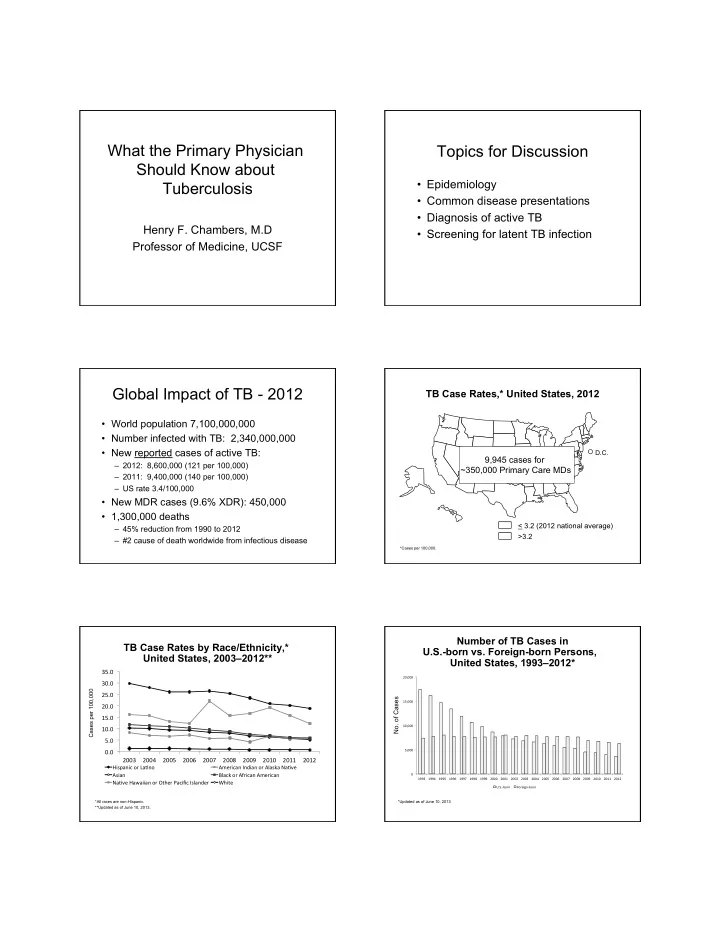
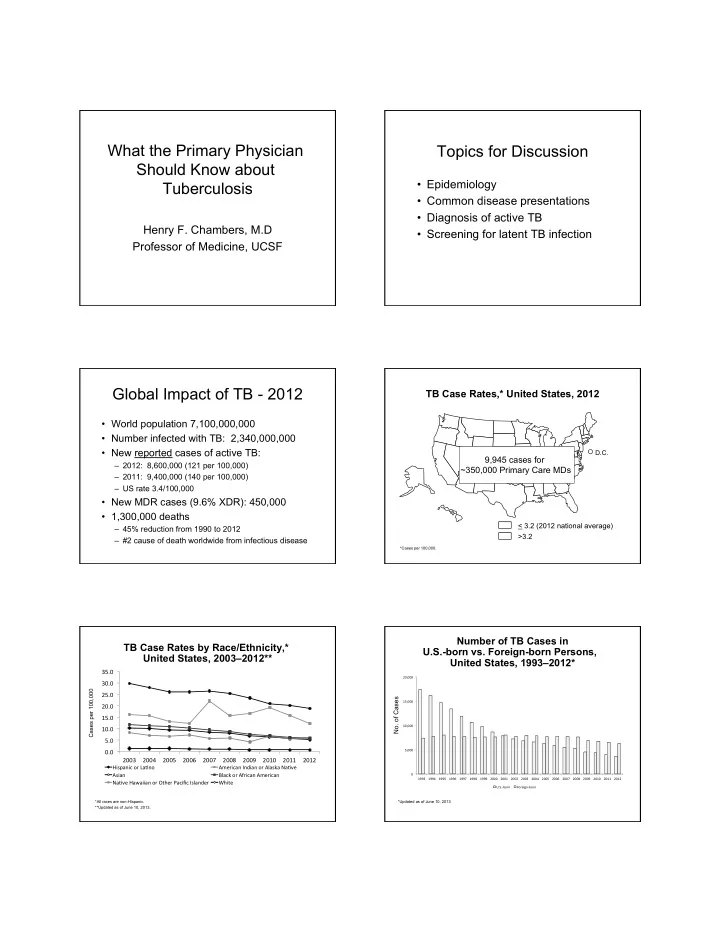
What the Primary Physician Topics for Discussion Should Know about • Epidemiology Tuberculosis • Common disease presentations • Diagnosis of active TB Henry F. Chambers, M.D • Screening for latent TB infection Professor of Medicine, UCSF Global Impact of TB - 2012 TB Case Rates,* United States, 2012 • World population 7,100,000,000 • Number infected with TB: 2,340,000,000 • New reported cases of active TB: D.C. 9,945 cases for – 2012: 8,600,000 (121 per 100,000) ~350,000 Primary Care MDs – 2011: 9,400,000 (140 per 100,000) – US rate 3.4/100,000 • New MDR cases (9.6% XDR): 450,000 • 1,300,000 deaths < 3.2 (2012 national average) – 45% reduction from 1990 to 2012 >3.2 – #2 cause of death worldwide from infectious disease *Cases per 100,000. Number of TB Cases in TB Case Rates by Race/Ethnicity,* U.S.-born vs. Foreign-born Persons, United States, 2003–2012** United States, 1993–2012* 35.0 ¡ 20,000 ¡ 30.0 ¡ Cases per 100,000 25.0 ¡ No. of Cases 15,000 ¡ 20.0 ¡ 15.0 ¡ 10,000 ¡ 10.0 ¡ 5.0 ¡ 0.0 ¡ 5,000 ¡ 2003 ¡ 2004 ¡ 2005 ¡ 2006 ¡ 2007 ¡ 2008 ¡ 2009 ¡ 2010 ¡ 2011 ¡ 2012 ¡ Hispanic ¡or ¡La7no ¡ American ¡Indian ¡or ¡Alaska ¡Na7ve ¡ Asian ¡ Black ¡or ¡African ¡American ¡ 0 ¡ 1993 ¡ 1994 ¡ 1995 ¡ 1996 ¡ 1997 ¡ 1998 ¡ 1999 ¡ 2000 ¡ 2001 ¡ 2002 ¡ 2003 ¡ 2004 ¡ 2005 ¡ 2006 ¡ 2007 ¡ 2008 ¡ 2009 ¡ 2010 ¡ 2011 ¡ 2012 ¡ Na7ve ¡Hawaiian ¡or ¡Other ¡Pacific ¡Islander ¡ White ¡ U.S.-‑born ¡ Foreign-‑born ¡ *All races are non-Hispanic. *Updated as of June 10, 2013 **Updated as of June 10, 2013.
Trends in TB Cases in Foreign-born Persons, TB Case Rates by Age Group and Sex, United States, 1992 – 2012* United States, 2012 No. of Cases Percentage 8.0 10,000 ¡ 70 ¡ 7.0 9,000 ¡ 60 ¡ Cases per 100,000 8,000 ¡ 6.0 50 ¡ 7,000 ¡ 5.0 6,000 ¡ 40 ¡ 4.0 5,000 ¡ 30 ¡ 3.0 4,000 ¡ 3,000 ¡ 20 ¡ 2.0 2,000 ¡ 10 ¡ 1.0 1,000 ¡ 0.0 0 ¡ 0 ¡ 2 ¡ 3 ¡ 4 ¡ 5 ¡ 6 ¡ 7 ¡ 8 ¡ 9 ¡ 0 ¡ 1 ¡ 2 ¡ 3 ¡ 4 ¡ 5 ¡ 6 ¡ 7 ¡ 8 ¡ 9 ¡ 0 ¡ 1 ¡ 2 ¡ Under 5 5 - 14 15 - 24 25 - 44 45 - 64 ≥ 65 9 9 9 9 9 9 9 9 0 0 0 0 0 0 0 0 0 0 1 1 1 9 9 9 9 9 9 9 9 0 0 0 0 0 0 0 0 0 0 0 0 0 1 1 1 1 1 1 1 1 2 2 2 2 2 2 2 2 2 2 2 2 2 Male Female Number ¡of ¡Cases ¡ Percentage ¡of ¡Total ¡Cases ¡ *Updated as of June 10, 2013 Active Tuberculosis Sites of TB Infection 120 • Pulmonary tuberculosis: 85% of all 100 Extrapulmonary cases Pulmonary 80 Percent Other • The infectious form of the disease 60 Bone/jt • Clinical suspicion based on Miliary 40 GU – Signs, symptoms, setting Pleural 20 – Chest x-ray Lymphatic 0 All cases Expul Case Presentation • 63 y/o inmate transferred from jail for r/o TB • No fever, cough, weight loss • 12 mm + PPD, HIV negative • Prior work-up – 2/2001: AFB smear/culture neg x3 – 4/2005: AFB smear/culture neg x3 – 8/2005: AFB smear/culture neg x3 – 3/2010: AFB smear/culture neg x1 – 9/2010: AFB smear/culture neg x4 CXR: LUL nodular infiltrate, slight volume loss, maybe slightly worse since prior film
Work-Up What is your estimate of the likelihood of active TB in this case? • CXR: LUL nodular infiltrate, slight 1. 75% or higher volume loss, maybe slightly worse 2. 50-75% since prior film? 3. 25-50% • Sputum examination 4. 5-25% – Routine: OF on culture and Gram-stain – AFB x2 and BAL x1: no AFB 5. < 5% – GenProbe Amplified MTD test: negative What is your revised estimate of the likelihood of active TB in this case? 1. 75% or higher Diagnosis of TB 2. 50-75% 3. 25-50% 4. 5-25% 5. < 5%
Performance of Diagnostic Tests Xpert MTB/RIF Test Performance for Pulmonary TB Sensitivity Specificity Sensitivity Specificity Smear pos. TB 95-98% AFB smear 60% 99% 99% NAA test 85% 99% Smear neg. TB 60-72% Culture 90% 99% Rifampin “R” 98-99% 99-100% PPD (or QTF) 60% 10% NEJM 361:1005, 2010; Am J Crit Care Med 184:132, 2011 Detection Thresholds of Tests Organism Burden in TB for TB Diagnosis Cavitary TB 10 6 - 10 7 cfu/g Positive smear 10 4 - 10 5 cfu/ml Pulmonary infiltrate 10 4 - 10 5 cfu/g Positive NAA test 10 1 - 10 2 cfu/ml Lymphadenopathy 10 2 - 10 4 cfu/g Positive culture 10 1 cfu/ml Performance of NAAT for Diagnosis of Pulmonary TB Clinical Course Pre-test PPV NPV probability • Patient was discharged back to jail 90% 100% 43% • Treatment for tuberculosis withheld pending results of work-up 75% 98% 69% • 16 days after discharge, one sputum culture and the BAL specimen were 50% 96% 87% reported positive for Mtb! 25% 91% 95% 5% 57% 99%
Forms of Extrapulmonary Tuberculosis Extrapulmonary TB • Cervical lymphadenitis • Tuberculous pleuritis • Other rarer birds Differential Dx of Cervical Adenitis Tuberculous Adenitis • Tuberculosis • Clinically presentation not distinctive • Non-tuberculous mycobacterial infection • Constitutional symptoms not usually present • Kikuchi-Fujimoto’s syndrome (histiocytic • Seen in children, young adults > adults necrotizing lymphadenitis) • PPD + in 75-80% • Staph or strep infection • Chest x-ray abnormality (15-20%) favors • Cat scratch MTB • Lymphoma, other tumor • Foreign-born patient more likely to have • Other: syphilis, HIV, tularemia, listeria, MTB plague
Diagnosis of TB Adenitis Work-up of Suspected TB Adenitis • Tissue is the issue • Tuberculin test – to exclude other etiologies • Check HIV serology – for sensitivity testing • Chest x-ray to r/o pulmonary TB • FNA • Respiratory isolation for patients with – Characteristic granulomas in 80% pulmonary symptoms, pulmonary TB – Culture + in 40-70% – Smear + < 50% • Notify tuberculosis control • Biopsy: partial vs. total excision Similar Scenario for TB Pleuritis Treatment of TB Cervical Adenitis • Responsive to medical therapy alone • Unilateral, benign, lymphocytic effusion • If excisional surgery performed, • Primary infection, newly + PPD medical therapy still must be given • Fluid usually smear and culture • Paradoxical “worsening” can occur; negative needle aspiration effective • Pleural biopsy culture positive ~60%, management with granulomas ~80% • Sinus track formation, non-healing • Treat as for adenitis or pulmonary TB wounds may benefit from surgery Bedaquiline Principles of Therapy • Treatment of TB caused by MDR or • Start 4 drugs (RIPE) for suspected active TB XDR strains of MTBtuberculosis • Never use a single drug for treating active TB: • DOT: 400 mg once daily for 2 weeks, resistance can emerge (1 mutant in 10 4 to 10 6 ) then 200 mg 3 x/week for 22 weeks, • Never add a single drug to a failing regimen – Taken with food and • Consult and expert and/or local health department – Always in combination with other anti-TB medications. • Francis Curry National TB Center: http:// www.nationaltbcenter.edu/ • Monitor for QTc prolongation Lancet 380:986, 2012; Antimicrob Agents Chemother 56:3271, 2012; NEJM 360:2397, 2009
Case Presentation • LV is a 58 y/o female from Ukraine referred for treatment of hypertension Screening for Latent TB and diabetes Infection (LTBI) • She is otherwise well • She gives a history of BCG vaccination as a teen What is the best course of action? LTBI: Goals of Screening 1. The patient should be screened for LTBI with a tuberculin test 2. The patient should not be screened for LTBI • Identify active cases because she is not a candidate for INH • Identify infected persons likely to benefit prophylaxis due to her age 3. The patient should not be screened because from treatment of latent TB infection with prior BCG vaccination the tuberculin test will (LTBI) be false positive • Surveillance 4. The patient should be screened for LTBI by chest x-ray Increased Risk of Infection Who Should Be Screened? • Recent contacts of an active TB case – About 30% are infected • Foreign-born persons from high TB • Persons with increased risk of TB infection prevalence areas • Persons with increased risk of progression – Asia, Mexico, Middle East, Central and South • Not the general population America, Africa, Eastern Europe • Medically underserved, low-income, racial and ethnic minorities • Others: HCW, residents of congregate living settings
Recommend
More recommend