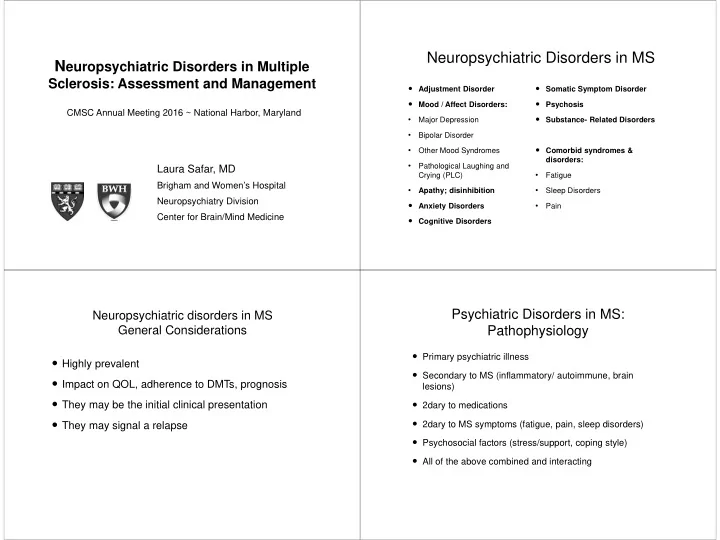
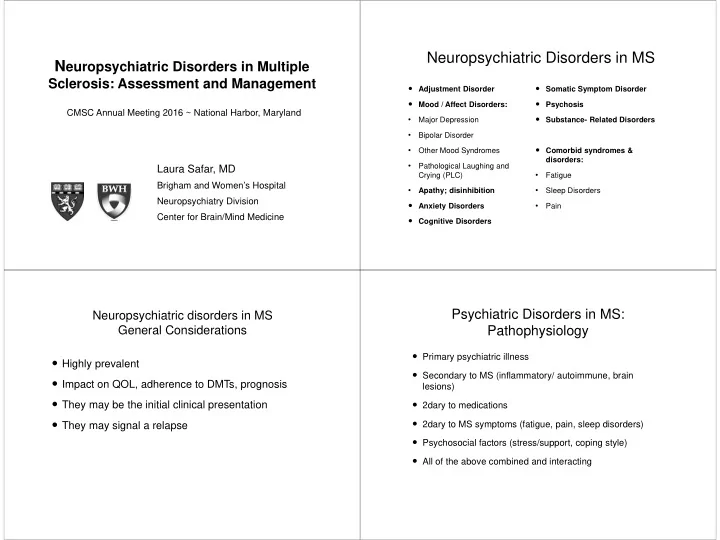
Neuropsychiatric Disorders in MS N europsychiatric Disorders in Multiple Sclerosis: Assessment and Management Adjustment Disorder Somatic Symptom Disorder Mood / Affect Disorders: Psychosis CMSC Annual Meeting 2016 ~ National Harbor, Maryland Substance- Related Disorders • Major Depression • Bipolar Disorder Comorbid syndromes & • Other Mood Syndromes disorders: • Pathological Laughing and Laura Safar, MD • Crying (PLC) Fatigue Brigham and Women’s Hospital • • Apathy; disinhibition Sleep Disorders Neuropsychiatry Division Anxiety Disorders • Pain Center for Brain/Mind Medicine Cognitive Disorders Psychiatric Disorders in MS: Neuropsychiatric disorders in MS General Considerations Pathophysiology Primary psychiatric illness Highly prevalent Secondary to MS (inflammatory/ autoimmune, brain Impact on QOL, adherence to DMTs, prognosis lesions) They may be the initial clinical presentation 2dary to medications 2dary to MS symptoms (fatigue, pain, sleep disorders) They may signal a relapse Psychosocial factors (stress/support, coping style) All of the above combined and interacting
General Approach: Analyze complexity Anxiety Screen, evaluate, & treat Screen/evaluate: Sleep Cognitive Dysfunction PHQ-9: Depression (BDI, HADS) Problems Ms. B: Depression GAD-7: Anxiety since 20s, +FH. CNS-LS: PBA Sx worsened MDQ: Bipolar Disorder since MS MFIS: Fatigue: Physical, cognitive, social MS physical onset. Isolation, sx: Pain, Audit-C: Alcohol, substances hypoactivity fatigue MoCA: Cognitive performance Baclofen, ADLs and IADLs tizanidine, Risk: Meds, suicide, falls, abuse, driving, fire, financial. BZD, steroids …and also evaluate: DMTs- possible side effects Associated MS symptoms (fatigue, pain) Brand name Psychiatric Side effects / other notes DMT Medical comorbidities (OSA, DM) Interferon beta IM, Avonex (IM), Depression 1a SC DMTs: Therapeutic & side effects Rebif (SC) SC Interferon beta Betaseron, Depression Symptomatic treatments including CAMs 1b Extavia Glatiramer SC Copaxone Anxiety Coping style, values & priorities, motivations IV Natalizumab Tysabri Depression PO Fingolimod Gilenya Neutral or ?Benefit for depression Support system, stressors, access to treatment, (Montalban- Mult Scler 2011). Monitor QTc treatment team
Symptomatic treatments in MS Treatment: Bring it all back together Bowel and Bladder Steroids (depression, agitation, euphoria, insomnia, psychosis) Oxybutynin Bio-psycho-social Neurologist / neurological team Tolterodine Pain Treatment Amitriptyline Individualized: Mental Heath team (Psychiatrist, Phenytoin nurse practitioner, Social Worker/ Darifenacin Carbamazepine Preferences & values psychotherapist, Trospium Amitriptyline or Nortriptyline Neuropsychologist) Longitudinal: Needs Gabapentin Fatigue Case manager vary: Educate, anticipate, Pregabalin Amantadine accompany, assist with OT, PT, CRT Duloxetine Stimulants planning Opioids PCP, Pain specialist, sleep Modafinil specialist, urologist, other. Support higher Dalfampridine ( Ampyra ) Spasticity Patient and caregivers functioning, positive Baclofen Psychotropics/ sleep agents coping skills Diazepam MS society, community resources, CAMs web Dantrolene Interdisciplinary Cannabinoids Tizanidine Attorney (disability/ labor, estate planning) Intrathecal Baclofen Neuropsychiatric Disorders in MS Mood Disorders in MS Study Fifty (50) patients with MS seen for treatment in Adjustment Disorder Somatic Symptom Disorder outpatient neuropsychiatry clinic. Mood / Affect Disorders: Psychosis Examined on the Patient Health Questionnaire-9 (PHQ- Substance- Related Disorders • Major Depression 9), the Generalized Anxiety Disorder 7-item scale (GAD- 7), the Center for Neurologic Study-Lability Scale (CNS- • Bipolar Disorder LS) for pseudobulbar affect (PBA), the Mood Disorder Comorbid syndromes & • Other Mood Syndromes Questionnaire (MDQ), and the Modified Fatigue Impact disorders: Scale (MIFS). • Pathological Laughing and • Crying (PLC) Fatigue Also evaluated clinically, in initial psychiatric visits lasting • Apathy; disinhibition • Sleep Disorders 75 min and follow up visits lasting 45-60min. Anxiety Disorders • Pain Findings from both, clinical evaluation and instruments were analyzed. Cognitive Disorders
Results Results MFIS and Depression: Strong correlation between MFIS PHQ-9 analysis: 66% of our patients had a PMR/SAD scores (total, and sub-scales) and Depression ratio =/> 1. MDQ and Bipolar Disorder: PMR= Fatigue, sleep, concentration, psychomotor retardation items 62% of individuals endorsed 1-3 items on the MDQ. This included “non-relevant” responses (eg, distractibility due to SAD= Decreased interest, sadness, negative self- cognitive dysfunction). thoughts, suicidal thoughts 10 patients endorsed 4 or more MDQ items. Of these, 6 were assessed as presenting bipolar spectrum symptoms. 11 subjects had PHQ-9 Score >5 but not depression. CNS-LS Questionnaire and PBA: 8 subjects had PHQ-9 >10 but mild depression. 9 individuals had scores >13 (suggestive of PBA; highly Positive correlation between PHQ-9 scores and clinical sensitive but less specific). 3 of those were considered to have mild PBA symptoms, in the context of clinical depression. depression Depression Conclusions Prevalence:30-50% (Major Depression) Mood and affect symptoms in MS may include sub- Clinical Presentation: Similar to primary depression syndromal depression, anxiety, bipolar, and PBA symptoms, as well as the full-fledged disorders. Comorbid MS symptoms: Fatigue, sleep disturbances, cognitive deficits, PMR Patients frequently present combined presentations. Comorbid psychiatric symptoms: Screening tools may help identify relevant symptoms Irritability, disinhibition, mood lability efficiently PLC (Pseudobulbar affect) Clinical correlation is needed to reach an accurate Apathy: Syndrome of decreased motivation/ interest diagnosis and select appropriate treatment. Anxiety
Depression: Treatment Bipolar Disorder Antidepressants: Small RCTs: Desipramine (marginal); Sertraline Open-label trials: Duloxetine; Moclobemide; Fluoxetine; Sertraline; Prevalence: Twice as common in MS as in the GP Imipramine; Tranylcypromine Steroids, baclofen, stimulants, may contribute ECT: Severe, TRD rTMS, tDCS: Small trials- more research needed Treatment: Mood stabilizers & atypical antipsychotics Exercise: Possible reduction in depressive symptoms Steroids- induced mania: Prophylaxis with mood stabilizers or atypical antipsychotics Psychotherapy: CBT, MBT, ACT, Positive Psychology Sub-syndromal “bipolar” symptoms: Irritability, emotional Treat associated symptoms: Fatigue, cognition, other mood symptoms lability, agitation, disinhibition: Treat MS (this may need to go to top) Treat MS symptoms, treat comorbidities Cognitive Disorder Anxiety Disorders in MS 40-70% of individuals with MS exhibit cognitive dysfunction Prevalence 15-55 % Clinical presentation: Common complaints: Difficulty multitasking; organizing; things take GAD longer to do; increased effort for same tasks; less sharp Adjustment: Post- diagnosis & Somatic complaints; relapses Abilities most commonly affected: differential with MS physical Unpredictability- MS course, symptoms Information Processing Speed disability PD Memory: Encoding & retrieval Attention OCD It increases suicide risk Executive function Treatment: Meds and Increased use of Word retrieval benzodiazepines, other psychotherapy as in sedatives, alcohol, cannabis Deficits may occur early, before physical disability; profile broadens primary anxiety disorders with MS progression; 10-25% of patients develop dementia Stress-management, ACT, Office screening: MoCA - Dagenais Can J Neurol Sci 2013 mindfulness Neuropsychological testing
Cognitive Disorders: Treatment Thank you Treat depression, anxiety, insomnia, fatigue Treat MS: DMTs may improve cognition Reduce polypharmacy Amphetamine; methylphenidate: May improve attention; processing speed; learning &memory- Benedict 2008; Morrow 2013 & 2009 Modafinil may improve attention- Lange J Neurol 2009 AChEI: Donepezil: Possible benefit. Rivastigmine: Small studies; from none to marginal benefit Memantine: No benefit; possible neurological worsening (Lovera)(Villoslada 2009) Brigham and Women’s Hospital Amantadine/pemoline: Small trial; no significantly different from placebo Neuropsychiatry Division Cognitive Rehabilitation Center for Brain/ Mind Medicine Partners MS Center
Recommend
More recommend