OVERVIEW C ERVICAL R ADICULOPATHY : P ATHOPHYSIOLOGY , P RESENTATION , AND C LINICAL E VALUATION Khalid M. Abbed, M.D. CERVICAL RADICULOPATHY IS a common condition that usually results from compres- sion and inflammation of the cervical nerve root or roots in the region of the neural Department of Neurosurgery, Massachusetts General Hospital, foramen. It is frequently caused by cervical disc herniation and cervical spondylosis. The Harvard Medical School, diagnosis can be established by history and physical examination, but care should be Boston, Massachusetts taken, as diagnoses can mimic or coexist with cervical radiculopathy, such as entrap- ment neuropathies. The pathophysiology, presentation, and clinical evaluation of cer- Jean-Valéry C.E. Coumans, M.D. vical radiculopathy are discussed. Department of Neurosurgery, Massachusetts General Hospital, KEY WORDS: Cervical spine, Cervical spondylosis, Nerve root, Radiculopathy Harvard Medical School, Boston, Massachusetts Neurosurgery 60[Suppl 1]:S-28–S-34, 2007 DOI: 10.1227/01.NEU.0000249223.51871.C2 Reprint requests: Jean-Valéry C.E. Coumans, M.D., Department of Neurosurgery, C ervical spondylosis is a term used to or extraspinal tumors, trauma with nerve root Massachusetts General Hospital, describe the degenerative aging process avulsion, synovial cysts, meningeal cysts, dural 15 Parkman Street, WACC 021, that encompasses a sequence of changes arteriovenous fistulae (19), or tortuous vertebral Boston, MA 02114. Email: jcoumans@partners.org in the intervertebral discs, vertebral bodies, arteries (16). Cervical radiculopathy may also facet joints, and ligaments of the cervical spine. occur without an identifiable cause. Other condi- It is a common condition that occurs as a natu- tions that can mimic cervical radiculopathy, ral consequence of aging in the majority of the which should be included in the differential adult population. As a result, it is often difficult diagnosis, are upper extremity nerve entrap- to distinguish normal physiological degen- ment, primary shoulder disease, brachial plexus eration from pathological changes. Anatomic disorders, and peripheral neuropathies. This changes should only be considered pathologi- article focuses on radiating pain secondary to cal if they are etiologically related to specific compression of cervical nerve roots by herniated clinical syndromes. disc material or pain that is associated with cer- There are three main categories of cervical vical spondylosis. spondylosis: cervicalgia (non-radiating neck pain), cervical radiculopathy, and cervical PATHOPHYSIOLOGY myelopathy. This article concerns the patho- physiology, presentation, and clinical evalua- The cervical intervertebral disc is taller ven- tion of cervical radiculopathy and the spectrum trally than dorsally, and it is the cervical disc, of radicular syndromes attributable to cervical not the vertebral body, that is responsible for spine degenerative disease. Cervicalgia and the maintenance of cervical lordosis. The outer myelopathy, which are commonly associated portion of the disc is made up of the anulus with radiculopathy and the treatment of cervi- fibrosus. The latter is crescent-shaped, and, cal radiculopathy, are covered elsewhere in this when viewed in the axial plane, it is thicker issue. ventrally than dorsally. Ventrally, it is multil- Cervical radiculopathy is a pathological aminated with interweaving fibers of alternat- process involving the cervical nerve root. It is ing orientation, but dorsally, it is only present the result of compression and inflammation of as a thin layer of collagen fibers (23). Before the nerve root or roots at or near the cervical the age of 20 years, few morphological changes neural foramen ( Fig. 1–3 ). It occurs annually in occur in the cervical spine. Beginning in the 85 out of 100,000 people (22). The most com- third decade of life, a progressive decline in mon causes for radiculopathy are cervical disc the water content of the intervertebral disc herniation ( Fig. 2 and 3 ) (17), followed by cervi- occurs and continues with age. The nucleus cal spondylosis ( Fig. 1 ) (1, 35). Cervical radicu- pulposus becomes an indistinct fibrocartilage- lopathy is less commonly caused by intraspinal nous mass (29). In patients younger than 30 S1-28 | VOLUME 60 | NUMBER 1 | JANUARY 2007 SUPPLEMENT www.neurosurgery-online.com
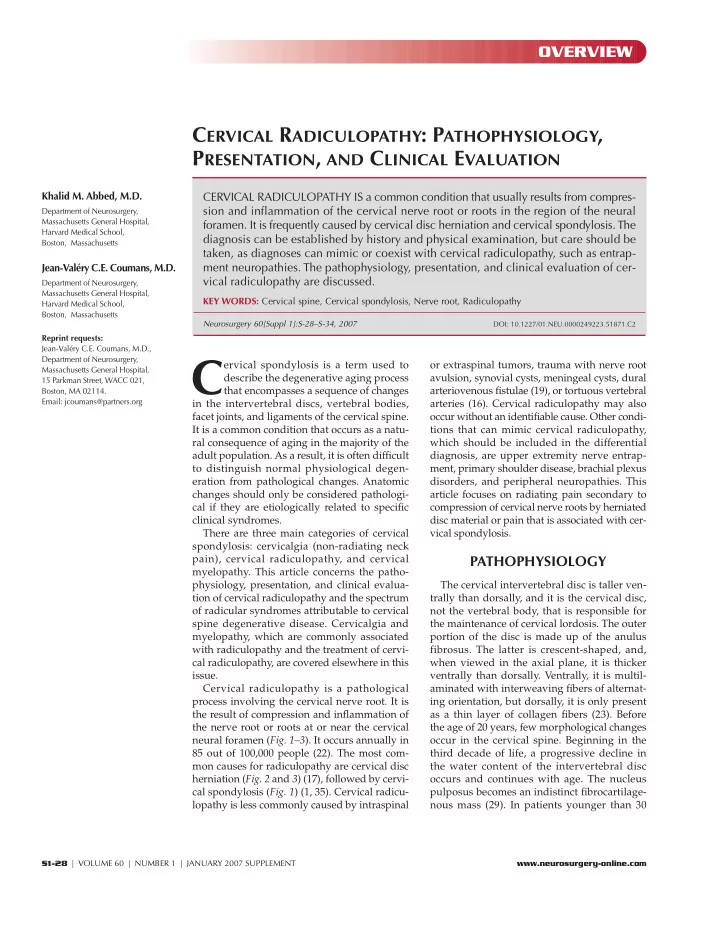
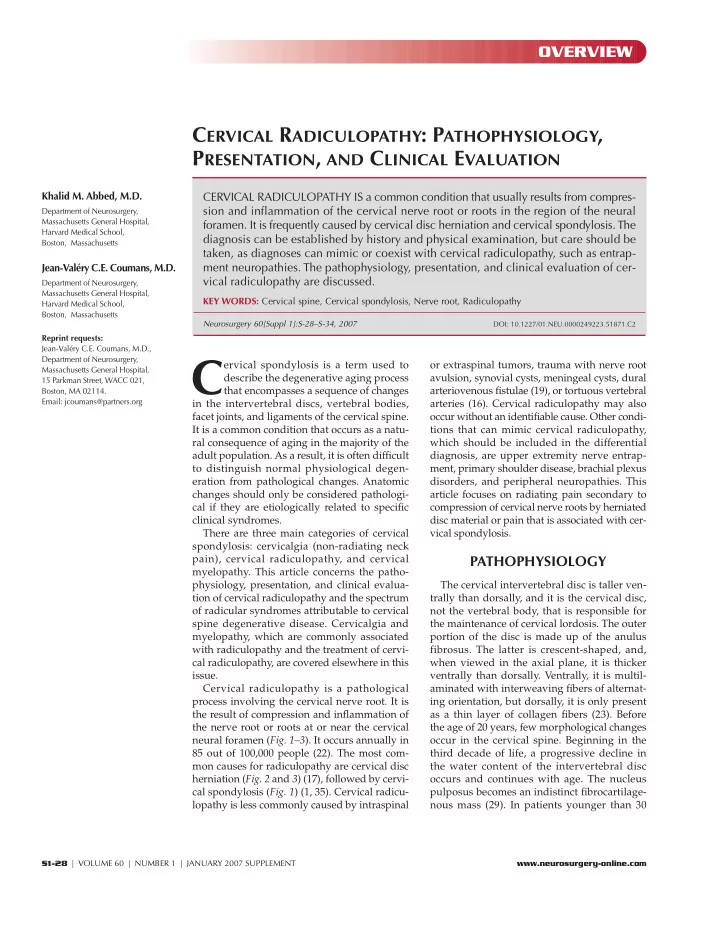
C ERVICAL R ADICULOPATHY ing the lumbar disc. In the cer- A B vical spine, true disc prolapse and herniation of the nucleus pulposus is uncommon (23). The neural foramen is bor- dered ventrally by the unco- vertebral joint and dorsally by the superior articular process of the caudal vertebra FIGURE 3. Axial T2 MRI demon- (2). Compressive radiculo- strating C7–T1 disc herniation in a FIGURE 1. Axial T2 MRI image ( A ) and CT scan ( B ) in a patient with a left pathies occur as a result of patient with a left-sided C8 radicu- C6 radiculopathy. There is a left-sided C5 to C6 osteophyte causing neural mechanical distortion of the lopathy. The patient was referred after foraminal stenosis and C6 nerve root compression. nerve root by either the unsuccessful attempted dorsal resec- hypertrophied facet joint or tion of the disc. uncovertebral joints ( Fig. 1 ), A B disc protrusion ( Fig. 2 and 3 ), spondylotic spurring of the verte- bral body, or a combination of these factors. Pressure on the nerve root may lead to sensory deficits, motor weakness, or radicular pain. Pain is related to mechanical compression and to an inflammatory response. PRESENTATION Radiculopathy can be divided into acute, subacute, and chronic. Acute cervical radiculopathy occurs in relatively young patients in the setting of a tear in the annulus fibrosus FIGURE 2. A, parasagittal reformat and subsequent prolapse of the nucleus pulposus. Subacute of CT myelogram and axial CT mye- radiculopathy occurs in patients with pre-existing cervical logram ( B ) demonstrating a left- spondylosis, without persistent symptoms except for occa- sided C6–C7 disc herniation in a patient who was unable to have an sional neck pain. Patients develop insidious symptoms, which MRI scan due to prior aneurysm clip are often polyradicular in nature. Chronic radiculopathies placement. materialize from acute or subacute radiculopathies that have failed to respond to treatment. Pain is most prominent in acute cervical radiculopathy and years, the water content of the intervertebral disc approaches diminishes as the condition becomes more chronic. It may be 90%, and it decreases to less than 70% by the eighth decade of life. described as sharp, achy, or burning and may be located in the The basic structural unit of the nucleus pulposus is glycosamino- neck, shoulder, arm, or chest, depending on the nerve root glycan protein, which consists of a proteoglycan protein core and involved. Classically, an acute radiculopathy presents with pain bulky, sterically active polysaccharide attachments of chondroitin radiating in a myotomal distribution. For example, patients with sulfate and keratin sulfate. Because of their high molecular a C7 radiculopathy often experience pain in the triceps region weight and overall negative charge, glycosaminoglycan proteins rather than the distal dermatomal region. Sensory symptoms, have a strong attraction for water molecules. With aging, these predominantly parasthesias and numbness, are more common large, sterically active glycosaminoglycan proteins gradually than motor loss and diminished reflexes. The clinician should diminish in size and number. As a result, the intervertebral disc’s keep in mind that the sensory symptoms frequently do not match ability to retain water also diminishes. These age-related changes the dermatomes illustrated in medical textbooks. Henderson et al. in the chemical composition of the nucleus pulposus and annu- (13) reviewed the clinical presentations of cervical radiculopathy lus fibrosus cause the degenerated disc to become more com- in more than 800 patients and found arm pain in 99.4%, sensory pressible and less elastic (3). Consequently, the disc loses height deficits in 85.2%, neck pain in 79.7%, reflex deficits in 71.2%, and bulges dorsally into the spinal canal. As the vertebral bodies motor deficits in 68%, scapular pain in 52.5%, anterior chest pain drift toward one another (i.e., subsidence), the ligamentum in 17.8%, headaches in 9.7%, anterior chest and arm pain in 5.9%, flavum and facet joint capsule fold in dorsally, causing a further and left-sided chest and arm pain in 1.3%. decrease in the canal and foraminal dimensions. This approxima- Radicular pain is often accentuated by maneuvers that stretch tion of adjacent vertebral bodies leads to a reactive process that the involved nerve root, such as coughing, sneezing, Valsalva, produces osteophytes around the disc margins and at the and certain cervical movements and positions. Several clinical uncovertebral and facet joints. However, the degenerative signs suggestive of radiculopathy have been described. changes of the cervical intervertebral disc differ from those affect- Davidson et al. (9) described the “shoulder abduction sign” in N EUROSURGERY VOLUME 60 | NUMBER 1 | JANUARY 2007 SUPPLEMENT 1 | S1-29
Recommend
More recommend