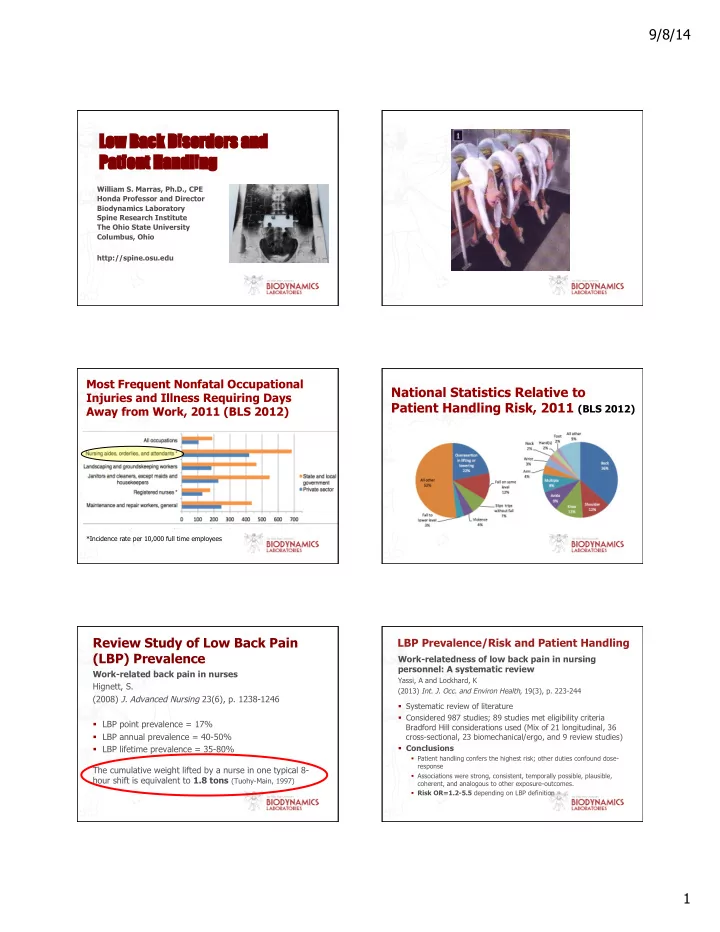
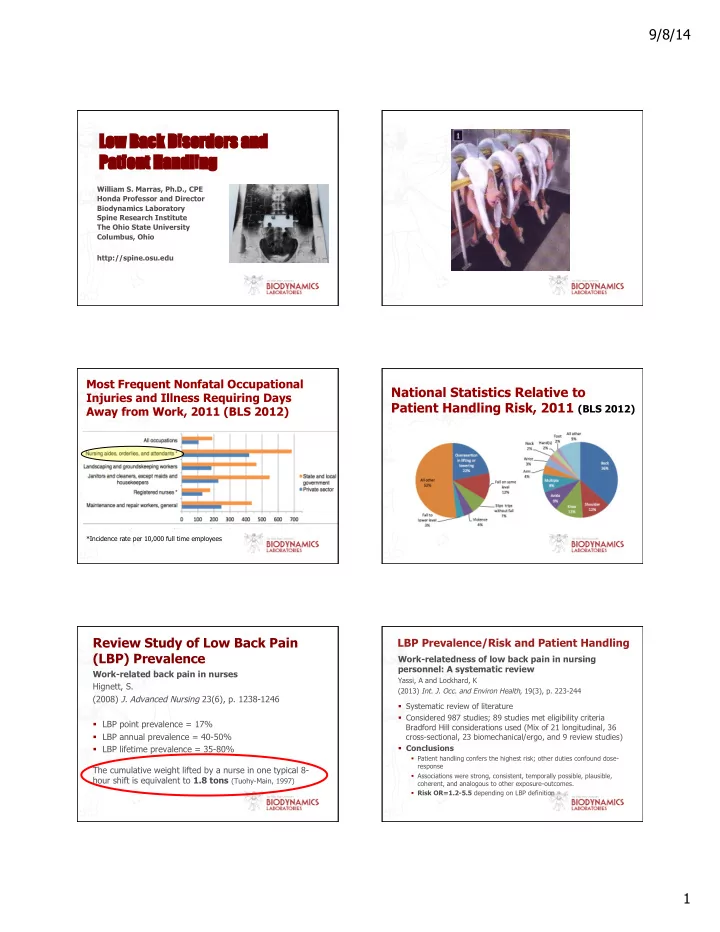
9/8/14 Low Back k Disorders and Pa Patient Handling William S. Marras, Ph.D., CPE Honda Professor and Director Biodynamics Laboratory Spine Research Institute The Ohio State University Columbus, Ohio http://spine.osu.edu Most Frequent Nonfatal Occupational National Statistics Relative to Injuries and Illness Requiring Days Patient Handling Risk, 2011 (BLS 2012) Away from Work, 2011 (BLS 2012) *Incidence rate per 10,000 full time employees Review Study of Low Back Pain LBP Prevalence/Risk and Patient Handling (LBP) Prevalence Work-relatedness of low back pain in nursing personnel: A systematic review Work-related back pain in nurses Yassi, A and Lockhard, K Hignett, S. (2013) Int. J. Occ. and Environ Health , 19(3), p. 223-244 (2008) J. Advanced Nursing 23(6), p. 1238-1246 § Systematic review of literature § Considered 987 studies; 89 studies met eligibility criteria § LBP point prevalence = 17% Bradford Hill considerations used (Mix of 21 longitudinal, 36 § LBP annual prevalence = 40-50% cross-sectional, 23 biomechanical/ergo, and 9 review studies) § Conclusions § LBP lifetime prevalence = 35-80% § Patient handling confers the highest risk; other duties confound dose- response The cumulative weight lifted by a nurse in one typical 8- § Associations were strong, consistent, temporally possible, plausible, hour shift is equivalent to 1.8 tons (Tuohy-Main, 1997) coherent, and analogous to other exposure-outcomes. § Risk OR=1.2-5.5 depending on LBP definition 1
9/8/14 Recent Studies Indicating LBP Current State of LBP Treatment Prevalence/Risk and Patient Handling Patient transfers and assistive devices: Prospective § A precise diagnosis is unknown in 80% to 90% of patients cohort study on the risk for occupational back injury among with low back pain (Deyo & Weinstein, 2001) healthcare workers § Few diagnosed through imaging (10-15%) Andersen, L., et al. (2014) Scand. J. Work, Environ. & Health, 40(1), p. 74-81 § Spend $90 Billion per year treating back problems in the U.S. (about the same as we spend on cancer) (JAMA, 2011) § Prospective cohort study of work-related LBP risk factors in § Cost of treatment increased 65% in 8 years (Martin, et al., health care workers 2008) § 5017 female eldercare workers in Denmark § Less than 50% of surgeries are successful (Weinstein, 2006) § Daily patient transfers incr. LBP risk (OR = 1.75) § Attributable fraction risk estimate = 36% § Value of prevention Low Back Pain Risk Factor Environment Social & Org. Individual Physical Factors Factors Factors Physical Factors (NRC/IOM, 2001) Biomechanical Implications Biomechanics is More than Strength Expanded OSHA 300 log as metric for bariatric patient-handling staff injuries Randall, S. B., Pories, W. J., Pearson, A., Drake, D.J. (2009) Surg Obes Relat Dis, 5(4), p. 463-468 § Patients with BMI > 35 = < 10% of patients § Handling patients with BMI > 35 associated with: § Turning and Repositioning patient implicated in: § 31% of cases § 29.8% injuries § 27.9 % lost time § 37.2% restricted time § Usually performed using biomechanics and NOT equipment 2
9/8/14 Traditional Biomechanical Logic Intervertebral Disc Load – Tolerance Relationship and Risk § The primary source of low back pain is suspected to be Risk of Injury the disc (Nachemson, 1976; Videman and Battie, 1996; An, 2004) Spinal Load § Noxious stimulation of the disc produces symptoms of Tolerance low back pain Safety Margin § Annular tears and reduced disc height are associated Loading Pattern with low back pain (Videman et. al., 2003) § Mechanical load can be the stimulus for pain (Marras, 2008) § Disc problems are very common in those reporting LBP (Cheung, et al., 2009) Time (McGill, 1997) Disc Degeneration Intervertebral Disc How Cumulative Trauma Develops in the Spine Disc Nutrition Pathways Vertebral Endplate Vertebral Body Vertebral Endplate Disc 3
9/8/14 How Cumulative Trauma How Cumulative Trauma Develops in the Spine Develops in the Spine Vertebral Endplate Vertebral Endplate Microfractures Scar Tissue Development Spine Compression Disc Degeneration and Tolerance 3400-6400 N Limit (NIOSH, 1981) Cumulative Trauma Limits Scar Tissue Vertebral Body Vertebral Endplate Anterior/Posterior (A/P) Shear Disc 750-1000 N Limit Lateral Shear (McGill, 1994; Yingling 1999) 750-1000 N Limit (Miller, 1986) Spine Loads Results from the Reaction of Internal Forces to External Forces Biome mechanical Modeling of the Low Back k External Force Internal Force Can we assess specific spine tissue loads in-vivo ? 4
9/8/14 Assessment of Spine Forces Laboratory Assessment of Push-Pull Based Upon Task Assessment of Specific Tissue Loads Spine Loads at Different Levels Patient Lifting Origins/ Destinations Our Early Patient Lifting Studies § Bed to/from wheelchair with arms § Bed to/from wheelchair with one arm removed § Portable commode chair to/ from hospital chair 5
9/8/14 Pre-Lifting during Patient Patient Transfer Techniques Handling § 1 person hug § 2 person hook and toss § 2 person gait belt Spine Compression as a Function of Spine Compression as a Function Transfer Task of Transfer Technique Compression Force (N) 9000 Compression Force (N) 9000 8000 8000 Maximum 7000 7000 Maximum Tolerance Tolerance 6000 6000 5000 5000 4000 Safe Limit 4000 3000 Safe Limit 3000 2000 Hug HOOK BELT HOOK BELT 2000 Bed – Wheelchair Commode One-Person Left Side Wheelchair Bed – Chair - Right Side - Bed w/o Arms – wheelchair Wheelchair - Chair Commode 2 person 2 person Bed w/o Arms Transfer Technique Transfer Task One-Person Two-Person Spine Compression as a Function of Repositioning Technique Patient Repositioning Techniques 12000 Compression Force (N) 11000 10000 9000 8000 Maximum 7000 Tolerance 6000 5000 4000 Safe Limit 3000 2000 Hook Hook Thigh & Sheet Hook Thigh & Sheet Shoulder Shoulder Left Side Right Side One Person Two Person Two Person Repositioning Technique 6
9/8/14 Implication from our First Study Body Mechanics? Physical therapists vs. nurses in a rehabilitation § Risk associated with one- or two- caregiver patient lifting hospital: comparing prevalence of work-related musculoskeletal complaints and working conditions § Conclusion - There is no safe way to lift a patient manually! Alperovitch-Najenson, D., Treger, I., and Kalichman, L. (2014) Archives of Environmental & Occupational Health, 69(1), 33-39 § The magnitude of spine loading is so great that any benefit of using proper body mechanics is negligible § Compared LBP rate in 26 PTs vs. 54 nurses in a Rehab. Hospital § LBP was more prevalent in PTs than nurses § Suggestion – Must employ patient lifting device § Conclusion: should initiate a “no-lift” policy Patient Handling Musculoskeletal Disorder Rate Changes (#MSDs/employee-hours worked)*200,000 Patient Handling Interventions Type of n Baseline Follow-up Rate Ratio (FU/ Intervention median median BL MSD rate) (Range) (Range) Reduce 16 9.89 6.65 .66 Bending (0.0-42.65) (0.0-59.51) Zero Lift 44 15.38 9.25 .54 (0.0-87.59) (0.0-28.27) Reduce 8 6.47 0.33 .15 Carrying (0.0-15.80) (0.0-6.70) Multiple 32 11.98 7.78 .56 Interventions (0.0-60.34) (0.0-25.94) All 100 12.32 6.64 .52 (0.0-87.59) (0.0-59.51) § Intervention Effectiveness (prospective observation of 100 units) (Fujishiro, et al. 2005) Patient Handling Change in MSD Rates per Intervention (baseline to follow-up) Our Previous Studies Type of # Units Number of Units P-value Decreased Increased Intervention or no change § Risk associated with one- or two- caregiver patient lifting Reduce 12 4 0.056 § Conclusion - There is no safe way to lift patient manually! Bending (75%) (25%) § Suggestion - Employ Patient Lifting assistance device Zero Lift 32 12 0.002 § Intervention Effectiveness (prospective (72.7%) (27.3%) observation of 100 units) Reduce 7 1 0.031 § Conclusion – Often observe significant reduction in risk Carrying (87.5%) (12.5%) § Not all interventions created equally! Multiple 26 6 0.001 § 23% of lift interventions had increased reporting Intervention s (81.3%) ( 18.7%) All 77 23 <0.001 (77.0%) (23.0%) (Fujishiro, et al. 2005) 7
9/8/14 Lifting Transformed into Pushing and Pulling Pushing and Pulling Patient Lift Devices Pushing/Maneuvering Patients Ceiling lift Floor based lift Likorall 243 ES Liko Viking L (230 Kg capacity) (250 Kg capacity) Patients Experimental Conditions § Lift system § Ceiling based § Floor based – large wheel vs. small wheel § Large wheels (5 inch diameter rear; 4 inch diameter front) § Patient weight § Small wheels (3 inch diameter rear; 2 inch diameter front) § 125 lb (56.8 Kg) § Floor Surface § 160 lb (72.7 Kg) § Hard Floor § 360 lb (163 Kg) § Carpet 8
9/8/14 Course Path and Required Control Course Path and Required Control CONFINED TURN GRADUAL TURN BATHROOM END START STRAIGHT SHARP TURN NOTE: All dimensions are in inches Floor Based Lift used on Carpet Ceiling Lift Trial and Analysis Risk Exposure Quantification: Floor Based Lift used on Carpet Patient Handling 9
Recommend
More recommend