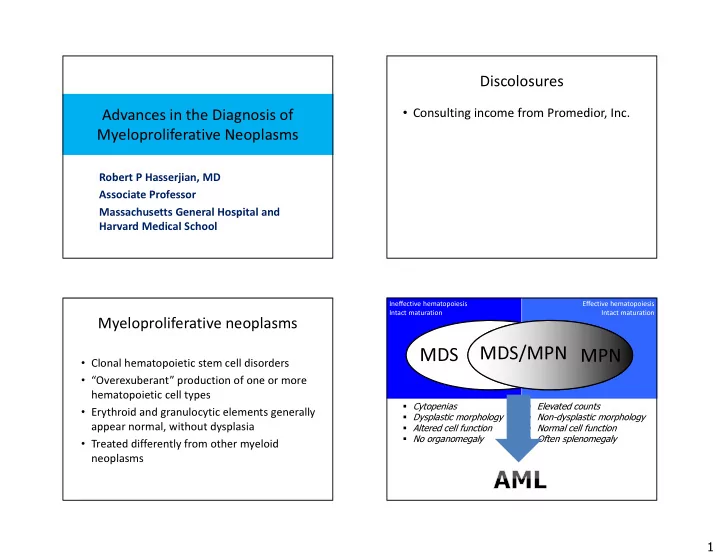
Discolosures • Consulting income from Promedior, Inc. Advances in the Diagnosis of Myeloproliferative Neoplasms Robert P Hasserjian, MD Associate Professor Massachusetts General Hospital and Harvard Medical School Ineffective hematopoiesis Effective hematopoiesis Intact maturation Intact maturation Myeloproliferative neoplasms MDS/MPN MPN MDS • Clonal hematopoietic stem cell disorders • “Overexuberant” production of one or more hematopoietic cell types � Cytopenias � Elevated counts • Erythroid and granulocytic elements generally � Dysplastic morphology � Non-dysplastic morphology appear normal, without dysplasia � Altered cell function � Normal cell function • Treated differently from other myeloid � No organomegaly � Often splenomegaly neoplasms 1
Diagnostic issues with MPN Chronic myeloproliferative • Distinguishing MPN from reactive conditions neoplasms (WHO 2016) • Chronic myeloid leukemia, Ph+ that can produce elevated counts BCR-ABL • Polycythemia vera • Separating MPN from other myeloid neoplasms JAK2 • Essential thrombocythemia MPL (MDS and MDS/MPN) • Primary myelofibrosis CALR • Providing a specific diagnosis • Rare entities – Chronic neutrophilic leukemia – Requires integration of clinical and molecular CSF3R – Chronic eosinophilic leukemia/hypereosinophilic syndrome genetic data with morphology – Myeloproliferative neoplasm, unclassifiable – Important in predicting prognosis and dictating therapy PDGFRA • Recognizing signs of progression Genetically defined eosinophilic neoplasms PDGFRB FGFR1 PCM1-JAK2 CML The Philadelphia chromosome • Hematopoietic stem cell neoplasm associated with BCR-ABL1 fusion gene • Patients present with neutrophilic leukocytosis Y412 with morphologically normal and maturing granulocytic elements BCR-ABL fusion proteins p190 • Natural history is that of genetic instability, p210 with progressive accumulation of blasts p230 culminating in acute leukemia 2
CML peripheral blood Sequelae of BCR-ABL1 • Growth advantage with progressive colonization of marrow at the expense of normal cells – Marked hypercellularity (typically 90-100%) • Overproduction of granulocytes, eosinophils, and basophils, underproduction of erythroids • Increased small, hypolobated megakaryocytes • Decreased cell retention in marrow – Leukocytosis with circulating immature myeloid forms – Basophilia and eosinophilia – Often thrombocytosis CML bone marrow aspirate CML bone marrow biopsy 3
CML bone marrow biopsy Natural course of CML • Patients may survive many years with relatively few symptoms • Inexorably progress to an acute leukemia with loss of differentiation – Termed ‘Blast crisis’ or ‘Blast phase’ – Blast crisis phenotype • 70% myeloid ( ≥20% BM/PB myeloblasts) • 30% B-lymphoid ( any BM/PB lymphoblasts raises strong supsicion) CML in blast crisis CML in the 20 th century Bela Bartok (1881-1945) • Therapies generally ineffective at delaying progression • Blast crisis very aggressive with short survival • Bone marrow transplant offered only cure 4
Tyrosine kinase inhibitors CML in the 21 st century • Treated very effectively with tyrosine kinase inhibitors (TKI) – Imatinib mesylate, nilotinib, dasatinib, bosutinib, ponatinib • Disease progression no longer inevitable • Patterns of disease evolution closely linked to responsiveness (versus resistance) to TKI therapy Faderl S et al. N Engl J Med 1999;341:164-172, Goldman J and Melo J. N Engl J Med 2003;349:1451-1464 Criteria for accelerated phase Role of pathology in the current era of CML management • At the time of initial diagnosis of CML – Get the diagnosis right! – Provide prognostic information • At later timepoints, determine any progression and evaluate for other pathologic processes while on therapy **Even small numbers of neoplastic B-lymphoblasts may indicate impending blast crisis 5
Required at diagnosis Caveats with CML diagnosis • Bone marrow biopsy and aspirate • Relatively low M:E ratio in patients with – Reticulin stain to assess baseline fibrosis hemoglobinopathies • Prominent thrombocytosis mimicking ET level – Blast count (may be higher in marrow than • Minimal or no myeloid left-shift in blood blood) • Monocytosis mimicking CMML • Full karyotype of bone marrow • Blast crisis mimicking AML or ALL – Splenomegaly, basophilia, cytogenetic clues help – Karyotype/FISH of blood may not pick up all differentiate CML blast crisis from Ph+ AML or B-ALL abnormalities • +8, double Ph, +19, i(17q) • CBC and review of peripheral smear – Ph+ AML will be a new genetically-defined AML – Blast and basophil count subtype in the 2016 WHO update Erythroid-rich CML 73 yo man WBC 13.3, HGB 14.0, PLT 1,483 56% polys 28% lymphs 4% monos 9% basos 2% eos 6
Chronic neutrophilic leukemia • Rare MPN with leukocytosis (>25 x 10 9 /L) – No dysplasia (hypogranulation) of neutrophils – Splenomegaly – <10% immature myeloid cells in blood – No BCR-ABL1 rearrangement – No significant basophilia or eosinophilia • 83-89% have CSF3R mutation 46, XY, t(9;22)(q34;q11.2) in all 20 metaphases RT-PCR showed p230 BCR-ABL1 transcript Gotlib J et al. Blood 2013;122:1707, Pardanani A et al. Leukemia 2013;27:1870, Maxson JE et al. NEJM 2013;368:1781 7
Chronic neutrophilic leukemia: peripheral blood smear Chronic neutrophilic leukemia: peripheral blood smear WBC 36.7 x 10 9 /L HCT 40.0% (MCV 98 fL) PLT 253 x 10 9 /L 82% polys, 14% lymphs, 2% metas, 2% myelos Chronic neutrophilic leukemia: bone marrow aspirate Chronic neutrophilic leukemia: bone marrow biopsy 8
Pathologic differential diagnosis of Algorithm for workup of persistent neutrophilia neutrophilia Disease Peripheral counts Neutrophil Genetics Possible reactive Pathologist has a causes excluded? morphology critical role in evaluating smear and Normal t(9;22); BCR-ABL1 CML, BCR-ABL1+ ↑ Granulocytes with biopsy morphology and left-shift Secondary reactive Usually self-limited to integrate these neutrophilia Eosinophilia findings with clinical Basophilia and genetic findings! Atypical CML, ↑ Granulocytes with Dysplastic SETBP1 mutation(30%) Karyotype, FISH, BCR-ABL + BCR-ABL1 - and/or RT-PCR BCR-ABL1- left-shift Chronic ↑ Granulocytes without Normal CSF3R mutation (90%) Significant JAK2 mutation and CSF3R mutation and neutrophilic left-shift CML granulocytic left- typical bone no dysplasia or left- leukemia shift and dysplasia? marrow findings? shift? Leukoerythroblastic Normal Primary JAK2 , MPL, or CALR Treat with TKI mutations (90%) myelofibrosis immediately to Atypical CML, BCR- Primary Chronic neutrophilic prevent progression ABL1- myelofibrosis leukemia Poor prognosis, Several treatment May respond to difficult to treat options ruxolitinib Eosinophilia Neoplastic eosinophilias • Eosinophils are part of a myeloid stem cell • Reactive neoplasm – Allergy, drug, parasitic or other infections – CML • Paraneoplastic (non-neoplastic eosinophils – AML with inv(16) – Rare MDS cases stimulated by tumor cytokines) • “Primary” eosinophilias – Hodgkin lymphoma – Rearrangement of PDGFRA – T-cell lymphomas – Rearrangement of PDGFRB • May be a very small clonal T-cell population (without – Rearrangement of FGFR1 overt T-cell lymphoma) – PCM1-JAK2 rearrangement (new entity in 2016) – Systemic mastocytosis – Chronic eosinophilic leukemia, not otherwise – ALL with t(5;14) specified • Translocation of IL-3 gene 9
Myeloid and lymphoid neoplasms with Myeloid/lymphoid neoplasms with eosinophilia and abnormalities of PDGFRA rearrangement PDGFRA , PDGFRB , or FGFR1 • Patients present with chronic eosinophilia and elevated • Share similar molecular and biologic features serum tryptase levels – Appear to involve pluripotent stem cell with both • Bone marrow mast cells are increased, but are diffuse lymphoid and myeloid differentiation capacity and not aggregated – Translocations activate genes encoding tyrosine • Small interstitial deletion at 4q12 fuses FIPL1 gene to kinases PDGRFA , a tyrosine kinase – Eosinophilia is characteristic – Cannot be detected by cytogenetics, must request FISH or PCR • Most entities respond to Gleevec and related – Should be sought in all cases of idiopathic hypereosinophilia – Excellent response (100%) to Gleevec and related TKI tyrosine kinase inhibitors Myeloid/lymphoid neoplasm with PDGFRA rearrangement Myeloid/lymphoid neoplasms with with PDGFRB rearrangement • Usually resemble CMML – Persistent monocytosis – Eosinophilia (almost always) – Dysplasia in one or more myeloid lineages • Rearragned PDGFRB at 5q33 (multiple partners) CD117 – t(5;12) ETV6-PDGFRB most common • TKI inhibits these fusion proteins and these patients respond to Gleevec therapy • Evaluation for PDGFRB rearrangement is indicated for cases of CMML with eosinophilia Courtesy of Tracy George, 39 University of New Mexico 10
Recommend
More recommend