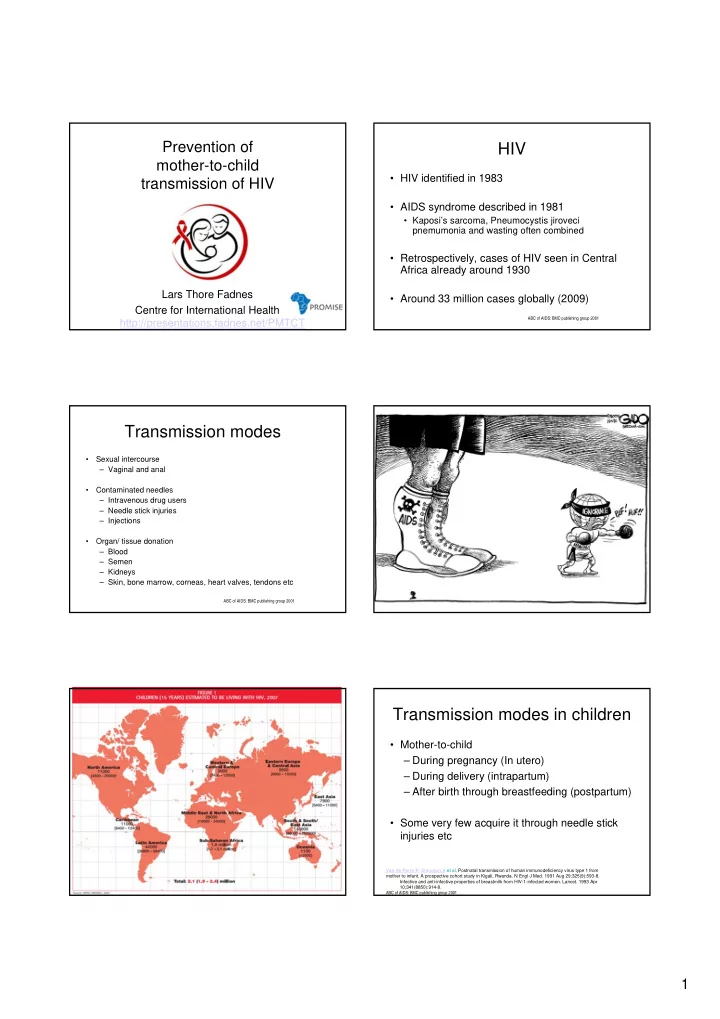
Prevention of HIV mother-to-child • HIV identified in 1983 transmission of HIV • AIDS syndrome described in 1981 • Kaposi’s sarcoma, Pneumocystis jiroveci pnemumonia and wasting often combined • Retrospectively, cases of HIV seen in Central Africa already around 1930 Lars Thore Fadnes • Around 33 million cases globally (2009) Centre for International Health ABC of AIDS: BMC publishing group 2001 http://presentations.fadnes.net/PMTCT Transmission modes • Sexual intercourse – Vaginal and anal • Contaminated needles – Intravenous drug users – Needle stick injuries – Injections • Organ/ tissue donation – Blood – Semen – Kidneys – Skin, bone marrow, corneas, heart valves, tendons etc ABC of AIDS: BMC publishing group 2001 Transmission modes in children • Mother-to-child – During pregnancy (In utero) – During delivery (intrapartum) – After birth through breastfeeding (postpartum) • Some very few acquire it through needle stick injuries etc Van de Perre P , Simonon A et al, Postnatal transmission of human immunodeficiency virus type 1 from mother to infant. A prospective cohort study in Kigali, Rwanda. N Engl J Med. 1991 Aug 29;325(9):593-8. Infective and anti-infective properties of breastmilk from HIV-1-infected women. Lancet. 1993 Apr 10;341(8850):914-8. ABC of AIDS: BMC publishing group 2001 1
Transmission risk of HIV related to Factors related with mother-to-child transmission of HIV maternal HIV stage MATERNAL FACTORS-MILK • Viral load (cell-free and cell-ssociated) • Viral strain Primary HIV Asymptomatic HIV Symptomatic • Hiv provirus increases risk Viral load • Protective factors: – Lipids – Lactoferrin – Lysozymes CD4 count – HIV antibodies – Cytotoxic cells MATERNAL HEALTH: • Maternal immunosuppression – Low CD4 0 3 months 5-10 years • Vitamin A deficiency • Breast problems increasing white blood cells and number of virus particles in the milk: Highly Less Highly – Cracked or bleeding nipples – Mastitis (clinical/ sub-clinical) infective infective infective – Breast abscesses – Trush Lehman DA, Farquhar C. Biological mechanisms of vertical human immunodeficiency virus (HIV-1) transmission. Rev Med Virol. 2007 Nov-Dec;17(6):381-403. Infectivity of milk Case: Faith INFANT FACTORS • Oral/ gastrointestinal (integrity of mucous membranes) – Stomatitis, oral thrush • HIV positive parents – Ulcerations – Pharyngitis, oesophagitis • 4 months old child with growth failure – Gastroenteritits (WLZ -3) and fungal infection • Receiving solid or semi-solid food in addition to breast milk during gastrointestinal the first months (mixed feeding) • Low-birth weight • Poor nutritional status Is it likely to be HIV? – • Protective factors How can HIV be diagnosed in children? – – Antiretroviral prophylaxis – Protective antibodies or cytotoxic CD8 cells If HIV is diagnosed, what about treatment – If HIV is diagnosed, what about – breastfeeding? Ref. Lehman DA, Farquhar C. Biological mechanisms of vertical human immunodeficiency virus (HIV-1) transmission. Rev Med Virol. 2007 Nov-Dec;17(6):381-403 Diagnosing HIV in children HIV testing • Direct demonstration of virus – PCR • How can HIV be diagnosed in children? – Viral culture • Indirect tests (antibody tests) • When can it be diagnosed? – All rapid tests – ELISA tests – Confirmatory Western Blot • More about testing: http://wwwn.cdc.gov/dls/ila/hivtraining/video.aspx 2
PCR Rapid tests Transmission rates • Without intervention: What is the total risk of HIV- transmission from mother to child? – What is the risk without any breastfeeding? – What is the risk including breastfeeding? A. Less than 10% of the children? B. 10%-20 of the children? C. 20%-40 of the children? D. 40%-60 of the children? E. Above 60 of the children? Is it better to avoid breastfeeding? Breastfeeding has benefits related to Morbidity • Less infections (diarrhoea, pneumonia, otitis media etc) • Less allergies and auto-immune diseases • Better growth Health aspects in adult life Probably slightly better cognitive outcomes Reduced risk of child deaths 3
Mortality from all causes Estimated 13% of 8 million child deaths could be prevented with optimal breastfeeding • Particularly in low-income settings • Jones G et al : How many child deaths can we prevent this year? Lancet 2003. 8% of deaths avoided with promotion of exclusive breastfeeding • Bhutta ZA et al : What works? Interventions for maternal and child undernutrition and survival . Lancet 2008. The Dilemma Case: Rachel • Mother from Mali testing HIV-positive for BALANCE: HIV just before delivery. No clinical symptoms of HIV Risk of HIV-1 • What about breastfeeding? transmission through • What about antiretroviral medicines breast milk or other treatment? • To mother? & • To child? Risk of child death • What will you say? through non- breastfeeding HIV transmission to Infant feeding patterns children • Exclusive breastfeeding and Nevirapine + zidovudine before delivery and predominant breastfeeding nevirapine to infant post- partum EBF • Relatively low risk of HIV-transmission PEP ARV treatment during RF • Positive effect on respiratory infections and pregnancy risk of several diseases • Not beneficial after around 6 months of age 10-20% 5% 10-20% 60-80% not HIV-infected Ante- If optimal management during through natal delivery BF • Complementary feeding/ partial breast- feeding/ mixed feeding • Necessary to give more than breast milk after HIV-positive 6 months of age 4
Case: Mary Case: Mary • Atenolol has low protein binding and is excreted in high • Mother testing negative for HIV proportion into breast milk with diabetes mellitus type II and • Unfortunate effect on child hypertension Metoprolol or propranolol are safer options – • Has been prescribed atenolol • Metformin is relatively safe when breastfeeding and metformin by family doctor • Child 1 month and Breastfeeding is safe when changing atenolol into e.g. metoprolol or breastfeeding and ask whether propranolol breastfeeding is safe? • What will you say? • Lactation Medicine on ToxNet (NLM): http://toxnet.nlm.nih.gov/cgi-bin/sis/search G8 Amming og legemidler http://legemiddelhandboka.no/ https://www.tryggmammamedisin.no Lessions from the large PMTCT studies • Not breastfeeding – high risk of death for the infant – Replacement feeding - increasing mortality Guidelines and • Women who need HAART for her own health should receive it – (clinical symptoms or CD4 < 350 cells/mL) recommendations on infant – Need for early diagnosis in pregnancy • For mothers with CD4 > 350 cells/ml feeding in the context of HIV – both maternal HAART and infant prophylaxis seems acceptable • Risk resistance for infants who become infected – depending on drug – Nevirapine alone is unfortunate from WHO 2010 • Often a need to continue breastfeeding beyond 6 months to reduce death and disease risk for the infant • Contextual and operational research is needed • Methodological and ethical challenges Recommendation 1 Key principles on HIV and infant feeding • Balancing HIV prevention with protection from other causes of child mortality • In women with confirmed HIV serostatus, • Ensuring mothers receive the care they need initiation of ART for her own health is • Integrating HIV interventions into maternal and child health services recommended when • Setting specific recommendations – CD4 <350 cells/mm 3 or Feasibility, affordability, acceptability, safety, sustainability – – WHO clinical stage 3 or 4 • Providing necessary balanced information – Throughout pregnancy and continue • Support mothers to appropriately feed their infants thereafter • Avoiding harm to infant feeding practices in the general population 5
Use of ARV Recommendation 2 • Preferred first-line ART regimen • Which breastfeeding practices and for how long – Many settings – AZT + 3TC + NVP/EFV. • Exclusive breastfeeding for 6 months with antiretroviral prophylaxis or maternal antiretroviral therapy – TDF + 3TC (or FTC) + NVP/EFV • Appropriate complementary feeding together with continued breastfeeding for their next months with ART prophylaxis or maternal HAART • Only stop breastfeeding when nutritionally adequate and safe diet without breast milk can be provided Recommendation 3 Recommendation 4 • When mothers decide to stop • What to feed infants when mothers stop or breastfeeding avoid breastfeeding avoid abrupt weaning – Safe and adequate replacement feeds to – enable normal growth and development • Alternatives during first 6 months: – Commercial infant feeding formula – Exressed, heat treated breast milk – Home-modified animal milk is not recommended as a replacement first six months of life Recommendation 5 Recommendation 6 • Infants born to HIV-infected women • All children born to HIV-positive mothers receiving ART for their own health should who are not in need of ART for their own receive health should have an effective ARV prophylaxis daily AZT or NVP from birth until 6 weeks – of age – started from as early as 14 weeks gestation or as soon as possible when women present late in pregnancy, in labour or at delivery. 6
Recommend
More recommend