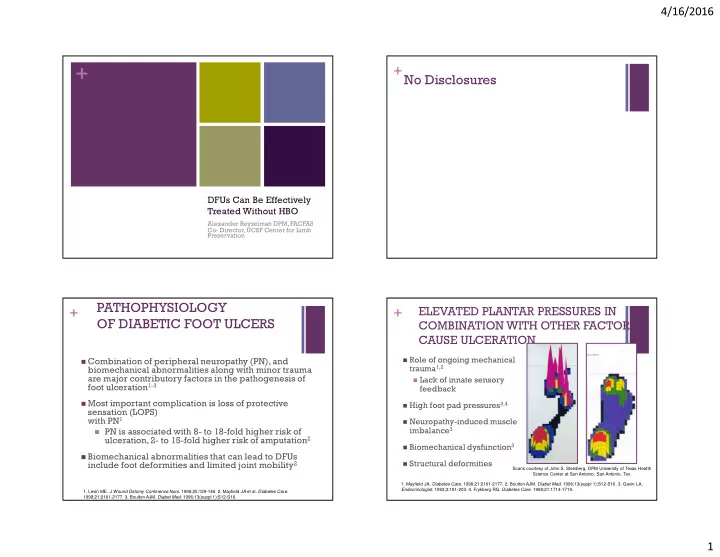
4/16/2016 + No Disclosures + DFUs Can Be Effectively Treated Without HBO Alexander Reyzelman DPM, FACFAS Co- Director, UCSF Center for Limb Preservation PATHOPHYSIOLOGY ELEVATED PLANTAR PRESSURES IN + + OF DIABETIC FOOT ULCERS COMBINATION WITH OTHER FACTORS CAUSE ULCERATION � Role of ongoing mechanical � Combination of peripheral neuropathy (PN), and trauma 1,2 biomechanical abnormalities along with minor trauma are major contributory factors in the pathogenesis of � Lack of innate sensory foot ulceration 1-3 feedback � Most important complication is loss of protective � High foot pad pressures 3,4 sensation (LOPS) with PN 1 � Neuropathy-induced muscle imbalance 3 � PN is associated with 8- to 18-fold higher risk of ulceration, 2- to 15-fold higher risk of amputation 2 � Biomechanical dysfunction 3 � Biomechanical abnormalities that can lead to DFUs include foot deformities and limited joint mobility 2 � Structural deformities Scans courtesy of John S. Steinberg, DPM University of Texas Health Science Center at San Antonio, San Antonio, Tex. 1. Mayfield JA. Diabetes Care . 1998;21:2161-2177. 2. Boulton AJM. Diabet Med. 1996;13(suppl 1):S12-S16. 3. Gavin LA. Endocrinologist. 1993;3:191-203. 4. Frykberg RG. Diabetes Care . 1998;21:1714-1719. 1. Levin ME. J Wound Ostomy Continence Nurs . 1998;25:129-146. 2. Mayfield JA et al. Diabetes Care . 1998;21:2161-2177. 3. Boulton AJM. Diabet Med . 1996;13(suppl 1):S12-S16. 1
4/16/2016 + + Reiber et al. 1999 Reiber et al . 1999 RESULTS: � The most common causal pathway to a diabetic foot ulceration The most common component causes -Neuropathy 78% NEUROPATHY + DEFORMITY + MINOR TRAUMA = -minor trauma 77% ULCERATION -foot deformity 63% -edema 37% -ischemia 35% -callus 30% Reiber et al. Diabetes Care 1999 Reiber et al. Diabetes Care 1999 Risk Factors For Non-healing Wounds + STANDARD TREATMENT FOR DIABETIC FOOT ULCERS Low mitogenic Standard treatment modalities 1 High levels of activity and MMPs and senescent Proteases � Sharp debridement of nonviable tissue cells � Treatment of infection Pro- inflammatory Offloading � Saline-moistened dressings cytokines � Off-loading to decrease pressure on extremity � Arterial revascularization if indicated Non- Vascular Infection healing intervention wound 1. Consensus Development Conference on Diabetic Foot Wound Care. ADA. Diabetes Care. 1999;22:1354-1360. 2
4/16/2016 Product Study Design % Healed Time to Heal P-Value Acellular/ Hyperbaric Oxygen therapy for Wounds Cellular + Regranex Regranex Vs. Regranex 14 Weeks P=0.007 Cellular chronic wounds (Review) SOC, 922 (50%) VS. 20 Patients SOC (36%) Weeks Kranke P, Bennett MH, Martyn-St James M, Schnabel A, Debus SE, GraftJacket GJ Vs. SOC, GJ (69.6%) 5.7 Weeks P= Acellular Weibel S. Cochrane Database of Systematic Review 2015, Issue 6. 86 Patients SOC (46.2%) VS. 6.8 Weeks Objectives Grafix Grafix Vs. Grafix (62%) 6 Weeks Vs. P=0.0001 Placenta- SOC, 97 SOC (21%) 9.8 Weeks derived Patients cellular � To assess benefits and harms of adjunctive HBOT for treating chronic ulcers of lower limb Dermagraft Dermagraft Dermagraft 1.6-1.7X P=0.023 Cellular Vs. SOC, 245 (30.0%) more likely Patients SOC (18.3%) to heal Selection Apligraf Apligraf Vs, Apligraf 9.2 Weeks P=0.0042 Cellular Criteria (56%) SOC, 208 VS. 12.8 Patients SOC (38%) Weeks � Randomized Controlled Trials (RCTs) EpiFix EpiFix Vs. EpiFix (92%) 2.5 Weeks P= <0.001 Placenta- SOC, 26 SOC (8%) VS. 5 Weeks derived � RCTs comparing benefit of wound healing using Patients acellular HBOT + Results + Final Conclusion � 12 included (577 participants) � DFU � 10 trials (531 participants) � HBOT beneficial in short term NOT � Enrolled people with DFU long term � Pooled data of 5 trials (205 participants) � Trials had various flaws in � Results design/reporting � Showed increase rate of ulcer healing, 95% confidence ratio, HBOT at 6 wks � Benefit not evident at long term 1 yr follow-up � No significant evidence in major amputation rate 3
4/16/2016 Lack of Effectiveness of Hyperbaric Oxygen + Results + Therapy for the Treatment of Diabetic Foot � N= 6,259 individuals Ulcer and the Prevention of Amputation: � Patient Criteria A Cohort Study � Adequate Lower limb perfusion � Diabetics David J. Margolis, MD, PHD, Jayanta Gupta, MD, PHD, Ole Hoffstad, M. Maryte Papdopoulos, BA, Henry A. Glick, PHD, Stephen R. Thom, MD, PHD, and Nandita � Wagner Grade 2 or greater Mitra, PHD2 Diabetes Care, Volume 36, July 2013 Treatment w/HBO Objective Endpoints � Wound Healing less likely � Amputation more likely -healed wound Compare effectiveness � 1.2-3 times less likely � 1.5-3 times more likely -LE amputation of HBO with other -assessed at 16 weeks conventional therapies after eligibility for treatment of Plantar DFUs Hyperbaric Oxygen Therapy Does Not Reduce + + Results Indications for Amputation in Patients with Diabetes with Non-healing Ulcers of the Lower Limb: A Prospective, Double-Blind, Randomized Controlled � N=157 assessed for eligibility Clinical Trial Fedorko, L., Bowen, J.M., Jones, W ., Oreopoulos, G., Goeree, R., Hopkins, R.B. and � 107 randomly assigned O’Reilly, D.J.Diabetes care (2016): dc152001. � Criteria for major amputation met ( Primary Endpoint) • Assess efficacy of HBOT in reducing � 13/54 patients in sham group amputation need Objective � 11/49 in HBOT group • Efficacy in improving wound healing of Chronic DFU Healed Wounds (Secondary Endpoint) � 12 (22%) in sham group healed • Double Blind, Placebo Controlled • Diabetics, Wagner 2-4 with >4 wks study Research � 10 (20%) in HBOT group healed duration • Received comprehensive wound care Design • 30 day sessions, 90 min of HBOT at 244 kPa 4
4/16/2016 + Conclusion: Do We Need HBOT to Heal DFUs? to Heal DFUs? � HBOT does NOT offer additional advantage to comprehensive wound care in reducing the Thank You indication for amputation or facilitating wound healing in patients with chronic DFUs � HBOT provided NO incremental benefit in measures of wound healing � Many RCTs evaluating effectiveness of other therapies (total contact cast, and substitutes) are available and have been extensively studied. + Results Continued.. + Results Continued.. � 1 trial (16 participants) � 1 trial (30 participants) � Considered venous ulcers � 30 day treatment � Reported Data at 6 wks (wound � Pts with “mixed ulcer types” reduction size) � Pts with venous ulcers and DM ulcers � Reported Data at 18 weeks (wound reduction size & number of ulcers � Significant benefit in size reduction healed) � No trials found that considered arterial or � Benefit suggested of HBOT in terms of pressure ulcers reduction of ulcer area in 6 wks 5
4/16/2016 + Wagner Classification + ROLE OF AGGRESSIVE DEBRIDEMENT � Removes necrotic tissue, senescent cells, � Stage 0- pre-ulcerative lesion foreign bodies 1,2 � Stage I- superficial with exposed sub Q � Decreases bacterial load, restores bacterial balance 1,3 � Stage II- down to tendon, ligament or bone, not infected � Stimulates the wound healing cascade to � Stage III- infected increase the healing rate 1 � Stage IV- localized gangrene of forefoot � Allows better visual assessment of ulcer area � Stage V - extensive gangrene (eg, sinus tracts or tunneling) 4,5 1. Steed DL et al. J Am Coll Surg. 1996;183:61-64. 2. Consensus Development Conference on Diabetic Foot Wound Care. ADA Diabetes Care. 1999;22:1354-1360. 3. Robson MC et al. Clin Plast Surg. 1990;17:485-492. 4. Levin ME. J Wound Ostomy Continence Nurs. 1998;25:129-146. 5. Levin ME. J ET Nurs. 1993;20:191-198. + Debridement 1) Debridement reduces the bio-burden 2) potentially prevents an infection 3) allows for better visualization and inspection of the wound. Steed and coworkers reported in their multi-center study that the patients that underwent debridement showed an improved healing response compared to the patients who did not undergo debridement. 6
Recommend
More recommend