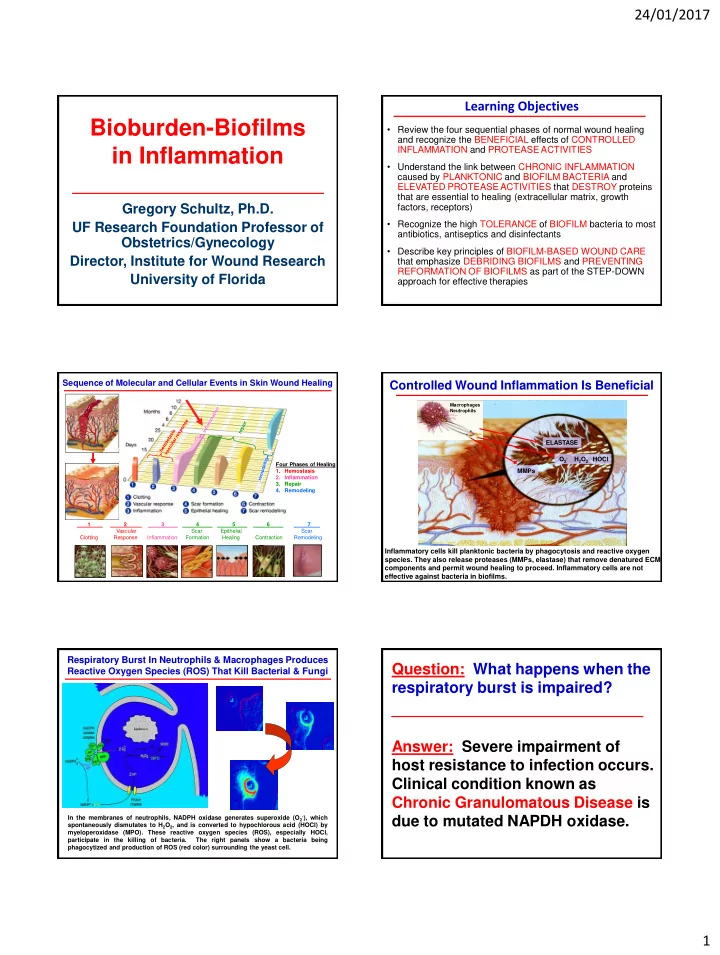
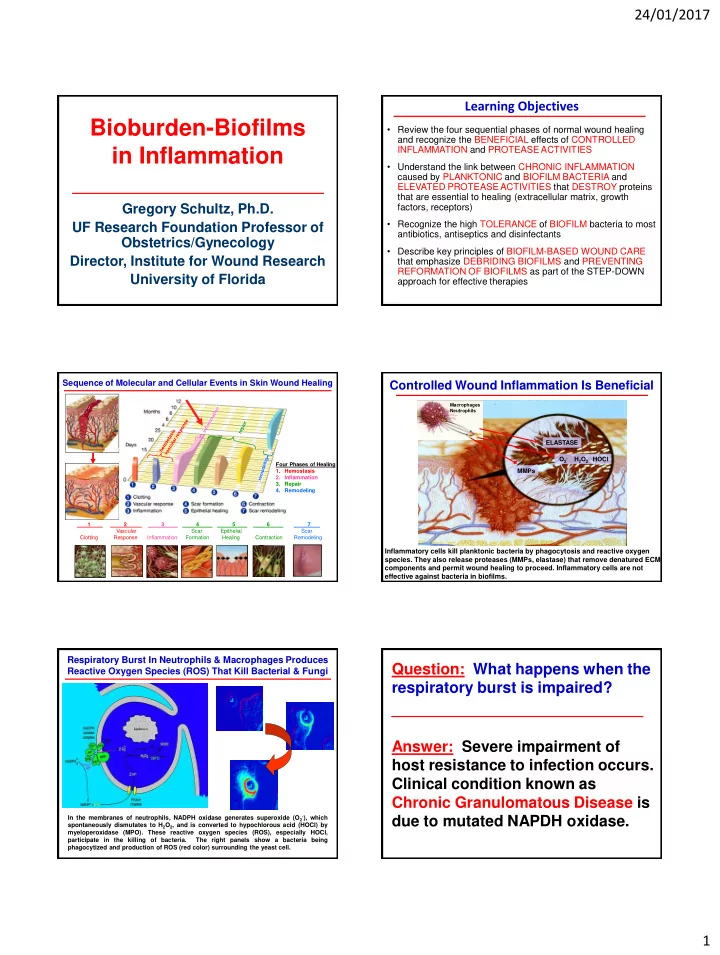
24/01/2017 Learning Objectives Bioburden-Biofilms • Review the four sequential phases of normal wound healing and recognize the BENEFICIAL effects of CONTROLLED in Inflammation INFLAMMATION and PROTEASE ACTIVITIES • Understand the link between CHRONIC INFLAMMATION caused by PLANKTONIC and BIOFILM BACTERIA and ELEVATED PROTEASE ACTIVITIES that DESTROY proteins that are essential to healing (extracellular matrix, growth Gregory Schultz, Ph.D. factors, receptors) • Recognize the high TOLERANCE of BIOFILM bacteria to most UF Research Foundation Professor of antibiotics, antiseptics and disinfectants Obstetrics/Gynecology • Describe key principles of BIOFILM-BASED WOUND CARE Director, Institute for Wound Research that emphasize DEBRIDING BIOFILMS and PREVENTING REFORMATION OF BIOFILMS as part of the STEP-DOWN University of Florida approach for effective therapies Sequence of Molecular and Cellular Events in Skin Wound Healing Controlled Wound Inflammation Is Beneficial Macrophages Neutrophils ELASTASE O 2- H 2 O 2 HOCl Four Phases of Healing 1. Hemostasis MMPs 2. Inflammation 3. Repair 4. Remodeling 1 2 3 4 5 6 7 . Vascular Scar Epithelial Scar Clotting Response Inflammation Formation Healing Contraction Remodeling Inflammatory cells kill planktonic bacteria by phagocytosis and reactive oxygen species. They also release proteases (MMPs, elastase) that remove denatured ECM components and permit wound healing to proceed. Inflammatory cells are not effective against bacteria in biofilms. Respiratory Burst In Neutrophils & Macrophages Produces Question: What happens when the Reactive Oxygen Species (ROS) That Kill Bacterial & Fungi respiratory burst is impaired? Answer: Severe impairment of host resistance to infection occurs. Clinical condition known as Chronic Granulomatous Disease is In the membranes of neutrophils, NADPH oxidase generates superoxide (O 2- ), which due to mutated NAPDH oxidase. spontaneously dismutates to H 2 O 2 , and is converted to hypochlorous acid (HOCl) by myeloperoxidase (MPO). These reactive oxygen species (ROS), especially HOCl, participate in the killing of bacteria. The right panels show a bacteria being phagocytized and production of ROS (red color) surrounding the yeast cell. 1
24/01/2017 Controlled MMPs Are Necessary for Wound Healing Chronic Granulomatous Disease Debridement, Angiogenesis, Contraction, Epithelial Migration, Remodeling • Characterized by predisposition to bacterial and fungal infections • Associated with decreased oxygen consumption P P and defective microbial killing • Due to defective mutation in components of P P P P P P P NADPH oxidase complex P 1 2 3 • Reduced levels of superoxide anion (O 2- ) which MMPs ARE NECESSARY FOR is converted to bactericidal reactive oxidants SEVERAL KEY PROCESS IN results in decreased levels of: WOUND HEALING – hydroxyl radical (OH - ) 1. removing denatured matrix P P 2. degrading capillary basement – hydrogen peroxide (H 2 O 2 ) P membrane for angiogenesis P 3. contraction of ECM by P – peroxynitrite anion (ONOO - ) 4 myofibroblasts 5 P 4. migration of epidermal cells – oxyhalides (HOCl, hypochlorus acid) 5. remodeling of scar Major Cytokines Involved in Wound Healing MMPs in Normal Wound Healing CYTOKINE CELL SOURCE BIOLOGICAL ACTIVITY PRO-INFLAMMATORY CYTOKINES ↑ PMN margination and cytotoxicity Tumor Necrosis Factor macrophages MMPs are essential for normal alpha TNF- a ↑ MMP synthesis wound healing, BUT must be: ↑ fibroblast and keratinocyte Interleukin-1 macrophages, keratinocytes chemotaxis, IL-1 ↑ MMP synthesis ↑ fibroblast proliferation – At the right places Interleukin-6 macrophages, keratinocytes, PMNs IL-6 ↑ macrophage and PMN chemotaxis Interleukin-8 macrophages, fibroblasts ↓ collagen synthesis IL-8 – At the right times Interferon- g ↑ macrophage and PMN activation macrophages, T-lymphocytes INF- g ↓ collagen synthesis ↑ MMP synthesis – At the right amounts ANTI-INFLAMMATORY CYTOKINES ↓ TNF - a , IL-1, IL-6 synthesis Interleukin-4 T-lymphocytes, basophils, mast cells ↑ fibroblast proliferation, collagen IL-4 synthesis ↓ TNF - a , IL-1, IL-6 synthesis Interleukin-10 T-lymphocytes, macrophages, ↓ macrophage and PMN activation IL-10 keratinocytes Is There a Common Molecular Hypothesis Of Chronic Wound Pathophysiology Pathology Of Chronic Wounds?? Repeated Tissue Injury, Ischemia and Bioburden – Planktonic & Biofilms TNF- a IL-1 , IL-6 Prolonged, elevated inflammation ↑ neutrophils ↑ macrophages ↑ mast cells Arterial ulcer Diabetic foot ulcer Imbalanced Proteases & Inhibitors Proteases (MMPs, elastase, plasmin), inhibitors (TIMPs, a 1PI), ROS Destruction of Essential Proteins (off-target) growth factors / receptors, ECM degradation cell proliferation, cell migration, Acute Wound Chronic Non-Healing Wound Pressure ulcer Venous ulcer B.A. Mast and G.S. Schultz. Wound Rep Reg 4:411-420, 1996. 2
24/01/2017 Chronic Infection by Medical Biofilms Wound biofilms are linked to contact lens chronic cochlear chronic CNS shunt associated otitis implant burn sinusitis infection keratitis media infection infection delayed healing catheter Mouse model breast infection showed presence of implant infection S. aureus and S. prosthetic valve epidermidis biofilms endocarditis significantly delayed ventilator associated pacemaker re-epithelialisation. 1 pneumonia infection Negative impact of pulmonary biliary stent infection in biofilm on healing infection CF patient verified by other peritoneal studies 2,3 intravascular dialysis stent infection catheter Effect of Staphylococcus aureus and Staphylococcus infection epidermidis biofilms on wound re-epithelialization.1 urinary stent prosthetic peritoneal dialysis 1. Schierle, C. F., et al. . Wound Repair Regen. 17, 354 – 9 (2009). infection joint infection catheter infection 2. Zhao, G. et al. Wound Repair Regen. 20, 342 – 352 (2012). del Pozo and Patel. The Challenge of Treating Biofilm-Associated Bacterial Infections. C lin Pharm 18 Clinical Pathologies 3. Roche, E. D. et al. . Wound Repair Regen. 20, 537 – 43 (2012). Ther 82:204-20, 2007 Heterogeneous Distribution Of Bacteria Biofilms Identified in >80% of Biopsies of Chronic In Chronic wounds Wounds but in Only 6% of Acute Wounds qPCR Pseudomonas aeruginosa A B C 9 12 Position Wound 1 Wound 2 C 510 ± 18% 920 ± 9% C 300 ± 13% 3 No sample 6 D 3 E 760 ± 7% 8200 ± 8% 6 47 ± 9% 800 ± 10% 9 280 ± 3% 15 ± 5% 12 Picture from homepage of Montana State University with permission Panels A, B & C: G. James, E. Swogger, R. Wolcott, E. Pulcini, P. Secor, J. Sestrich, J. Costerton, P. Stewart. Wound Rep Regen, 16:37-44, 2008 Panel D: HC Flemming, J Wingender The Biofilm Matrix, Nature Rev Microbiol, 8:623-633, 2010 Panel E: SR Schooling , A Hubley, TJ Beveridge. J Bacteriol 191:4097-4012, 2009 Thomsen TR, Aasholm MS, Bjarnsholt T, Givskov M, Kirketerp-Møller K, and Nielsen PH. The bacteriology of chronic M. Malone, T. Barjnsholt, A. McBain, G. James, P. Stoodley, D. Leaper, M. Tachi, G. Schultz, T. Swanson, R. Wolcott. Prevalence of biofilms in venous leg ulcer examined by culture-independent molecular methods. Wound Repair Regen, 18(1):38-49, 2010 chronic wounds: a systematic review and meta-analysis of published data, J wound Care, in press Mono-species Biofilms Verses Distribution of Species Multi-species Infections S. aureus A biofilm S. aureus biofilm P. aeruginosa biofilm 25 mm B Confocal Laser Scanning Microscopic (CLSM) images of 48-h in situ dental biofilms stained simultaneously with all- bacterium-specific EUB338 probe (red), a Streptococcus-specific STR405 probe (yellow-green), and Actinomyces- specific ACT476 probe (blue) and red represent streptococci. (A) Maximum projection image of relative thin 48-h biofilm showing complete surface coverage with the dominance of streptococci. Well-defined microcolonies of large coccoid non-streptococci are observed as well as microcolonies of A. naeslundii. Scale bar = 25 mm. (B) Sagittal (x-z, y-z) section of a multilayered dental biofilm. Note that A. naeslundii (blue) is predominantly located in the inner part of the P. aeruginosa biofilms next to the surface (bottom of the images). Some microcolonies of A. naeslundii extended almost throughout the biofilm entire thickness of the biofilm. Burmølle, M. et al. Biofilms in chronic infections – a matter of opportunity – monospecies biofilms in multispecies Fazli and Bjarnsholt et al: J Clin Microbiol. 2009 Dec;47(12):4084-9 Images from Prof Bjarnsholt with permission infections. FEMS Immunol. Med. Microbiol. 59, 324 – 336 (2010). 3
Recommend
More recommend