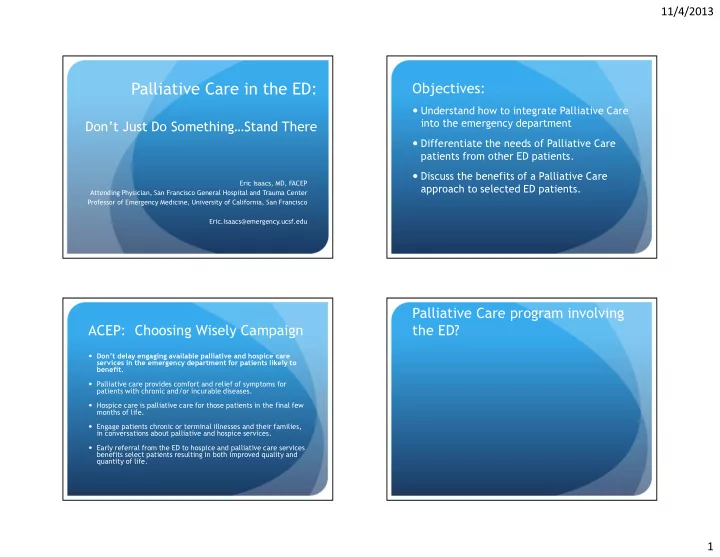
11/4/2013 Objectives: Palliative Care in the ED: � Understand how to integrate Palliative Care into the emergency department Don’t Just Do Something…Stand There � Differentiate the needs of Palliative Care patients from other ED patients. � Discuss the benefits of a Palliative Care Eric Isaacs, MD, FACEP approach to selected ED patients. Attending Physician, San Francisco General Hospital and Trauma Center Professor of Emergency Medicine, University of California, San Francisco Eric.Isaacs@emergency.ucsf.edu Palliative Care program involving ACEP: Choosing Wisely Campaign the ED? � Don’t delay engaging available palliative and hospice care services in the emergency department for patients likely to benefit. � Palliative care provides comfort and relief of symptoms for patients with chronic and/or incurable diseases. � Hospice care is palliative care for those patients in the final few months of life. � Engage patients chronic or terminal illnesses and their families, in conversations about palliative and hospice services. � Early referral from the ED to hospice and palliative care services benefits select patients resulting in both improved quality and quantity of life. 1
11/4/2013 When you hear “Palliative Care in Tension Points… the ED,” do you feel: � Bias towards action 1) Nervous? 2) This will be too difficult? � The Facts (or the lack thereof) 3) I am motivated to incorporate this? 4) All of the above � Emotional Issues � Communication Issues Reality Check: Provide Excellent Reality Check: Provide Excellent Care Care • Triage and disposition • Triage and disposition • Right care, right place, in a timely manner • Right care, right place, in a timely manner • Optimizing and efficiently using ED • Optimizing and efficiently using ED resources resources • Reducing ED length of stay • Reducing ED length of stay • Increasing ED throughput • Increasing ED throughput • Decreasing ED boarding of admitted patients • Decreasing ED boarding of admitted patients • Increasing patient/family satisfaction • Increasing patient/family satisfaction • Palliative Care can address all of these! 2
11/4/2013 Reality Check… Global trajectories How Many of you would like to die from: 1) Sudden death 2) Terminal illness 3) Organ failure 4) Frailty Lunney, Lynn, Foley et al., 2003 Lunney, Lynn, Foley et al., 2003 Global trajectories : How Many of you would like to die from: Case # 1: Yellow? Anyone home? � 56 year old male with a history of � Sudden death (6%) pancreatic cancer � Terminal illness � Brought in by his wife due to shortness of � Organ failure breath and fatigue � Frailty � He has a chemotherapy appointment on Tuesday and they want to get him tuned up � 80% want to die at home a bit so he can get his next dose of chemo � 17% die at home. 60% in hospitals and 20% SNF 3
11/4/2013 Case # 1: Yellow? Anyone home? Your Thoughts…? � Vital Signs: Temp 38.6 (oral), P . 110, BP . 92/48, RR 24 � As you walk into the room, � Patient is severely jaundiced � Abdomen very distended with ascites � Looks in mild respiratory distress � There are no beds; it will be 3 hours… Your Thoughts…? Your Thoughts…? � A-B-C IV-O2-Monitor � A-B-C IV-O2-Monitor � “WHY did she bring him to the ED?” � “WHY did she bring him to the ED?” � “Just get him upstairs” � “Just get him upstairs” � “%$#@!! Oncologists” � “%$#@!! Oncologists” � “We have some talking to do…” � “We have some talking to do…” 4
11/4/2013 Your Thoughts…? What is Palliative Care? � Intends neither to hasten or postpone death � A-B-C IV-O2-Monitor � Patient determined goals of care � “WHY did she bring him to the ED?” � Relief of pain and other distressing � “Just get him upstairs” symptoms � “%$#@!! Oncologists” � Includes psychological and spiritual � Involves patients and families � “We have some talking to do…” � Support an understanding of disease process � Palliative Care in the ED Palliative Care “Integration” in Models of Palliative Care the Emergency Department � Palliative Care consultant comes to the ED � Just like Toxicology… � Palliative Care consultant will see the patient upstairs � Incorporate palliative care principles into daily practice � Referred by ED � Dedicated hospital palliative care team or inpatient palliative care unit NOT REQUIRED � Referred by Hospitalist � We are doing “Palliative Care” every day � No Palliative Care consultant: Emergency Physician responsible for trajectory of care in the hospital. � Non-curative symptom management � Thinking about trajectories � Delivering bad news � Emergency Physician required to trigger all of these 5
11/4/2013 Palliative Care in the E.D.: We are missing Patients who need: Models of palliative care � Improved communication skills around goals Hospice Old Life prolonging care Benefit of care � More attention on assessment/ Disease progression documentation of pain and other symptoms Life prolonging New Hospice Care � Emphasis on symptom interventions with care Palliative care improved EOL outcomes Diagnosis of serious illness Death Palliative Care is like Hypertension… Who Do We Screen? � Routine Follow-up: Do they have a serious or incurable � Serious or life-threatening illness and one or more: illness? � Not Surprised � Printed information � If the patient died in next 12 months � Bounce-Back � Referral for services � More than one ED visit or admit for same condition in last few months � Urgency (Would you be surprised if they died in the next 6 months?) � Uncontrolled Symptoms � ED visit prompted by difficulty to control physical or psychological � Follow up in one week symptoms � Functional Decline � Emergency (Would you be surprised if they died during this admission?) � Decline in function, feeding, weight loss, or caregiver distress � Increasingly Complicated � Rapid palliative care assessment � Long-term care needs requiring more resources or support � ED based palliative care/hospice consult 6
11/4/2013 Who to Include: Hospice Eligible Who to include: (>50% chance dying in next 6 months) � The less obvious but obvious � Progressive disease � increased symptoms, worsening lab values or functional � Dialysis Patients status and/or evidence of metastatic disease, particularly � Nearly 25% per year brain � Mortality for a 40 year old � Weight loss >5% in last 3 months � (8.4 vs. 37 years) � Karnofsky Performance Scale or PPS< 70% � COPD (Third leading cause of death in US) � CHF (NYH Class 4 – 1 yr mortality=50-66%) Palliative performance scale Hospice Percent Ambulatio Activity Self-Care Intake LOC Estimated � Hospice has greatest patient/family Median Activity n Survival satisfaction: Process not a place (Days) 70 Reduced No job Full Normal Full 108-145 � Protocol driven medications, equipment, or support of physical, psychosocial and reduced 40 Mainly bed No job Occasional Normal Full or 18-41 spiritual needs. No hobbies Assistance or drowsy No reduced � Some departments can refer directly to housework 10 Bed bound No job Significant Mouth Drowsy 1-6 hospice No hobbies Assistance care /coma No only � Need a lot of support housework 7
11/4/2013 What if the Intervention Began EARLIER than the ICU? Goals of Care/Code Discussion Early Intervention Associated with Cost Savings *P<.001 **P<.01 ***P<.05 Morrison RS. Arch Intern Med 2008 Live Discharges Hospital Deaths � Who to include? Usual Palliative Usual Palliative Costs ∆ ∆ Care Care Care Care � Gestalt…you are better than you think Per Day $830 $666 $174* $1,484 $1,110 $374* Per Admission $11,140 $9,445 $1,696** $22,674 $17,765 $4,908** � We are really good at sick or not sick Laboratory $1,227 $803 $424* $2,765 $1,838 $926* ICU $7,096 $1,917 $5,178* $14,542 $7,929 $7,776* � The better you know the patient, the Pharmacy $2,190 $2,001 $190 $5,625 $4,081 $1,544*** worse you are at predicting prognosis Imaging $890 $949 ($58)*** $1,673 $1,540 $133 � (Too Optimistic) Died in ICU X X X 18% 4% 14%* ED palliative ? ? ? ? ? ? � Plan for the worst…hope for the best care consult 2011 Center to Advance Palliative Care 29 Assessment choice ABCD Assessment � Patient condition drives assessment � Advance care plan Triage/Bedside Assessment Serious/Terminal Illness � Make the patient feel Better � Caregivers to consider Unstable/Critical � Decision-making capacity (e.g. near arrest, Stable VS compromised) � Covers physical, psychosocial domains ‘ ABCD ’ Expanded ‘ NEST ’ � If patient stabilizes, move onto sub-acute assessment Focused Assessment Assessment 8
Recommend
More recommend