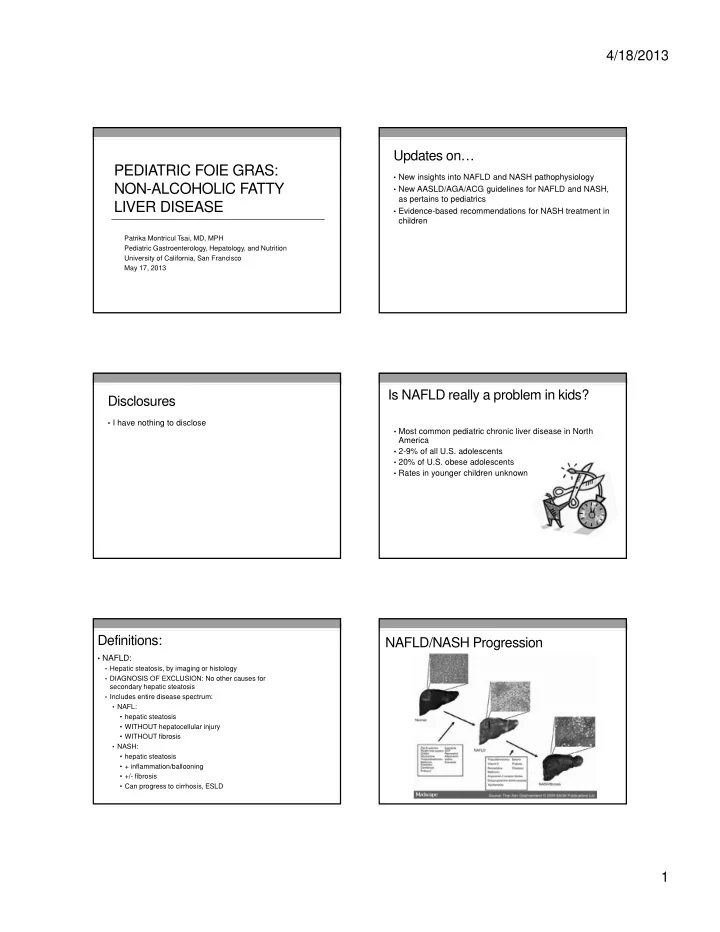
4/18/2013 Updates on… PEDIATRIC FOIE GRAS: • New insights into NAFLD and NASH pathophysiology NON-ALCOHOLIC FATTY • New AASLD/AGA/ACG guidelines for NAFLD and NASH, as pertains to pediatrics LIVER DISEASE • Evidence-based recommendations for NASH treatment in children Patrika Montricul Tsai, MD, MPH Pediatric Gastroenterology, Hepatology, and Nutrition University of California, San Francisco May 17, 2013 Is NAFLD really a problem in kids? Disclosures • I have nothing to disclose • Most common pediatric chronic liver disease in North America • 2-9% of all U.S. adolescents • 20% of U.S. obese adolescents • Rates in younger children unknown Definitions: NAFLD/NASH Progression • NAFLD: • Hepatic steatosis, by imaging or histology • DIAGNOSIS OF EXCLUSION: No other causes for secondary hepatic steatosis • Includes entire disease spectrum: • NAFL: • hepatic steatosis • WITHOUT hepatocellular injury • WITHOUT fibrosis • NASH: • hepatic steatosis • + inflammation/ballooning • +/- fibrosis • Can progress to cirrhosis, ESLD 1
4/18/2013 Histology of NASH Pediatric NAFLD: Type 1 vs. Type 2 • Type 1 NAFLD : • Type 2 NAFLD : • “Adult-type” • ?Unique to children • Zone 3 steatosis • Zone 1 steatosis • Ballooning • No ballooning • Perisinusoidal fibrosis • Portal inflammation/fibrosis Loomba et al. HEPATOLOGY 2009;50:1282-1293 NAFLD Pathogenesis Natural history of NAFLD • Not well understood Two-hit hypothesis Lipotoxicity hypothesis • In adults, NASH associated with: • Increased overall mortality risk • Leading cause of death: cardiovascular disease • Increased liver-mortality rate • NASH cirrhosis: Increased HCC risk (but lower than Hep C cirrhosis) • In children: 1 retrospective single center study • 66 children • 5 with serial biopsies, 4 with fibrosis progression Mantena SK et al. 2008 Bass NM. Hepatology 2010. Which of the following groups is protected Demographic Predictors of NAFLD from NAFLD? • A) African Americans • Overweight/obesity • B) Asian Americans • Adolescents • C) Hispanic Americans • Males > Females: • Estrogen protective? • D) None of the above • Ethnicity: • Hispanics, Asians AT RISK • African Americans PROTECTED • Family history: obesity, insulin resistance/DM, NAFLD Loomba R et al. Advances in Pediatric NAFLD. Hepatology . 2009; 50(4): 1282–1293. 2
4/18/2013 New NAFLD guidelines: June 2012 Grading of recommendations, evidence • Strength of Recommendation : factors include evidence quality, importance to patient outcomes, and cost STRONG 1. 2. WEAK • Quality of Evidence • High (A): Further research unlikely to change confidence in the estimate of the clinical effect • Moderate (B): Further research may change confidence in estimate of the clinical effect • Low (C): Further research very likely to impact confidence on the estimate of clinical effect AAP Guidelines for NAFLD Screening AASLD: NAFLD screening? • Starting at 10 years of age, every 2 years • Not recommended in adult primary care clinics or high-risk specialty clinics (diabetes, obesity) (1, B) • AST/ALT in pediatric patients with: • BMI>85 th percentile for age/gender WITH risk factors OR • Not recommended in overweight/obese children: • BMI>95 th percentile for age/gender, regardless of risk factors • “Due to a paucity of evidence, a formal recommendation cannot be • Risk factors: made with regards to screening for NAFLD in overweight and obese children despite a recent expert committee recommendation • Family history of obesity-related diseases, including hypertension, for biannual screening.” (1, B) early cardiovascular deaths, and strokes • Not recommended for family members of people with • Patient history of elevated blood pressure, hyperlipidemia, or tobacco use. NAFLD or NASH (1, B) • 18% of NASH patients have a first degree relative with NASH Pediatrics. December 2007, pp. S164-S192, S193-S228 Initial evaluation What are “normal” LFTS? • AST/ALT • Does NOT correlate well with presence or severity of NASH • Screening ALT for Elevation in Today’s Youth (SAFETY) • Medication history • Family history • U.S. children’s hospitals: • Alcohol screen for adolescents • Median ALT (range): • ALL: 53 (30-90) • BOYS: 50 (30-70) • GIRLS: 40 (29-65) AND Viral hepatitis: • NHANES: 12-17 yrs w/o liver disease • Hep A total Ab • 95 th percentile ALT: • Hep B Sag, Cab, • BOYS: 25.8 U/L SAb, • Hep C Ab • GIRLS: 22.1 U/L Schwimmer JB et al. Gastroenterology 2010. 3
4/18/2013 Ultrasound for hepatic steatosis Evaluation of incidental hepatic steatosis • History, clinical exam, LFTs • Signs/symptoms liver disease and/or abnormal LFTs: • Suspected NAFLD, further workup (1, A) • NO signs/symptoms liver disease AND normal LFTs: • Assess for metabolic risk factors (obesity, DM, dyslipidemia) (1, A) • NO liver biopsy recommended (1, B) Bohte AE et al. Radiology 2012; 262 (1): 327-334. MRI steatosis “color mapping” When to biopsy adults for NAFLD? Qayyum A et • “Should be considered in patients with NAFLD who are at al. AJR, increased risk to have steatohepatitis and advanced March 2012. fibrosis” (1, B) • Metabolic syndrome • NAFLD Fibrosis Score • “Patients with suspected NAFLD in whom competing etiologies for hepatic steatosis and co-existing chronic liver diseases cannot be excluded” (1, B) When to biopsy children for NAFLD? Approach to NAFLD workup and biopsy • AASLD: • “where the diagnosis of NAFLD is unclear” • “where there is possibility of multiple diagnoses” • “before starting potentially hepatotoxic medications” • “prior to starting pharmacologic therapy for NASH” • ESPGHAN: • “no present consensus or evidence base to formulate guidelines” • “to exclude other treatable disease” • “in cases of clinically suspected advanced liver disease” • “before pharmacologic/surgical treatment” • “as part of a structured intervention protocol or clinical research trial” 4
4/18/2013 Which of the following is not an effective Lifestyle modification to treat NAFLD: treatment for NAFLD? • A) Weight loss • Weight loss through lifestyle modification: • B) Exercise • 3-5%: reduced hepatic steatosis (1, B) • C) Vitamin E • 10%: reduced necro-inflammation (1, B) • D) Metformin • Improved steatosis, lobular inflammation, ballooning, and NAFLD activity score • Exercise alone, even without weight loss • Can significantly decrease hepatic steatosis (1, B) • 2-3 sessions/week, 30-60 minutes, 6-12 weeks • In children and adults, no evidence to definitively recommend a specific diet or exercise plan Pediatric NAFLD Vitamin E in adults: • Vitamin E: Recommended at 800 IU/day for biopsy-proven, • Treatment: non-diabetic ADULTS as first line therapy (1, B) • Lifestyle modification (2, B) • Anti-oxidant • Vitamin E: • Improves steatosis, inflammation, ballooning, NASH resolution • TONIC trial (NASH CRN): RCT of Vitamin E vs. metformin • Does NOT improve fibrosis vs. placebo x 96 weeks • NASH CRN trials (PIVENS, TONIC) suggest that rrr alpha-tocopherol at 800IU/day helpful • NO difference between groups in primary outcome: • Recommended daily allowance: 30 IU/day sustained ALT reduction • 2 previous meta-analyses failed to show histologic benefits • Vitamin E did significantly decrease NAS and improve • ?Increases all-cause mortality NASH resolution • Conflicting data from meta-analyses • Recent trial of 400 IU/day associated with increased prostate cancer risk • Recommendation : 800 IU rrr alpha-tocopherol daily for • NOT recommended in NASH + DM, NAFLD w/o liver biopsy, NASH children with biopsy-proven NASH or borderline NASH cirrhosis, cryptogenic cirrhosis, (1, C) NAFLD/NASH with other chronic liver (1, B) disease co-existing (1, B) Medications for NAFLD/NASH: Medications for NAFLD/NASH: • Metformin: Not recommended ( 1, A) • UDCA: Not recommended (1, B) • RCT data for both adults and children • Several small studies, 1 large RCT: no benefit • No effect on AST/ALT or liver histology • No effect regardless of diabetes as co-morbidity • Omega-3 fatty acids : Use to treat hypertriglyceridemia in • Rosiglitazone: Not recommended NASH patients, but not specifically to treat NAFLD/NASH • Increased risk coronary events • Less data than for pioglitazone, but does not seem to improve (1, B) inflammation or fibrosis (maybe AST/ALT, steatosis?) • Large multicenter study ongoing: eicosapentoic acid • Pioglitazone: Recommended in biopsy-proven, non- • Other studies small, flawed diabetic ADULTS (1, B) • Meta-analysis (Vernon G et al, 2011): • Improves steatosis: OR 4.05, 95% CI 2.58-6.35 • Statins : Use to treat dyslipidemia in NAFLD/NASH • Improves inflammation: OR 3.53, 95% CI 2.21-5.64 patients (1, B), but NOT as specific treatment for • Does NOT improve fibrosis: OR 1.40, 95% CI 0.87-2.24 • Causes weight gain NAFLD/NASH (1, B) 5
Recommend
More recommend