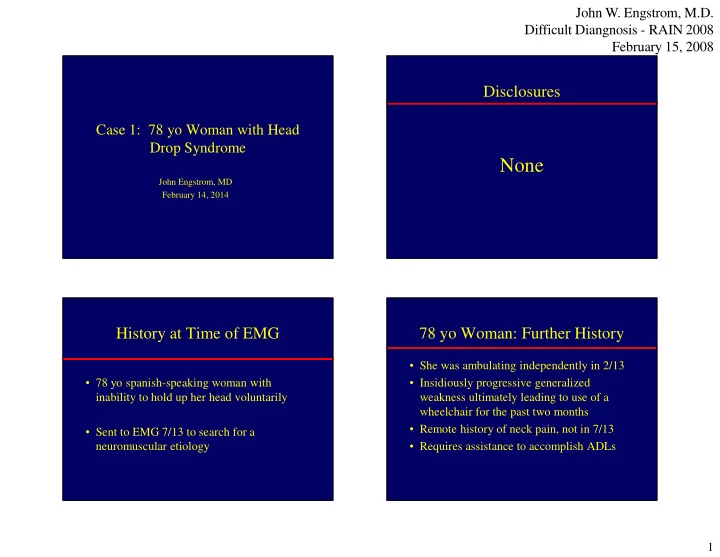
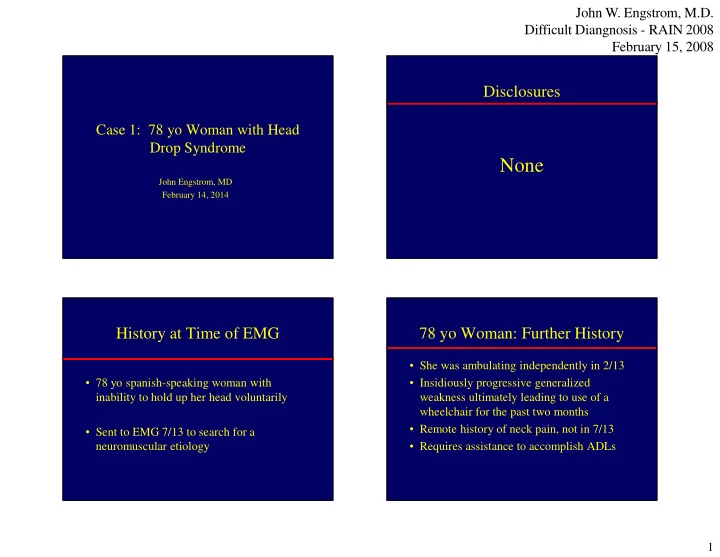
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 Disclosures Case 1: 78 yo Woman with Head Drop Syndrome None John Engstrom, MD February 14, 2014 History at Time of EMG 78 yo Woman: Further History • She was ambulating independently in 2/13 • 78 yo spanish-speaking woman with • Insidiously progressive generalized inability to hold up her head voluntarily weakness ultimately leading to use of a wheelchair for the past two months • Remote history of neck pain, not in 7/13 • Sent to EMG 7/13 to search for a neuromuscular etiology • Requires assistance to accomplish ADLs 1
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 Q!-Which of the following is the least Pre-EMG Neuro Exam likely cause of a head drop? • CN normal, including normal tongue power 1. ALS and bulk bilaterally 2. Myopathy • Sensory-identifies light touch in all 4 limbs 57% 3. Myasthenia gravis • Motor exam 4. CIDP – SOB supine, better with partial sitting up 23% 5. An upper motor neuron process – Arm >> leg weakness 9% – Unable to walk or stand 6% 6% – Unable to hold neck in extension; not painful ALS Myasthenia gra... CIDP Myopathy An upper motor... Head Drop Syndrome: Head Drop Syndrome: DDx Neuromuscular Etiologies • Anterior horn cell-ALS • Kyphotic deformity of the cervical spine • Nerve-CIDP, GBS – Orthopedic • Neuromuscular junction-MG • Listhesis with or without endogenous fusion • Anterior wedging vert bodies • Myopathy-inflammatory, mitochondrial, – Dystonic-anterocollis, Parkinsonian syndromes dystrophy, other – Neuromuscular-weakness of the cervical Isolated head drop uncommon-most assoc paraspinal muscles with other findings on neurologic exam 2
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 Head Drop and Camptocormia Q2-Which choice below is not a limitation to the clinical assessment of paraspinal muscles? • Classic: Flexion of the thoracolumbar spine 1. Cannot test muscle power attributable to a • Greek Kamptos (bend) and Kormos (trunk) specific segmental level • 1818-Brodie suggests destructive spine 2. Inaccessible for muscle biopsy disorders or hysterical reaction 28% 28% 3. There are no norms for the degree of fatty 24% • Consid psychogenic until latter 20 th century 20% muscle replacement on MRI with age • May be associated with head drop, but 4. Pathologists do not know the range of normal anatomy for paraspinal muscles should consider other causes Azher SN, Jankovic J. Neurology 2005;65:355-59 . . . . . . . . . u . f . . n d m e l o s b n t s t i s s e g i e s r o t e a t c l o c e o a r h n n e t n a a I h T P C Neurologic Assessment of the Electromyographic Assessment Paraspinal Muscles of the Paraspinal Muscles • Neurologic exam is insensitive to assess • Can directly assess muscle function with paraspinal muscles-neck ext, T/L posture needle EMG recording and activation of muscles by extension of the neck • MRI can detect fatty replacement of muscle • Detects short dur motor units (myopathy or – Fatty replacement increases with age nmj) or long duration units (nerve/AHC) – Lack of control groups corrected for age • Limitations: overlapping innervation at a • Little muscle biopsy normal data given level, incomplete muscle relaxation • Ultrasound-future use to direct muscle biopsy in the OR 3
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 Q3-In general, what is the Least Likely Cause 78 yo woman: EMG findings Diminished Firing Frequency of MUAPs? • NCS right CTS; no other segmental nerve 1. Lack of effort conduction slowing or conduction block 2. An upper motor neuron process • Sural 11 microvolts-normal 3. Pain associated breakaway 32% 29% 29% • Needle EMG: absence of fibrillations, weakness myopathic or neurogenic motor units 4. Inattentiveness • Needle EMG: diminished motor unit 11% firing frequency in all muscles-no pain, no breakway weakness, constant effort t . . . r . . . . . o . e s r t e f f o a e t n o c i e f m o v o s t i k r s n e a c e a p n t L p t u a i a P n n I A Additional Neurologic Exam Findings EMG: Diminished Firing Frequency • Normal tone in the arms and legs • Power: Arms-barely antigrav prox, weaker • Needle EMG notable for diminished firing distally; Legs 4- quadriceps bilat 2s distally frequency (“diminished suprasegmental activation of motor units”) is due to: • Slowed FFM and foot taps-but very weak – Poor effort-not apparent in this patient; effort • Hyperactive leg and arm reflexes-normal constant in all muscles jaw jerk – Pain-not present in this patient during the test • Bilateral Babinski signs – An upper motor neuron process • No sensory level 4
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 78 yo woman: Cervical spine MRI “Normal” Cervical Spine MRI Abnl Cervical MRI Findings • Anterolisthesis of C2 on C3 and C4 on C5 • Loss of normal cervical lordosis ( kyphosis ) • Marked narrowing of the cervical spinal canal due to soft tissue or bone • Abnormal signal at level of the compression “Normal” Cervical Spine CT 5
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 78 yo woman: Cervical CT Findings • Confirms bony canal narrowing rather than soft tissue • C1-C2: The anterior atlantodental interval is increased and measures 5.5 mm • Autofusion of C1 to C2 • Anterolisthesis of C2 on C3 by 4 mm 78 yo woman: Cervical Spine CT Sensitivity of abnormal signal for Operative report compressive myelopathy • “Approximately 75%” • Pre-Op diagnosis: C1-C2 subluxation and severe stenosis with cervical kyphosis and • If neuro exam shows progressive myelop spinal cord contusion at C1-C2 and radiology severe spinal stenosis (but no • Procedure: suboccipital craniectomy; C1 increased signal) then decompress and C2 laminectomy; occiput to C5 • How distinguish cortical vs. upper cervical- posterior cervical fixation and possible use of DTI or other imaging posterolateral fusion; 6
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 Case 2: 61 yo man with acute Clinical Course painful neuropathies • Able to stand with assistance at discharge • 4/05-painful left radial neuropathy-resolved over months • 10/13 using a walker, no SOB, more independent for ADLs • 6/06-C3-4 spinal fusion; awake 1 mo later with SOB-bilateral phrenic nerve palsies • 12/13 using a cane • 11/11 numbness and shocks over the toes of • Continues to improve L foot; VA EMG-mononeurop multiplex Q4-In general, what is the least likely cause of Mononeuropathy multiplex mononeuropathy multiplex? • Axonal injury to multiple single nerves 1. Leprosy • Worldwide-leprosy, diabetes 2. Diabetes • Other- vasculitis , sarcoid, AIDP/CIDP, mult 61% 3. Vasculitis entrapments, lyme, leukemia, lymphoma 4. Brachial neuritis • Nomenclature confusing: Early GBS/CIDP? 24% Polyradiculopathy? Ulnar neuropathy and 12% CTS? Brachial neuritis? 2% • Only 20% with 2+ specific nerves by exam Leprosy Diabetes Vasculitis Brachial neuri... 7
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 Case 2: 61 yo man with acute Mononeuropathy Multiplex painful neuropathies • 2/3 appear by clinical exam to have distal • 3/12-Decr light touch, pin entire left foot polyneuropathy; asymmetry on EMG • EMG-mild L peroneal/sciatic axonal neurop • Diagnosis-Search for systemic illness assoc • 10/12 Right upper arm pain that tapered with vasculitis; consider nerve biopsy over several months; new R arm weakness • Exclude focal neuropathies at sites prone to • Recalled similar event L arm 20 yrs ago compression • Motor Ex-power R arm deltoid 0, SS 3, IS 3, biceps 5; biceps reflex R 1, L 2 • Sens-Decr light touch over R lateral deltoid Q5-What would your predict was Hereditary Brachial Neuritis: the next diagnostic step? Similarities to Classic Form 1. Another EMG • Triggers-infections, immunizations, surgery, parturition 2. Blood tests to search for vasculitis 49% • Symptoms at onset-severe pain followed by 3. Genetic testing focal weakness and muscle atrophy 4. Joint psychiatry referral for a 31% • Spontan, slow recovery between attacks frustrated patient and neurologist • Management-persistent pain, rehab for focal 14% 5. Refer to the Mayo Clinic motor loss of function 4% 2% Genetic testin... Another EMG Blood tests to... Joint psychiat... Refer to the M... 8
John W. Engstrom, M.D. Difficult Diangnosis - RAIN 2008 February 15, 2008 Hereditary Brachial Neuritis Hereditary Brachial Neuritis • Genetic variations: • SEPT 9 gene mutation-autosomal dominant; – Whole gene duplication, partial gene duplic chromosome 17 (17q25) – Mapped to other loci on chromosome 17 • Unususal Clinical Features-episodes that are pain – 15% of US families do not map to SEPT9 only, weakness only, painless attack (5%), CN involvement, or lumbar plexus • Genetic Counseling • Phrenic nerve in 14% – Penetrance 80-90% • Diagnosis: 1) Recurrent attacks 2) positive family – Identify who at risk does not have the mutation history 3) positive genetic testing (Athena) – Cannot predict when symptoms will occur Moral of the Story The smartest neurologist is the last one to see the patient! 9
Recommend
More recommend