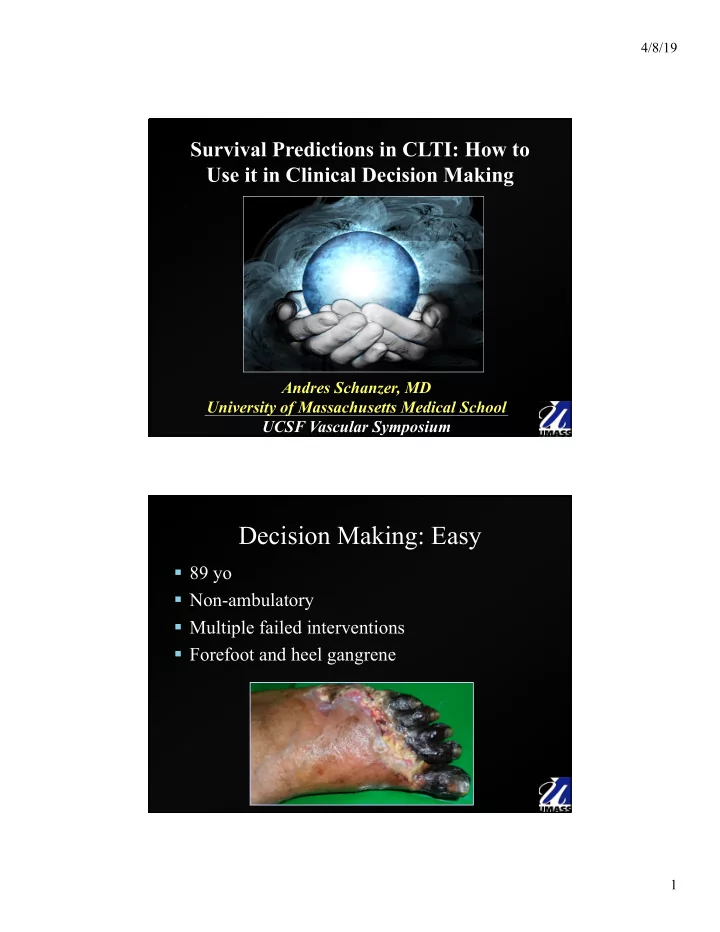
4/8/19 Survival Predictions in CLTI: How to Use it in Clinical Decision Making Andres Schanzer, MD University of Massachusetts Medical School UCSF Vascular Symposium Decision Making: Easy § 89 yo § Non-ambulatory § Multiple failed interventions § Forefoot and heel gangrene 1
4/8/19 Decision Making: Not so Easy § 77 yo § Dialysis dependent § Tissue loss § CABG 2 years prior § Lives at home independently § Contralateral GSV present Angiogram: Mild iliac/CFA disease, occluded SFA/Pop with reconstitution of anterior tibial runoff to the foot 7.5 Months Postop 2
4/8/19 Predicting Outcomes Risk Stratification Decision Making CLTI is associated with a high risk of cardiovascular events including major limb loss, myocardial infarction, stroke and death. 3
4/8/19 Open surgical bypass traditionally has been the gold standard method for revascularization. Alternative Treatment Strategies 1. Endovascular techniques 2. Primary amputation 3. Conservative management 4
4/8/19 Goal: To develop and validate a prognostic risk index for patients with CLTI considered for bypass surgery Research Design and Methods § Study Design § Retrospective review of three prospectively collected databases to derive and then validate a risk prediction model § Data Sources § PREVENT III ┼ § 1404 CLTI patients from 83 hospitals § External validation cohort * § 716 CLTI patients from 3 hospitals (BWH, USF, Sarasota Memorial) § VSGNE § § 1166 CLTI patients from 11 hospitals ┼ Schanzer et al, JVS, 2009. * Schanzer et al, JVS, 2010. § Schanzer et al, JVS, 2011. 5
4/8/19 PIII CLTI Risk Score Development 1. PREVENT III cohort randomly divided into a derivation set and a validation set 1404 patients Two-Thirds: One-Third: PIII Derivation Set PIII Validation Set 953 patients 451 patients PIII CLTI Risk Score Development 1. Derivation § Multivariable model converted to a standard integer score system 2. Validation § Internal validation (PIII validation set, n=451) § External validation (External multicenter cohort, n=716) § External validation (VSGNE, n=1166) § External validation (Finland, n=1425) 6
4/8/19 Results Multivariable Model for 1-Year AFS COVARIATES ore HR (95% CI) P-Value β coefficient ient Integer score Dialysis 2.81 (1.97, 3.99) 1.03 <0.0001 4 2.8 CLI criterion 2.22 (1.43, 3.44) 0.0004 0.80 3 2.2 Age ≥ 75 years 1.64 (1.21-2.22) 0.50 2 0.001 1 Hematocrit < 30 1.61 (1.11, 2.34) 0.48 2 0.012 1.6 History of advanced CAD 1.41 (1.05, 1.88) 0.34 1 0.021 1.4 COVARIATES nt Integer score β coeff PIII Derivation Set Stratified by Dialysis 4 2 CLI criterion 3 2 Risk Score Age ≥ 75 years 2 1 Hematocrit < 30 2 1 History of advanced CAD 1 1 Risk Score Amputation-Free Survival (%) 1 93.1 LOW 2 89.7 3 86.2 4 81.1 5 76.1 MED 6 74.5 7 71.7 8 63 9 51 10 44 HIGH 11 27.3 12 33 7
4/8/19 Discrimination PIII Derivation Set Stratified by Risk Score Amputation- Risk Categories Integer Score HR p-value Free Survival Low ≤3 85.9 1.0 (ref) __ Medium 4-7 73.0 2.11 (1.54-2.89) <.0001 High ≥8 44.6 5.50 (3.73-8.10) <.0001 PREVENT III DERIVATION SET N=953 PREVENT III DERIVATION SET N=953 90 90 AMP-FREE SURVIVAL RATES (%) AMP-FREE SURVIVAL RATES (%) 80 80 86% 86% 70 70 73% 73% 60 60 50 50 45% 45% 40 40 30 30 20 20 10 10 0 0 LOW RISK LOW RISK MEDIUM RISK MEDIUM RISK HIGH RISK HIGH RISK ≤3 Points ≤3 Points 4-7 Points 4-7 Points ≥8 Points ≥8 Points PIII RISK SCORE PIII RISK SCORE for for CRITICAL LIMB ISCHEMIA CRITICAL LIMB ISCHEMIA POINTS POINTS DIALYSIS DIALYSIS 4 4 TISSUE LOSS TISSUE LOSS 3 3 AGE ≥ 75 2 AGE ≥ 75 2 HCT ≤ 30% 2 HCT ≤ 30% 2 CAD CAD 1 1 AMP-FREE SURVIVAL RATES (%) AMP-FREE SURVIVAL RATES (%) 90 90 80 80 86% 86% 70 70 73% 73% 60 60 50 50 40 40 45% 45% 30 30 20 20 10 10 0 0 LOW RISK LOW RISK MEDIUM RISK MEDIUM RISK HIGH RISK HIGH RISK ≤3 Points ≤3 Points 4-7 Points 4-7 Points ≥8 Points ≥8 Points 8
4/8/19 Internal Validation PREVENT III DERIVATION SET N=953 PREVENT III DERIVATION SET N=953 90 90 AMP-FREE SURVIVAL RATES (%) AMP-FREE SURVIVAL RATES (%) 80 80 86% 86% 70 70 73% 73% 60 60 50 50 40 40 45% 45% 30 30 20 20 10 10 0 0 LOW RISK LOW RISK MEDIUM RISK MEDIUM RISK HIGH RISK HIGH RISK ≤3 Points ≤3 Points 4-7 Points 4-7 Points ≥8 Points ≥8 Points PREVENT III VALIDATION SET N=451 PREVENT III VALIDATION SET N=451 90 90 AMP-FREE SURVIVAL RATES (%) AMP-FREE SURVIVAL RATES (%) 80 80 88% 88% 70 70 60 60 64% 64% 50 50 40 40 45% 45% 30 30 20 20 10 10 0 0 LOW RISK LOW RISK MEDIUM RISK MEDIUM RISK HIGH RISK HIGH RISK <4 Points <4 Points 4-8 Points 4-8 Points >8 Points >8 Points External Validation 1 PREVENT III DERIVATION SET N=953 PREVENT III DERIVATION SET N=953 90 90 AMP-FREE SURVIVAL RATES (%) AMP-FREE SURVIVAL RATES (%) 80 80 86% 86% 70 70 73% 73% 60 60 50 50 40 40 45% 45% 30 30 20 20 10 10 0 0 LOW RISK LOW RISK MEDIUM RISK MEDIUM RISK HIGH RISK HIGH RISK ≤3 Points ≤3 Points 4-7 Points 4-7 Points ≥8 Points ≥8 Points BWH/USF/FSU DATASET N=716 BWH/USF/FSU DATASET N=716 90 90 AMP-FREE SURVIVAL RATES (%) AMP-FREE SURVIVAL RATES (%) 80 80 86% 86% 70 70 70% 70% 60 60 50 50 40 40 48% 48% 30 30 20 20 10 10 0 0 LOW RISK LOW RISK MEDIUM RISK MEDIUM RISK HIGH RISK HIGH RISK ≤3 Points ≤3 Points 4-7 Points 4-7 Points ≥8 Points ≥8 Points 9
4/8/19 External Validation 2 PREVENT III DERIVATION SET N=953 PREVENT III DERIVATION SET N=953 90 90 AMP-FREE SURVIVAL RATES (%) AMP-FREE SURVIVAL RATES (%) 80 80 86% 86% 70 70 73% 73% 60 60 50 50 40 40 45% 45% 30 30 20 20 10 10 0 0 LOW RISK LOW RISK MEDIUM RISK MEDIUM RISK HIGH RISK HIGH RISK ≤3 Points ≤3 Points 4-7 Points 4-7 Points ≥8 Points ≥8 Points VSGNNE DATASET N=1166 VSGNNE DATASET N=1166 90 90 AMP-FREE SURVIVAL RATES (%) AMP-FREE SURVIVAL RATES (%) 80 80 86% 86% 70 70 74% 74% 60 60 50 50 40 40 56% 56% 30 30 20 20 10 10 0 0 LOW RISK LOW RISK MEDIUM RISK MEDIUM RISK HIGH RISK HIGH RISK <4 Points <4 Points 4-8 Points 4-8 Points >8 Points >8 Points Results-Validation AFS at One Year by Risk Category 100 86.4 90 85.9 87.7 86.3 Amputation-Free Survival 73 63.7 70.1 80 74.1 70 56.1 60 47.8 44.6 45.0 50 40 30 20 10 0 Low (≤3) Medium (4-7) High (≥8) Risk category (integer score) PIII Derivation Set (n=953) PIII Validation Set (n=451) Retrospective Validation Set (n=716) VSGNNE VALIDATION SET (n=1166) 10
4/8/19 Results-Validation JVS, November, 2010 Discussion § The PIII Risk Score is easily used at initial presentation using five simple dichotomous variables: Dialysis-Dependency Tissue Loss on Presentation Hematocrit ≤ 30% Age ≥ 75 History of Advanced CAD 11
4/8/19 Conclusions § The PIII Risk Score is GENERALIZABLE Dialysis-Dependency Tissue Loss on Presentation Hematocrit ≤ 30% Age ≥ 75 History of Advanced CAD The PIII risk score is a useful clinical tool for treatment decision planning 12
4/8/19 VSGNE LEB Risk Prediction Models § Amputation or graft occlusion at 1 year * § Death at 1 year § § Ambulation status at 1 year ┼ § Clinical failure, despite graft patency, at 1 year ° * Goodney et al, Annals of Vasc Surg, 2010. ┼ Goodney et al, JVS, 2009. § Goodney et al, JVS, 2010. °Simons et al, JVS, 2010. “Patients with no risk factors had…amputation rates <1%; patients with >3 risk factors had nearly 30% chance of suffering amputation.” * Goodney et al, Annals of Vasc Surg, 2010. 13
4/8/19 “Patients with no risk factors had 1-year death rates…<5%; patients with >3 risk factors had 28% chance of dying by 1 year.” § Goodney et al, JVS, 2010. “Likelihood of nonambulatory status at 1 year was <5% in patients with no risk factors and nearly 50% in patients with >3.” § Goodney et al, JVS, 2009. 14
4/8/19 “After lower extremity bypass for CLTI, 10% of patients with a patent graft did not achieve clinical improvement at 1 year.” °Simons et al, JVS, 2010. 15
4/8/19 16
4/8/19 Risk Assessment in the CLTI Patient: Who is Likely to Benefit from Revascularization and Who is Not? § We lack validated instruments to accurately answer this question § We can predict some specific outcomes at specific time points with relatively reliable accuracy (i.e. <50% likelihood that patient is alive with an intact limb) § The best we can do is try to use available data to help inform patient and physician decision-making 17
4/8/19 18
4/8/19 Problem: 1 year or 2 year outcomes at most 19
4/8/19 “Procedure type (open/endo) was not significant in any models…” “greatest magnitude of effect associated with age >80 years, oxygen- dependent chronic obstructive pulmonary disease, stage 5 chronic kidney disease, and bedbound status.” 20
4/8/19 21
4/8/19 Thank You. 22
Recommend
More recommend