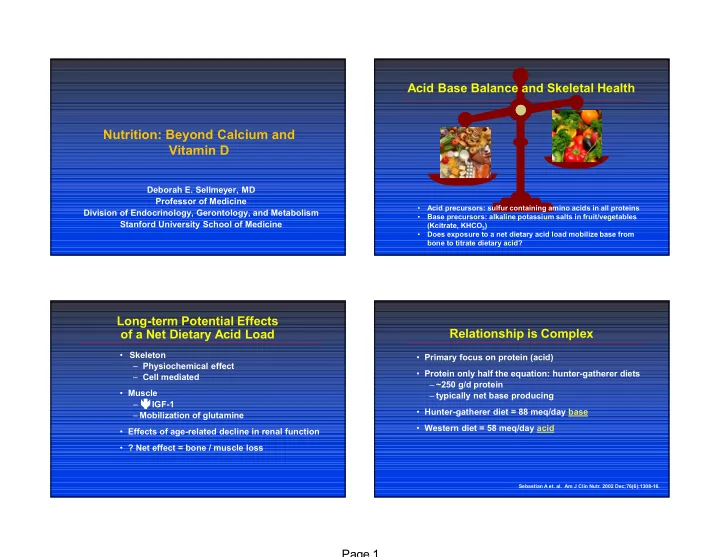
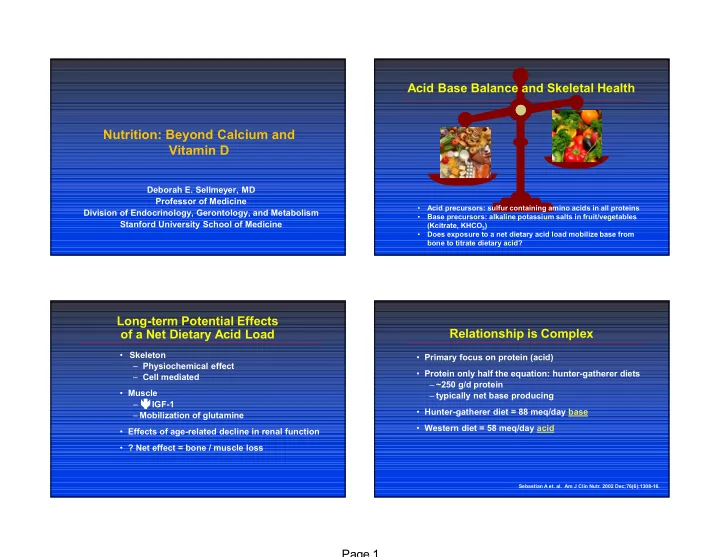
Acid Base Balance and Skeletal Health Nutrition: Beyond Calcium and Vitamin D Deborah E. Sellmeyer, MD Professor of Medicine • Acid precursors: sulfur containing amino acids in all proteins Division of Endocrinology, Gerontology, and Metabolism • Base precursors: alkaline potassium salts in fruit/vegetables Stanford University School of Medicine (Kcitrate, KHCO 3 ) • Does exposure to a net dietary acid load mobilize base from bone to titrate dietary acid? Long-term Potential Effects of a Net Dietary Acid Load Relationship is Complex • Skeleton • Primary focus on protein (acid) – Physiochemical effect • Protein only half the equation: hunter-gatherer diets – Cell mediated – ~250 g/d protein • Muscle – typically net base producing – IGF-1 • Hunter-gatherer diet = 88 meq/day base – Mobilization of glutamine • Western diet = 58 meq/day acid • Effects of age-related decline in renal function • ? Net effect = bone / muscle loss Sebastian A et. al. Am J Clin Nutr. 2002 Dec;76(6):1308-16. Page 1
Sulfur-containing AA (g) per 10g Protein Improving Dietary Acid-Base Balance spaghetti noodles • Option 1: Less acid haddock – Reduce dietary protein, cereal grains white rice – Protein important for peak bone mass, chicken skeletal maintenance, healing english muffin ground beef • Option 2: More base cottage cheese milk – Dietary (potassium-rich fruit / veggies) soybeans – Alkaline potassium supplements Grt North beans • Potassium bicarbonate peanut butter • Potassium citrate peas almonds 0.00 0.10 0.20 0.30 0.40 KCitrate and Long-term Calcium Balance Study Procedures • Randomized (stratified by gender) to 6 months of: • Dietitian counseled and monitored self-selected – Placebo (n=18) diet to 600 mg/d – Potassium citrate 60 mmol/day (n=18) • Calcium and vitamin D – Potassium citrate 90 mmol/day (n=17) – 600 mg dietary calcium • NAE Western diet = 50-75 mmol/day – 630 mg calcium citrate – 400 IU vitamin D • Baseline and Month 6 – 12 days controlled diet • Two week run-in – Calcium balance: days 7-12 complete urine – Calcium 1230 mg/d (diet + supplements) and stool collections in 24 hour increments – Vitamin D 400 IU/d = dietary calcium intake – (urine calcium + fecal calcium) – Placebo (identical to KCitrate): 3 pills, 3 times / day – Fractional calcium absorption (oral / IV stable isotopes) Page 2
Subject Characteristics Net Acid Excretion Net acid excretion K Citrate K Citrate (meq/day) Placebo 60 mmol/day 90 mmol/day (n=18) 40 (n=17) (n=17) 30 Age (years) 65.2 + 6.2 64.7 + 5.9 63.8 + 6.4 NAE = (Titratable Acid + NH 4 ) – HCO 3 20 Gender (% female) 67% 67% 73% 10 Race (% Caucasian) 83% 100% 78% 0 BMI (g/m 2 ) 26.0 + 4.0 25.1 + 2.7 24.3 + 3.3 -10 Placebo * KCitrate 60 mmol/day -20 Urine calcium (mg/day) 184 + 59 206 + 94 189 + 82 KCitrate 90 mmol/day -30 25-hydroxyvitamin D (ng/ml) 36 + 10 31 + 10 32 + 10 * -40 No significant differences at baseline. *p<0.05 compared to placebo Calcium Absorption and Balance 6 Month Intervention Markers of Bone Turnover Change in urine calcium Change in fractional Change in calcium K Citrate K Citrate excretion (mg/day) calcium absorption (%) balance (mg/day) Placebo 60 mmol/day 90 mmol/day 40 10 250 * BsAP (μg/L) 8 200 20 Baseline 11.8 + 1.3 11.8 + 1.3 11.3 + 1.1 6 150 0 4 100 Change -0.95 + 0.8 -1.1 + 0.9 -1.8 + 0.8 -20 2 50 Serum CTX (ng/ml) -40 0 0 Baseline 0.19 + 0.04 0.25 + 0.03 0.25 + 0.04 -60 * -2 -50 Change 0.04 + 0.03 -0.07 + 0.04 a -0.03 + 0.04 a -80 -4 -100 * -6 -150 -100 a p<0.05 vs. placebo Placebo *p<0.05 compared to placebo KCitrate 60 mmol/day KCitrate 90 mmol/day Moseley KF, et al. J Bone Miner Res. 2013 Mar;28(3):497-504. Moseley KF, et al. J Bone Miner Res. 2013 Mar;28(3):497-504. Page 3
KCitrate and BMD KCitrate and BMD 0.0 161 postmenopausal women KCl 2-year BMD change (%) 30 mmol/day KCitrate -0.5 -1.0 + 1% KCitrate 55.5 mmol + 1% KCitrate 18.5 mmol -1.5 0% 1.9% Placebo 2.0% 0% p<0.001 -2.0 p<0.001 Fruit / Veggies - 1% - 1% -2.5 - 2% -3.0 Lumbar Spine Total Hip 3 Months 6 Months 9 Months 12 Months 276 postmenopausal women Lumbar Spine Total Hip KCitrate 55.5 mmol/d, 18.5 mmol/d, fruit / veggies, placebo No effect BMD, urine calcium Macdonald HM, et al. Am J Clin Nutr. 2008 Aug;88(2):465-74 Jehle S, et. al. J Am Soc Nephrol. 2006 Nov;17(11):3213-22 L2-L4 KCitrate and BMD 3 n=91 n=87 n=86 n=84 2.5 Isoflavones/Soy †† 2 †† % Change in BMD 1.0 † xx xx 1.7% 1 xx (1.0-2.3) • Plant compounds (phytoestrogens) found in 0.5 N=201 0 soybeans, clover, alfalfa sprouts -0.5 60% female n=91 n=87 n=86 n=85 -1 25(OH)vit D = 24 + 8 ng/ml • Studies on bone health mixed -1.5 -2 L Spine T-score = -0.6 + 1.5 – Interventions varied 0 6 12 18 24 Kcitrate Months – Different compounds may offset each other Placebo Kcitrate 60 mmol/day vs. pbo – Effects may depend on proximity to menopause Total Hip NAE negative on Kcitrate 2 1.5 – Equol producers n=91 n=87 n=86 n=84 % Change in BMD 1 † † † ↑ trabecular thickness, – 2 placebo controlled RCTs neg 0.5 xx x 1.0% x 0 number on QCT. (0.5-1.5) -0.5 n=90 n=87 n=86 n=85 -1 -1.5 -2 0 6 12 18 24 x=p<0.05; xx=p<0.001, Kcitrate vs. placebo Kcitrate †=p<0.05;††=p<0.001, compared to baseline Months Placebo Jehle S, et. al. J Clin Endocrinol Metab. 2013 Jan;98(1):207-17. Page 4
Sodium Chloride Phosphorus • dietary NaCl urine calcium, bone resorption • Essential for bone building and growth Relationship to Skeleton • 85% of body’s P bound to skeleton • Effects on fracture not known • Excess PO4 PTH ? bone resorption The Issues • Dietary K and base (fruit and vegetables) offset • Typical intakes > RDA (700 mg/day) NaCl effects • PO4 intake ’ing due to preservatives • High dietary Ca absorption dietary PO4 • High salt foods: – prepared foods--jars, cans, boxes, bottles Sources • Meat, poultry, fish, eggs, dairy, nuts, legumes, – condiments, sauces cereals, grains, cola – cheese, bread Bottom Line • Typical intakes (1000-1500 mg/day) prob OK unless – restaurants dietary Ca low • Current RDA: 1500mg/day; AHA rec: 2400mg/day • Poor overall nutrition = low PO4 intake • ? important during anabolic osteoporosis tx Magnesium Iron • Essential for bone formation Relationship Relationship • Co-factor for enzymes involved in collagen synthesis • 2/3 of body’s Mg in skeleton (surface) to Skeleton to Skeleton • Impt for proper crystal formation during mineralization • bone strength Fe deficient rats The Issues • Deficiency impairs PTH secretion hypocalcemia, The Issues • Fe absorption decreased by other minerals esp Ca vitamin D resistance • Fe overload states associated with trabecular • Typical intakes < RDA volume, number, thickness • RDA 320 mg women, 420 mg men, +35 mg preg Sources • Dark green veg, spinach, red meat • Whole grains, green vegetables, squash, nuts, seeds, Sources “hard” water • Separate Fe and calcium supplements Bottom Line • Unclear how much of bone deficits in overload states • Typical intakes appear low Bottom Line due to Fe itself • EtOH Mg wasting • Effect on skeletal health not clear Page 5
Zinc Copper Relationship • Co-factor for enzymes involved in collagen synthesis Relationship • Involved in collagen maturation, cross linking to Skeleton and mineralization to Skeleton • bone formation Zn deficient rats • Typical intakes < RDA The Issues The Issues • Low Zn levels associated with osteoporosis in humans • Cu deficiency assoc with osteoblast function • Zn supplements improved BMD in rats • Trace mineral supplement incl Cu increased BMD • Red meat, poultry, fish, oysters, eggs, legumes, whole Sources • Legumes, nuts, mushrooms, liver, oysters, cereals, Sources grain breads, milk chocolate • Zn stims osteoblasts, bone formation in animal studies • Need human intervention studies Bottom Line Bottom Line • EtOH Zn wasting • Need human intervention studies Vitamin A and Carotenoids Vitamin B12 Relationship • Vitamin A involved in bone remodeling process Relationship • May effect osteoblast function/activity to Skeleton • Animal foods: retinol; vegetables: carotenoids to Skeleton • Excess and deficiency Vit A skeletal fragility • Low serum B12 associated with BMD, bone loss, The Issues The Issues • intakes/ serum retinol levels associated with BMD, fracture in most human studies fracture in some human studies • Supplementation with B12 and folate in CVA • β-carotene, lycopene, leutein assoc with BMD, population hip fracture risk (RCT) bone loss, hip fracture Sources • Fish, shellfish, meat, poultry, eggs, milk Sources • red/orange/yellow vegetables (β-carotene), dark green • Be alert to states associated with B12 Bottom Line veg (lutein), tomatoes, watermelon (lycopene), liver, – Vegan dairy products, fish – Pernicious anemia Bottom Line • Avoid excess or insufficient Vit A intake (3000 IU per – Gastric bypass day in supplements) – Atrophic gastritis (up to 40% elderly) • Vegetable sources also provide antioxidants – Celiac, Crohn’s, other GI disease Page 6
Recommend
More recommend