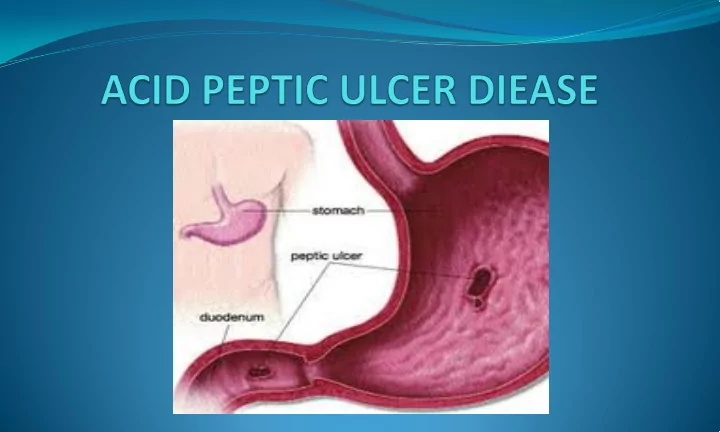
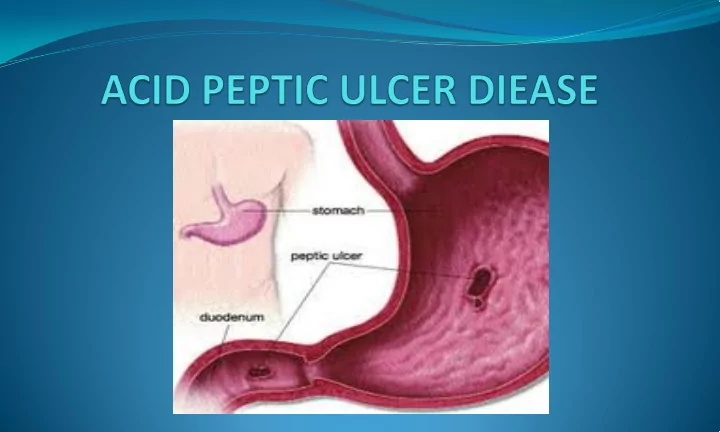
An eroded lesion in either the esophageal, gastric, or duodenal mucosa resulting from the action of gastric secretions and typically H.pulori bacterial inflammation.
• Normal gastric and duodenal mucosa is protected from the digestive actions of acid and pepsin by the secretion of mucus, the production of bicarbonate, the removal of excess acid by normal blood flow, and the rapid renewal and repair of epithelial cell injury. • Peptic ulcer refers to an ulcer that occurs as a result of the breakdown of these normal defense and repair mechanisms. • Typically more than one of the mechanisms must be malfunctioning for symptomatic peptic ulcer to develop. • Peptic ulcer typically show evidence of chronic inflammation and repair processes surrounding the lesion.
Acid peptic ulcer may develop due to any of the following reasons. • H.pylori infection. • Increased number of parietal cell or acid secretion. • Increased gastric emptying rates. • Reduced ability of the duodenum to handle an acid load. • Stress • Excessive use of non steroidal anti inflammatory drugs (NSAID) and corticosteroids.
• Increased gastric tone and painful hunger contraction when stomach is empty. • Piercing, burning and gnawing pain which usually relieved by taking food. • Frequent vomiting sometimes with blood too. • Anorexia
• Gastrointestinal bleeding • Intestinal perforation • Peritonitis (inflammation of the lining of abdominal cavity) • Anemia • Intestinal narrowing and obstruction • Shock
• Restoration of good nutritional status with dietary modifications and counseling. • Alleviate the symptoms. • Neutralize acids. • Reduce acid secretion. • Preservation of epithelial resistance to the destructive action of gastric juices.
• Milk neutralizes gastric acidity only for 20 to 60 minutes after its ingestion and the PH reverts back to the basal levels. Current studies indicate that a diet with high milk content has an adverse effect on the healing rate of ulcer because of high calcium. So protein from cottage cheese, egg, chicken and fish in adequate amounts is beneficial for regeneration of cell. Additional protein 10-15g/day above the RDA can be given. • The products of fat digestion in the small intestine stimulate entrogastrone, which inhibits gastric juice secretion. PUFA such as linoleic and eicosapentanoic acid have been found to effective against duodenal ulcer by inhibiting in vitro growth of H.Pylori. Around 25-30 g visible fat in emulsified form can be given. Avoid fried foods as they cause digestive problems.
• 55 to 65% of CHO can be given in simple and complex form but in soft well cooked form. Soluble fiber is more beneficial than insoluble as insoluble fiber delays gastric emptying time hence prevents the mucosal damage by acidic gastric juice. • Fruits in general are related to an alkaline ash diet. If they are not well tolerated by some individuals, avoid them. • Avoid taking alcohol, caffeine, black pepper ad meat extracts as they significantly change gastric pH. • Clinical observations have shown that tolerance for a variety of standard foods is highly individual. Pulse, soyabean, cabbage, cauliflower, onions, peas, apple, watermelon are some of the foods identified.
• Cigarette smoking cause an adverse effect because of the presence of nicotine which cause pyloric incompetence, increased reflux of duodenal juice into the stomach, increased gastric acid secretion by favoring gastric secretion, decrease pancreatic bicarbonate synthesis.
Stage 1 • Initially, for bleeding ulcer, if the patient is extremely nauseated or vomiting he must be kept NBM • This is followed by an hourly feeding to begin with milk and cream 100g/hr followed by small feeding of easily digestible food like soft cooked eggs, custards, refined flour products, cottage cheese, low fiber vegetables like gourds, clear soup with no seasoning and herbs, soft over ripe fruit whips and light desserts. • The diet must be feed orally and of liquid/semi liquid/ soft consistency which is easy to digest
Stage 2 • Marked recovery from pain. • 6 meal pattern followed. • Light, blend, low fiber diet. • Mechanical/ thermal, chemical irritation of gastric mucosa to be avoided. • Late night feeding avoided as the end products of digestion may cause the epigastric pain.
Stage 3 • Number of feeds reduced to 3-4. • Discharged from hospital – discharged diet • Increased amount/ feed Stage 4 • Liberalizing the diet depending on the patient’s individual tolerance and schedule. • Ensuring optimum intake of calorie, protein, fats, vitamins and minerals. • Relaxed atmosphere on eating. • Lifestyle change.
Recommend
More recommend