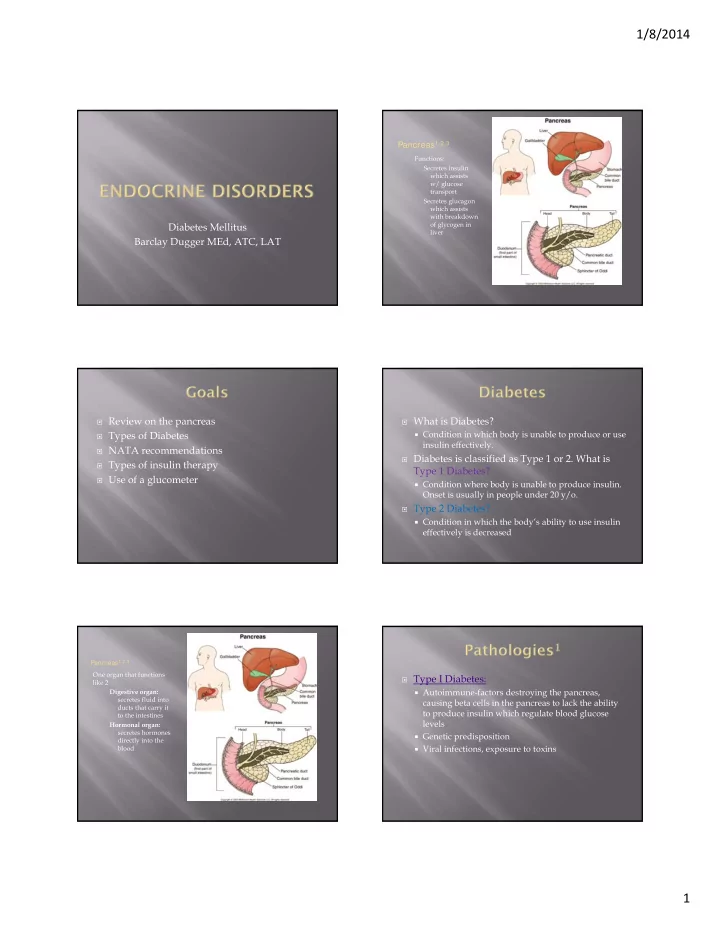
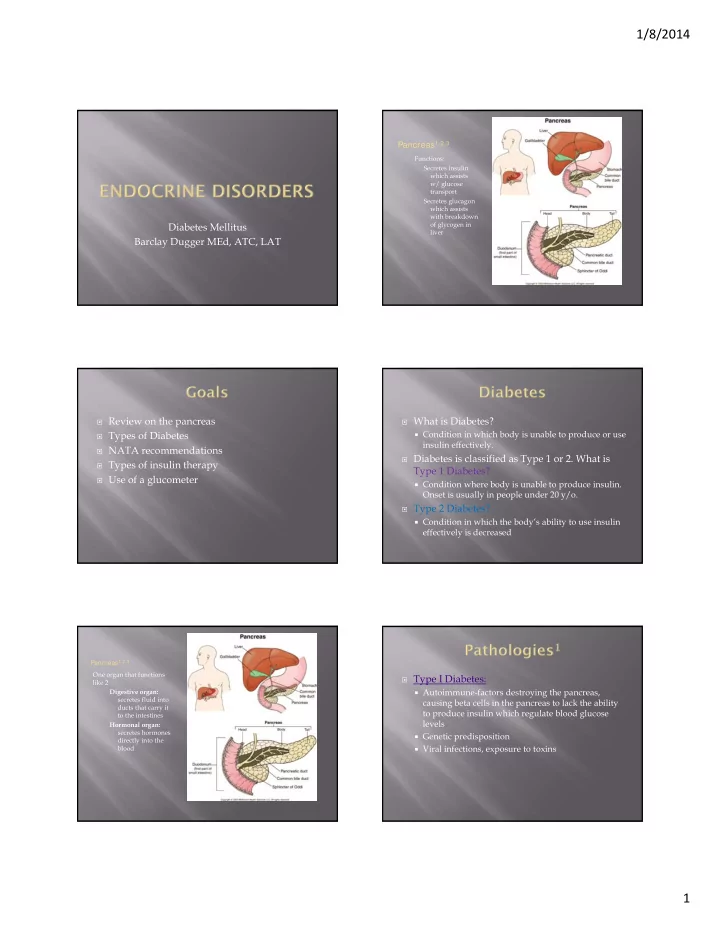
1/8/2014 Pancreas 1,2,3 Functions: Secretes insulin which assists w/ glucose transport Secretes glucagon which assists with breakdown Diabetes Mellitus of glycogen in liver Barclay Dugger MEd, ATC, LAT Review on the pancreas What is Diabetes? Condition in which body is unable to produce or use Types of Diabetes insulin effectively. NATA recommendations Diabetes is classified as Type 1 or 2. What is Types of insulin therapy Type 1 Diabetes? Use of a glucometer Condition where body is unable to produce insulin. Onset is usually in people under 20 y/o. Type 2 Diabetes? Condition in which the body’s ability to use insulin effectively is decreased Pancreas 1,2,3 One organ that functions Type I Diabetes: like 2 Digestive organ: Autoimmune-factors destroying the pancreas, secretes fluid into causing beta cells in the pancreas to lack the ability ducts that carry it to produce insulin which regulate blood glucose to the intestines levels Hormonal organ: secretes hormones Genetic predisposition directly into the blood Viral infections, exposure to toxins 1
1/8/2014 Time Measurement Taken Blood Serum Levels Type II Diabetes: After fasting for 8 hours 60-80mm/dl What is it? Pancreas produces adequate insulin but insulin receptors are not working properly Complications-concerns? No cure; increased fat in blood, 2-3 hours after fasting 100-140 mm/dl commonly associated with obesity, ateriosclerosis, peripheral neuropathy, chronic infections, osteoporosis How can you detect it? Monitoring blood glucose levels Random and unplanned Less than 126 Normal Blood Glucose Levels Type I & Type II Diabetes: Signs/symptoms? Polydipsia (excessive thirst) Polyphagia (excessive hunger) Polyuria (frequent urination) weight loss may present initially with ketoacidosis Abnormal Blood Glucose Levels Type I Diabetes: Each athlete with diabetes should have a diabetes care plan that includes blood glucose What is ketoacidosis? monitoring and insulin guidelines, treatment When the body is unable to move glucose from the blood to the cells, it turns to fats as an energy source guidelines for hypoglycemia and Ketones are produced as a by product of the breakdown of hyperglycemia, and emergency contact fats for fuel information. These toxic acids build up in the blood and eventually spill over into the urine Ketones are responsible for the fruity odor noticed on the breaths of persons suffering from extreme hyperglycemia and DKA 2
1/8/2014 Hyperglycemia can present with or without Hypoglycemia typically presents with ketosis. Typical signs and symptoms of tachycardia, sweating, palpitations, hunger, hyperglycemia without ketosis include nausea, nervousness, headache, trembling, or dizziness; dehydration, reduced cognitive performance, in severe cases, loss of consciousness and death feelings of sluggishness, and fatigue. can occur. Hyperglycemia with ketoacidosis may include the signs and symptoms listed earlier as well as Kussmaul breathing (abnormally deep, very rapid sighing respirations characteristic of diabetic ketoacidosis), fruity odor to the breath, unusual fatigue, sleepiness, loss of appetite, increased thirst, and frequent urination. Mild hypoglycemia (the athlete is conscious Type I-insulin injections and able to swallow and follow directions) is Type II-diet and exercise treated by administering approximately 10–15 g of carbohydrates (examples include 4–8 glucose tablets or 2 tablespoons of honey) and reassessing blood glucose levels immediately and 15 minutes later. Rapid-acting Severe hypoglycemia (the athlete is unconscious or unable to swallow or follow Short-acting directions) is a medical emergency, requiring Intermediate-acting activation of emergency medical services Long acting (EMS) and, if the health care provider is Pre-mixed properly trained, administering glucagon. Onset: The amount of time insulin takes to Physicians should determine a safe blood enter blood stream. glucose range to return an athlete to play after Peak: Time when insulin is most effective. an episode of mild hypoglycemia or Duration: How long the insulin lowers blood hyperglycemia. sugar. 3
1/8/2014 Rapid-acting- Used at time of meal Long-acting: About a full day Onset= 15-30 minutes Onset= 30” – 3 hours Peak= 30-90 Peak= 6-20 hours Duration= 1-5 hours Duration= 24-36 hours Drug Name: Humalog, Lispro, Novolog, Aspart, Drugs Names: Ultralente, Lantus, Levemir, Glulisine. Detemir. Short-acting: Used from a meal to within 1 Pre-mixed: Used twice a day or before meals hour Onset= 10-30”, time it takes to enter blood stream Onset= 30” – 1 hour Peak= 30”-12 hours, when most effective Peak= 2-5 hours Duration= 14-24 hours, how long it lowers blood Duration= 2-8 hours sugar Drug Name: Novolin, Vesolulin(insulin pump) Drug Names: Humulin 70/30, Humulin 50/50, Novolin 70/30, Novolog 50/50, Intermediate-acting: Used for half a day or http://www.youtube.com/watch?v=s8nzOrbe before sleep M5Q Onset= 1-2.5 hours Peak= 3-12 hours Duration= 18-24 hours Drugs Name: Lente (L) 4
1/8/2014 Jimenez, C., Corcoran, M.H., Crawley, J.T., Hornsby, W.G., Peer, K. S., Philbin, R.D., & Riddell, M.C. (2007). National athletic trainers’ association position statement: management of the athlete with type I diabetes mellitus. Journal of Athletic Training, 42 (4), 536-545 Cuppetta, M., Walsh, K. M. (2012) General Medical Conditions in the Athlete (Second Edition) Elsevier-Mosby 5
1/8/2014 The upper respiratory tract: Nasal passages Paranasal sinuses Pharynx Larynx Responsible for warming, humidifying, and filtering the air as it reaches the lower respiratory tract The lower respiratory tract: Trachea Right and left bronchi Lung parenchyma Overview of pulmonary system History and Inspection The first step is to take a thorough history; it Evaluation of patient with breathing difficultly includes questions about how long a problem has Auscultation of lung sounds existed, what exacerbates the condition, and the severity of symptoms. Asthma Describe the characteristics of the condition, and Exercise Induced Bronchospasm timing of it; shortness of breath should also be noted. Spirometer use The chest is inspected after the history is taken. The examiner inspects the chest for shape and Nebulizer use configuration, including any skeletal deformities, as well as bruising of the ribs or chest wall. The pulmonary system is involved primarily in Respiratory Patterns Tachypnea: Refers to breathing that has become more rapid than the exchange of oxygen and carbon dioxide, 24 breaths per minute which are vital in the production of the energy Hyperpnea: Refers to a type of tachypnea in which breaths are involved in metabolism at the cellular level. usually large and deep, resulting in hyperventilation Bradypnea: When breathing slows to fewer than 12 breaths per Respiration can be divided into ventilation and minute oxygenation. Hypopnea: When breathing becomes slow and shallow and is seen in an adaptive response to painful situations, such as rib a. During ventilation, air moves through the fractures Dyspnea: Refers to the subjective sensation of difficulty in respiratory tract. breathing or shortness of breath Orthopnea: Describes a type of dyspnea that begins or increases as the patient lies down 1
1/8/2014 Respiration Patterns Bronchial breath sounds are loud, high-pitched, and predominantly expiratory. Breathing involves several simultaneous patterns. These sounds represent air moving through large airways and sound Decreases in pH as well as corresponding increases more tubular. in carbon dioxide result from normal cellular Normally heard over the trachea metabolism and stimulate an increase in ventilation Bronchiovesicular breath sounds are heard when air moves to remove these by-products. through medium-sized airways, such as the mainstem bronchi. Neural control of breathing comes from the phrenic Can be heard both anteriorly and posteriorly, toward the center of the thorax nerve, which arises from cervical nerve roots C3, C4, Sounds are of medium pitch and moderate intensity. and C5. Vesicular breath sounds predominate in most of the peripheral lung tissue and represent the air as it moves into the smaller airways, such as the bronchioles. These sounds are soft, low-pitched noises that involve mostly inspiration. Auscultation Auscultation is the skilled listening by a trained ear for sounds produced by the body. Perform auscultation after history, observation, and palpation in order to gather as much information as possible first. Perform in a quiet environment. Listen for the presence or absence of sounds as well as their frequency, loudness, quality, and duration. Make sure the earpieces of the stethoscope fit comfortably, and point the earpieces toward the face. https://www.youtube.com/watch?v=yFWWS IGB6-0 The examiner must listen systematically at each position throughout inspiration and expiration https://www.youtube.com/watch?v=O2yOP and evaluate lungs in the anterior, posterior, O0NBnM and lateral aspects to ensure that each lobe of the lungs is properly examined. When the athletic trainer listens to the lungs, three different sounds can be appreciated in normal individuals. 2
Recommend
More recommend