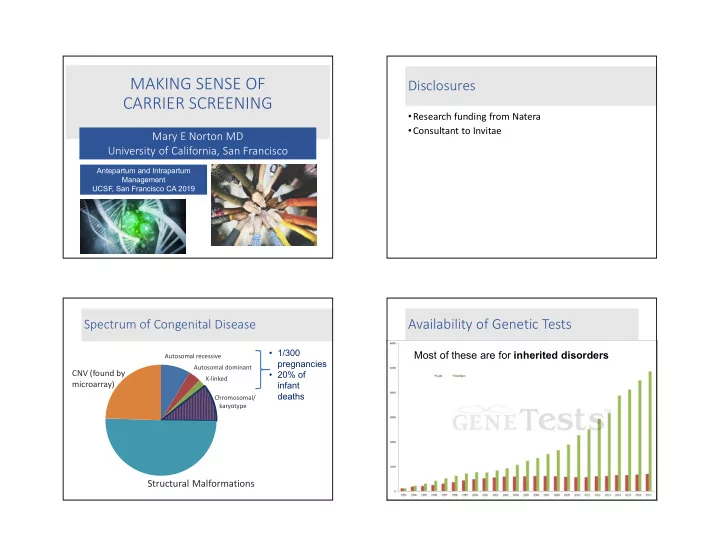
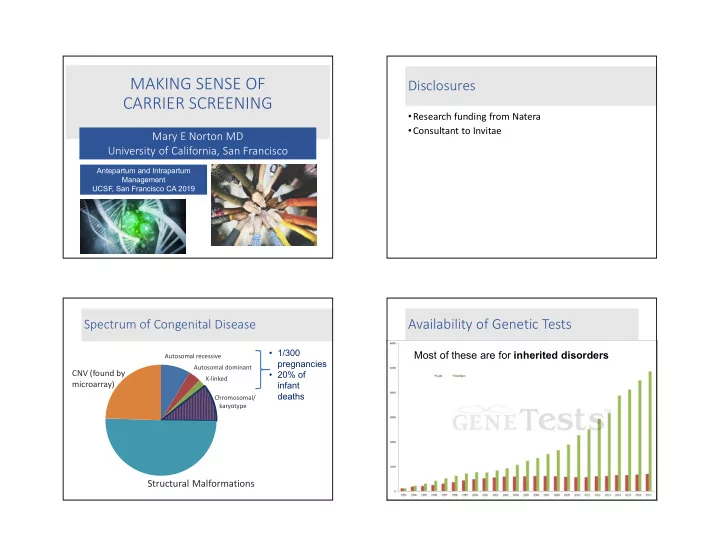
MAKING SENSE OF Disclosures CARRIER SCREENING • Research funding from Natera • Consultant to Invitae Mary E Norton MD University of California, San Francisco Antepartum and Intrapartum Management UCSF, San Francisco CA 2019 Availability of Genetic Tests Spectrum of Congenital Disease Spectrum of Congenital Disease • 1/300 Most of these are for inherited disorders Autosomal recessive pregnancies Autosomal dominant CNV (found by • 20% of X-linked microarray) infant deaths Chromosomal/ karyotype Structural Malformations
Recessive inheritance Recessive inheritance Affected Affected Unaffected carriers Unaffected carriers What is the purpose of prenatal What is the purpose of newborn carrier screening? screening?
Screening for Screening for Affected Carriers NEWBORN PRENATAL Carrier Newborn screening screening Wilson and Junger: History of Prenatal Carrier Screening Criteria for screening for disease 1. Hemoglobinopathies 1970’s • A good test is available 2. Tay Sachs disease 1971 • The disorder is common 3. Canavan disease 1998 • The disorder is severe 4. Cystic fibrosis 2001 5. Familial dysautonomia 2004 • There is an intervention 6. Spinal muscular atrophy 2008 (ACMG) • Testing is voluntary and patients give 7. Spinal muscular atrophy 2017 (ACOG) informed consent 8. Expanded Jewish panel 2008 (ACMG) 9. Expanded Jewish panel 2017 (ACOG) 10. Expanded carrier screening 2017 (ACOG)
Traditional Carrier Screening Ethnicity Based Screening • Focus on ancestry and family history Ashkenazi Jews Tay Sachs disease, Canavan • Small number of diseases disease, cystic fibrosis, • High frequency in a certain population familial dysautonomia • Severe morbidity or mortality • Fetal, neonatal or early childhood onset Louisiana Cajun, Tay Sachs disease • Well-defined phenotype Fr Canadian Caucasians Cystic fibrosis Sickle cell disease Tay-Sachs disease Africans, African Sickle cell anemia, beta Americans thalassemia Southeast Asians Alpha thalassemia Mediterraneans Beta thalassemia ACOG 2017 Updated Screening ACOG 2017 Updated Screening Recommendations Recommendations • Screening should be offered to all women before or • Fragile X screening should be offered to during pregnancy for: all women with: • Cystic fibrosis • a family history of FraX related disorders • Spinal muscular atrophy • unexplained ovarian insufficiency or failure • MCV should be offered to all women who are • Tay Sachs screening should be offered currently pregnant to those who are: • To those at risk for hemoglobinopathies , Hb • French Canadian electrophoresis should be offered (African, • Cajun Mediterranean, Middle Eastern, SE Asian, West • Ashkenazi Jewish Indian) or if MCV is low
ACOG 2017 Updated Screening Expanded (Universal) Carrier Screening Recommendations It is reasonable to do: • Ethnicity based screening • Pan-ethnic screening • Same tests are offered to everyone • Expanded carrier screening Expanded Carrier Screening Multiplex Panel Screening: Expanded Carrier Screening Utilization of new technologies to identify • Multiplex screening now allows testing for carriers of multiple genetic conditions many (>100) disorders at once simultaneously • This is relatively inexpensive (~$350) • Should it be offered to everyone?
Is More Better? Newborn vs prenatal screening • What are these additional conditions? • What is the process for adding new Disorder is important test is developed and introduced conditions? • Is the test accurate? • How often does the test find Technology is developed test is something? introduced • What happens then? What is on expanded panels and how Newborn Screening are disorders chosen? • Disorders chosen by Health Resources and Disorders should be: Services Administration (HRSA) • Severe • Recommended Uniform Screening Panel • Common • Cause serious health problems if treatment is • Have a well-described natural history not started shortly after birth and phenotype • Identification and management of these • Have a high detection rate conditions may prevent life-threatening complications
What criteria are required by laboratories before adding gene variants to panels? Alpha 1 antitrypsin deficiency Achromatopsia Chronic Obstructive Pulmonary Disease • Decreased visual acuity, nystagmus • Smoking influences the onset of COPD • Non-smokers often have a normal life span • Increased light sensitivity • Extremely rare in children • Decreased color discrimination Liver disease – increased risk with age • Adults – Cirrhosis 15-20% by age 50 • Non-progressive • Children -- obstructive jaundice • Does not lead to blindness • 2% liver failure • No other organ system affected • Hepatocellular carcinoma - rare Clinical disease is infrequent in heterozygote state • Smoking increases risk • Should this be on panels? Would most consider prenatal diagnosis?
Other mild/minimal/non-disorders • 23,453 patients screened Condition 1/ for 96 conditions α1AT deficiency 13 MTHFR Hemochromatosis • Mild conditions excluded: • Elevated homocysteine • Inappropriate absorption of hemochromatosis ( HFE) Cystic fibrosis 28 • Risk for thrombosis, iron MTHFR • Clinical – end organ failure cerebrovascular and DFNB1 43 others cardiovascular disease, stroke • Onset: >40 years SMA 57 • Treatment: vitamins • 75-90% - asymptomatic Fam Mediterranean Fever 64 SLO 68 Because we “can” should we be offering carrier SS/ β-thal 70 screening? Gaucher disease 77 o Which may lead to partner carrier screening…. Anxiety Factor XI deficiency 92 o Prenatal diagnosis…. Achromatopsia 98 “First, do no harm” Lazarin GA, et.al.. Genetics in Med 2012. Expanded Carrier Screening: Gene variants The Wild West What criteria are required by laboratories before adding variants to panels? Test is available
Optimal criteria for carrier screening: ACMG and ACOG • Good test is available • Detection rate ≥ 70% • Carrier frequency is high • At least 1 in 100 • Exclusions: • Adult onset • Poorly studied • Prevalence unknown • Incomplete penetrance • Mild phenotype Which conditions should be included? • Includes conditions for which carrier screening of the general population is NOT recommended • Factor V Leiden, Fragile X, hemochromatosis • Include conditions with significant variation in their presentation • Age at onset • Severity • Evaluated commercially available panels • Includes rare conditions with unknown detection rates • 27% of included disorders meet criteria and carrier frequencies and uncertain natural history • Counseling about likely phenotype difficult per ACMG and ACOG • Calculation of residual risk may not be possible
How accurate is the test? Other Limitations and Challenges Molecular DNA testing is not the recommended Individuals with a positive family history screening approach for certain conditions • Family-specific mutations may not be on • Tay-Sachs disease commercially available panels • Hexosaminidase A enzyme analysis is best test for • Genetic counseling should be considered non-Jewish individuals • Hemoglobinopathies before offering ECS • Gold standard is MCV and hemoglobin electrophoresis • Carrier screening platforms do not include all mutations for alpha and beta thalassemia How Often Do Tests Find Something? What Then? 24-45% will have something • Explain to the patient • Test the partner (he might not have insurance) • He will often have something else • If low detection rate on original panel, do gene sequencing • Explain all this to the patient
A real patient story • Patient reports that she carries SMA • Partner has expanded carrier screening through panel covered by his insurance Carries Fanconi Anemia, group A • Patient undergoes expanded carrier screening with panel covered by her insurance She carries Pompe disease but was not tested for Fanconi group A, just group C (updated panel) • They are frustrated and seek a second opinion • He undergoes gene sequencing for Pompe and she has sequencing for Fanconi group A • All he really needed was testing for SMA Another patient story • Patient and partner had expanded carrier screening during first pregnancy (in NY) • Both carried a variant for Zellweger disease • Life-threatening metabolic disorder • Usually neonatal death • Had prenatal diagnosis: fetus carrier
Delayed pregnancy for THREE years Results • Saw GC for pre-conception counseling • Planning for preimplantation genetic testing • GC was having a slow day…. Researched this variant Results (Page 2 of report, fine print) • ClinVar (public database) • 2 labs: pathogenic or likely pathogenic • 1 benign • 1 VUS (variant of uncertain significance) • Gnomad (another genome database) • 8 individuals who were homozygous and presumably normal • PubMed • Called a researcher, who said that variant should be reclassified as benign
Recommend
More recommend