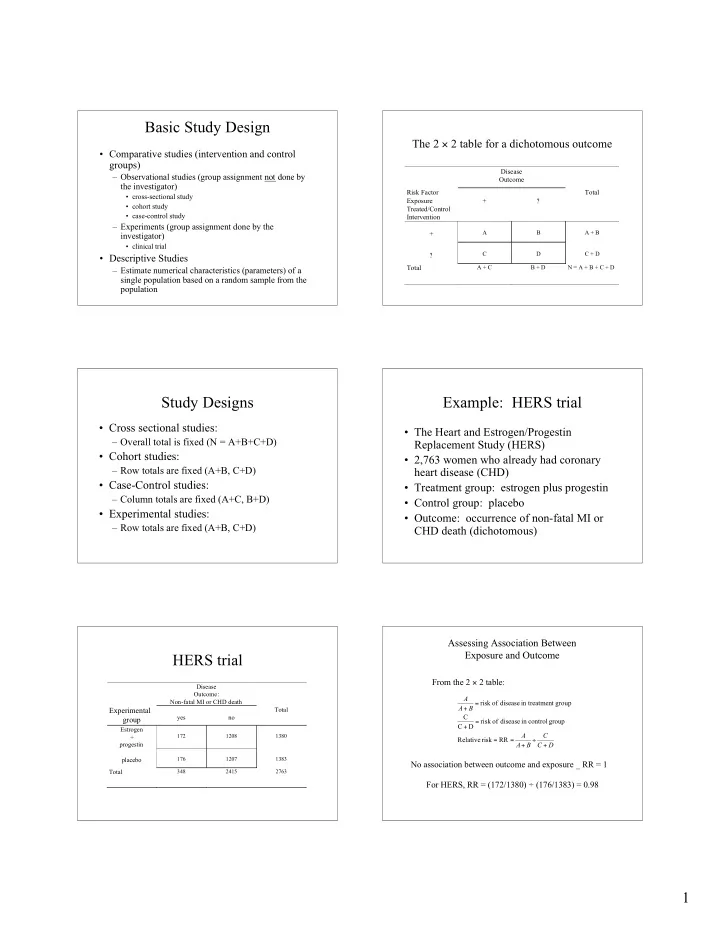
Basic Study Design The 2 × 2 table for a dichotomous outcome • Comparative studies (intervention and control groups) Disease – Observational studies (group assignment not done by Outcome the investigator) Risk Factor Total • cross-sectional study Exposure + ? • cohort study Treated/Control • case-control study Intervention – Experiments (group assignment done by the A B A + B + investigator) • clinical trial C D C + D ? • Descriptive Studies Total A + C B + D N = A + B + C + D – Estimate numerical characteristics (parameters) of a single population based on a random sample from the population Study Designs Example: HERS trial • Cross sectional studies: • The Heart and Estrogen/Progestin – Overall total is fixed (N = A+B+C+D) Replacement Study (HERS) • Cohort studies: • 2,763 women who already had coronary – Row totals are fixed (A+B, C+D) heart disease (CHD) • Case-Control studies: • Treatment group: estrogen plus progestin – Column totals are fixed (A+C, B+D) • Control group: placebo • Experimental studies: • Outcome: occurrence of non-fatal MI or – Row totals are fixed (A+B, C+D) CHD death (dichotomous) Assessing Association Between Exposure and Outcome HERS trial From the 2 × 2 table: Disease Outcome: A Non-fatal MI or CHD death risk of disease in treatme nt group = A B + Experimental Total yes no C group risk of disease in control group = C D + Estrogen A C 172 1208 1380 + Relative risk RR = = ÷ progestin A B C D + + placebo 176 1207 1383 No association between outcome and exposure _ RR = 1 Total 348 2415 2763 For HERS, RR = (172/1380) ÷ (176/1383) = 0.98 1
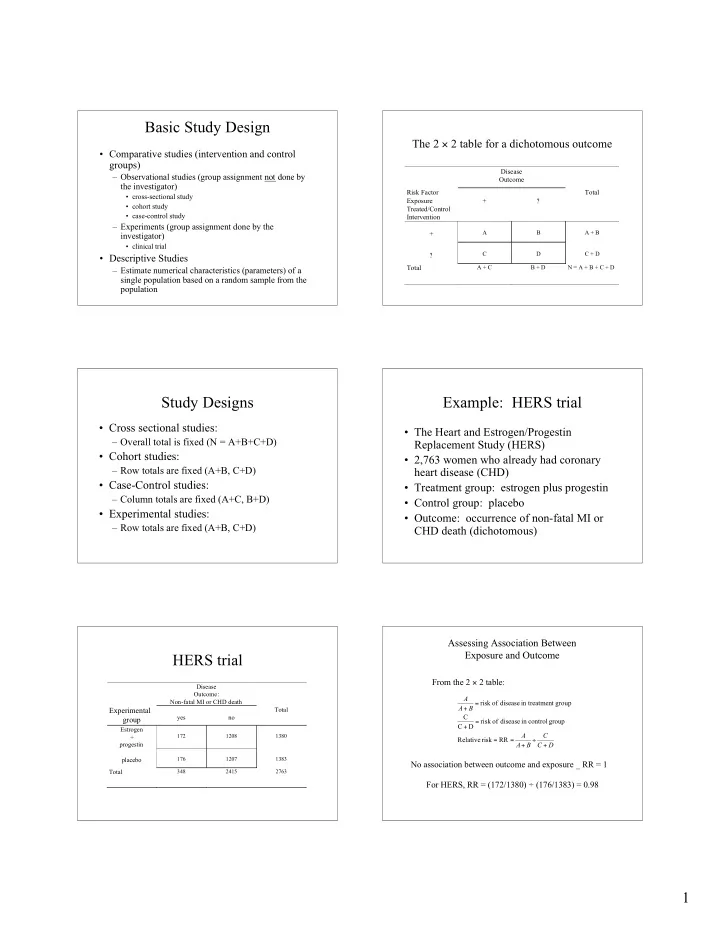
Assessing Association Between Assessing Association Between Exposure and Outcome Exposure and Outcome A odds in favor of disease in the treatment group = B C odds in favor of disease in the control group A C = Risk difference RD = = − D A B C D + + A / B Odds ratio OR = = No association between outcome and exposure _ RD = 0 C / D No association between outcome and exposure _ OR = 1 For HERS, RD = (172/1380) − (176/1383) = − 0.003 For HERS, OR = (172/1208)/(176/1207) = 0.98 Basic Study Design Basic Study Design • Randomized control studies – Sound scientific clinical investigation almost always • Issues in randomized control studies demands that a control group be used against which the – ethical new intervention can be compared. Randomization is the preferred way of assigning participants to control • treat the patient with the intervention believed to be and intervention groups. best – Why use random assignment? • clinical equipoise • avoids bias (investigator or participant may influence choice of intervention) – for rare outcomes, other designs are necessary • produces comparable groups (controls confounding variables (case-control study) (known and unknown): variables associated with both the outcome and the intervention) • makes statistical inference possible Assignment of subjects to groups: Basic Study Design Randomization • Group allocation designs • fixed allocation – Unit of randomization is a group – simple • example: clinic, pharmacy, community – blocked – Sample size is number of groups, not the – stratified randomization number of individuals within groups (not always efficient) 2
Randomization Randomization • Fixed allocation randomization • Fixed allocation randomization – Blocked randomization – Assign subjects to intervention with a fixed probability • example: blocks of size 4 (usually 0.5). – Simple randomization AABB, ABAB, BAAB, BABA, BBAA, ABBA • toss a fair coin • alternate method • random number table • computer (pseudo-random number generator) Assignment Random number Rank • can be extended to more than two groups A 0.069 1 • can result in groups of different sizes A 0.734 3 – not a problem for analyses – does affect efficiency B 0.867 4 B 0.312 2 Randomization Randomization • Fixed allocation randomization • Fixed allocation randomization – Stratified randomization – Blocked randomization • prognostic factors should be evenly distributed between • guarantees groups will differ by no more than b /2 treatment groups to make them comparable • randomization guarantees this on average members ( b = block size) • to ensure groups are comparable, stratify then randomize • strictly speaking, analysis should account for • in multi-center trials, center is used to stratify blocking (if not, it is conservative) – Example: 3 prognostic factors • age (40-49, 50-59, 60-69) • sex (F, M) • smoking status (current, ex-smoker, never) Randomization Randomization – Example: stratified allocation • The analysis of a trial which used stratified random allocation should include the Strata Age Sex Smoking Group assignment 1 40-49 M Current ABBA BABA . . . stratification variables. 2 40-49 M Ex BABA BBAA . . . 3 40-49 M Never etc. • If randomization was not stratified, it is still 4 40-49 F Current 5 40-49 F Ex 6 40-49 F Never possible to control the effects of prognostic 7 50-59 M Current 8 50-59 M Ex variables in the analysis phase. 9 50-59 M Never 10 50-59 F Current 11 50-59 F Ex 12 50-59 F Never etc. 3
Blindness Blindness • unblinded trials • Definition: Bias is systematic error: the difference between the true value and that actually obtained due to all • single blinded trials causes other than sampling variability. • double blinded trials – Can occur consciously or unconsciously. – Can occur anywhere in a trial from initial design through analysis • triple blinded trials and interpretation. • Solution: blind investigator and participant with respect to intervention assigned. • Other aspects of trial can be blinded as well: assessment, classification, and evaluation of outcome. Blindness Blindness • Unblinded trials – Both investigator and participant know to which • Single-blinded trials intervention the participant has been assigned. – Investigators know which intervention each • surgery participant is receiving. • changes in lifestyle • devices – Simpler, admits decision-making ability of – Simpler to execute than blinded study. investigators. – Investigators more comfortable with decisions such as – Bias is reduced, but possible. whether or not to continue a participant on a given • administration of therapy medication. • data collection and assessment – Bias is possible. • control participants may drop out • concomitant therapy differentially applied • reporting of symptoms and side effects biased Blindness Blindness • Double-blind studies • Triple-blind studies – Neither participants nor investigators know the – Same a double-blind plus the committee monitoring identity of the intervention assignment. outcomes does not know treatment assignment. – Not always a good idea; if ensuring patient safety, – Bias reduced. blinding may be counterproductive. – Placebo used in control group. – A study might need to be stopped if there is a clear • Placebo should be used if no standard therapy is difference between the groups in an adverse direction; superior to placebo. knowledge of the intervention group would be • Applicants should understand they might receive necessary. placebo. 4
Recommend
More recommend