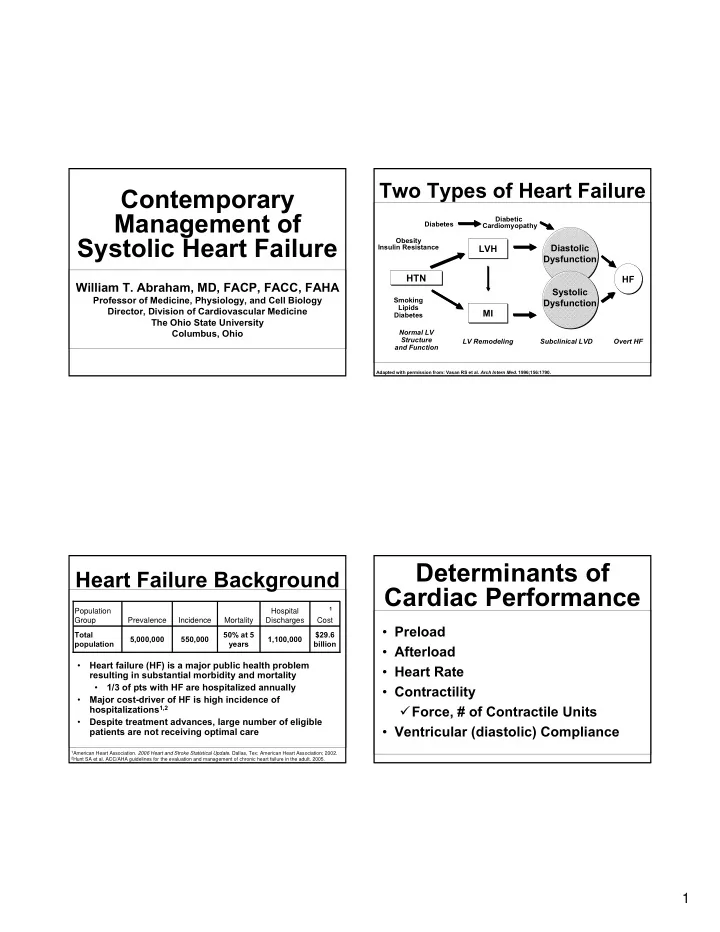
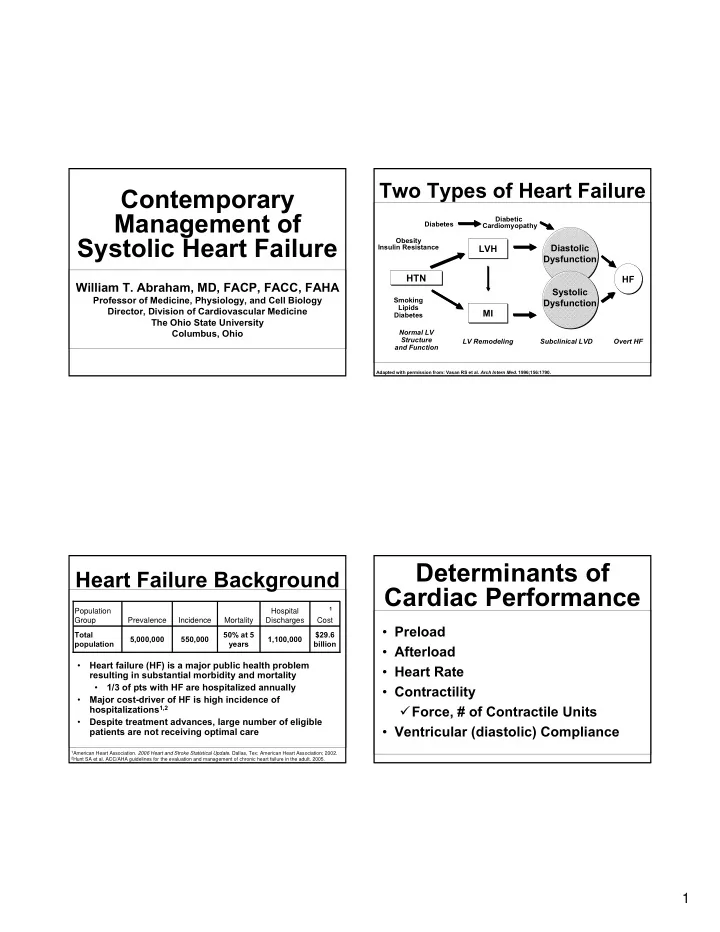
Two Types of Heart Failure Contemporary Management of Diabetic Diabetes Cardiomyopathy Systolic Heart Failure Obesity Insulin Resistance Diastolic LVH Dysfunction HTN HF William T. Abraham, MD, FACP, FACC, FAHA Systolic Professor of Medicine, Physiology, and Cell Biology Smoking Dysfunction Lipids Director, Division of Cardiovascular Medicine MI Diabetes The Ohio State University Columbus, Ohio Normal LV Structure LV Remodeling Subclinical LVD Overt HF and Function Adapted with permission from: Vasan RS et al. Arch Intern Med. 1996;156:1790. Determinants of Heart Failure Background Cardiac Performance 1 Population Hospital Group Prevalence Incidence Mortality Discharges Cost • Preload Total 50% at 5 $29.6 5,000,000 550,000 1,100,000 population years billion • Afterload Heart failure (HF) is a major public health problem • • Heart Rate resulting in substantial morbidity and mortality 1/3 of pts with HF are hospitalized annually • • Contractility Major cost-driver of HF is high incidence of • hospitalizations 1,2 � Force, # of Contractile Units Despite treatment advances, large number of eligible • • Ventricular (diastolic) Compliance patients are not receiving optimal care 1 American Heart Association. 2006 Heart and Stroke Statistical Update. Dallas, Tex: American Heart Association; 2002. 2 Hunt SA et al. ACC/AHA guidelines for the evaluation and management of chronic heart failure in the adult. 2005. 1
Preload Afterload • Based on Starling's observation that the mechanical energy released • The stress or tension distributed in the ventricular wall during ventricular ejection. between the resting and contracted state is a function of the resting muscle fiber length in isolated heart tissue. • Afterload is not constant during ejection but continually declines as ventricular volume and mid • In the whole heart, preload is synonymous with end-diastolic volume. wall radius decrease. • Practically, preload is estimated by the end-diastolic pressure • Inversely related to the velocity and extent of mid (the pulmonary capillary wedge pressure). wall shortening. • Increases in preload, or end-diastolic pressure, are associated with • The sum of forces contributing to ventricular increases in both the extent and velocity of muscle fiber shortening, afterload are referred to as inpedance, which which combine to produce an increase in stroke volume. includes the resistance of small arteries and arterioles, the compliance of the large arteries, the • Failing hearts are less responsive to changes in preload. viscosity of blood, and the forces of inertia. Starling Curves for Failing and Effects of Ventricular Afterload on Failing and Nonfailing Hearts Nonfailing Hearts Nonfailing Nonfailing Stroke Ventricular Volume Performance Failing Failing Aortic Impedance Ventricular End-Diastolic Volume 2
Pathophysiology of Heart Failure AHA/ACC Applying Classification of Recommendations and Level of Evidence Risk Factors Class I Class IIa Class IIb Class III Myocardial injury to the heart (MI, HTN, CMP, Valvular disease) Benefit >>> Risk Benefit >> Risk Benefit ≥ Risk Risk ≥ Benefit Additional studies Additional studies No additional studies Initial fall in LV performance, ↑ wall stress with focused with broad objectives needed objectives needed needed; Additional registry data would be helpful Activation of RAS and SNS IT IS REASONABLE Procedure or Procedure or Procedure or treatment SHOULD to perform procedure treatment treatment should NOT Fibrosis, apoptosis, Remodeling and Hemodynamic alterations MAY BE be performed or or administer be performed or hypertrophy, progressive Salt & water retention CONSIDERED administered SINCE administered treatment cellular/ IT IS NOT HELPFUL worsening of LV function molecular AND MAY BE alterations, HARMFUL myotoxicity Heart failure symptoms Morbidity and mortality A: Multiple randomized controlled trials Dyspnea Arrhythmias Level of Evidence B: Single trial, non-randomized studies Edema Pump failure C: Expert opinion Fatigue RAS, renin-angiotensin system; SNS, sympathetic nervous system. Hunt SA et al. J Am Coll Cardiol. 2005 ACC/AHA 2005 Guideline Update for the Diagnosis and Management of Chronic HF ACE Inhibitors Hunt SA, et al. ACC/AHA 2005 Practice Guidelines. Available at http://www.acc.org. 3
Effect of ACE Inhibitors on Mortality ACE Inhibition in Heart Failure Reduction in Patients With Heart Failure • Indicated for all patients with asymptomatic LV Mortality dysfunction and for Class I to IV Heart Failure. (Contraindications: hyperkalemia, angioedema, Trial ACEI Controls RR (95% CI) pregnancy) Chronic CHF CONSENSUS I 39% 54% 0.56 (0.34–0.91) • Start at low dose and titrate to target doses (example enalapril 10 mg bid, lisinopril 20 qd, SOLVD (Treatment) 35% 40% 0.82 (0.70–0.97) ramipril 10 mg qd, benazepril 40 qd) SOLVD (Prevention) 15% 16% 0.92 (0.79–1.08) Post-MI • Renal insufficiency is not a contraindication but SAVE 20% 25% 0.81 (0.68–0.97) must start at very low dose and very closely monitor AIRE 17% 23% 0.73 (0.60–0.89) TRACE 35% 42% 0.78 (0.67–0.91) • Monitor serum potassium and renal function. Average 23% 27% Advise checking chemistry panel 1-2 weeks after first dose. Data shown from individual trials—not direct comparison data. Garg R et al. JAMA. 1995;273:1450–1456. Pfeffer MA et al. N Engl J Med . 1992;327:669–677. The AIRE Study Investigators. Lancet . 1993;342:821–828. Køber Hunt SA, et al. ACC/AHA 2005 Practice Guidelines L et al. N Engl J Med . 1995;333:1670–1676. The SOLVD Investigators. N Engl J Med . 1992;327:685–691. ACE Inhibitor Recommendations • Recommended for all pts with current or prior I I I I I I I I I IIa IIa IIb IIa IIa IIa IIa IIa IIb IIa IIb IIa IIa IIa IIa IIb IIb IIb III IIb III IIb III IIb III IIb IIb IIb III III III III III III III III symptoms of HF and reduced LVEF, unless contraindicated • Indicated in all pts with a recent or remote history of MI regardless of LVEF or presence of HF Beta-Blockers • Should be used in pts with a reduced LVEF and no symptoms of HF, even if they have not experienced an MI I I I IIa IIb IIa IIb IIa IIb IIa IIb IIa IIa IIa IIa IIb III IIb IIb IIb III IIb IIb III IIb IIb III III III III III III III III III I I I I I I IIa IIa IIa IIa • Can be useful to prevent HF in pts at risk for developing HF with a history of atherosclerotic vascular disease, DM, or HTN with associated risk factors I I I I I I I I I IIa IIb IIa IIb IIa IIb IIa IIb IIa IIa IIa IIa IIa IIa IIa IIa IIb IIb III IIb IIb III IIb III IIb IIb IIb III III III III III III III III III • Can be beneficial in patients with HTN and LVH and no symptoms of HF MI=myocardial infarction; LVEF=ejection fraction; DM=diabetes mellitus; HTN=hypertension; LVH=left ventricular hypertrophy. Underlining represents changes from 2001 guidelines. Hunt SA, et al. ACC/AHA 2005 Practice Guidelines . Available at http://www.acc.org. 4
Recommend
More recommend