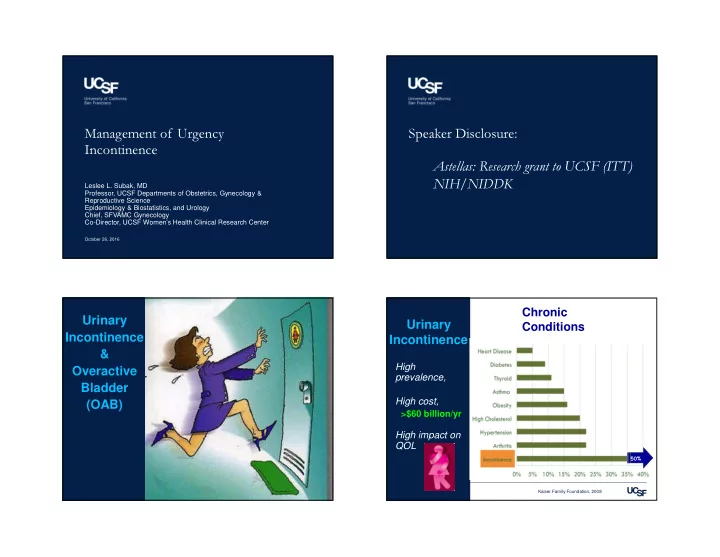
Management of Urgency Speaker Disclosure: Incontinence Astellas: Research grant to UCSF (ITT) Leslee L. Subak, MD NIH/NIDDK Professor, UCSF Departments of Obstetrics, Gynecology & Reproductive Science Epidemiology & Biostatistics, and Urology Chief, SFVAMC Gynecology Co-Director, UCSF Women’s Health Clinical Research Center October 26, 2016 Chronic Urinary Urinary Conditions Incontinence Incontinence & Overactive High prevalence, Bladder (OAB) High cost, >$60 billion/yr High impact on QOL 50% 50% Kaiser Family Foundation, 2008
UI: Who is at Risk? Urinary Incontinence Risk Factor � Risk � Common Age (per 5 years) 30% - 25% reproductive age women Live birth 30% - 40% postmenopausal women Modifiable or Preventable Oral estrogen 90% � Chronic Stroke 90% ‒ Social seclusion Diabetes 70% ‒ Falls & Fractures BMI (per 5 units) 60% ‒ 3x Nursing home admissions Poor overall health 60% ‒ Depression, anxiety, poor QOL Hysterectomy 40% COPD 40% Sampselle 2002; Jackson 2004; Hannestad 2003; Waetjen 2006; Melville 2005; Danforth 2006; Ebbesen 200; Wetle 1995; Brown 1996 Overactive Bladder (OAB) Stress vs. Urgency Incontinence Prevalence: 8-31% of women � Frequency: frequent urination Symptom Stress UI Urgency UI • >8x per day � Urgency: sudden compelling desire to void Precipitant Activity Urge • Difficult to defer Timing Immediate Delayed � Nocturia: need to wake during sleep to void Amount Small-mod Small-large • >2x per night Urinary Frequency Rare Common � Urgency urinary incontinence (UUI): involuntary leakage of urine usually associated with urgency Nocturia Rare Common Abrams P et al. Neuourol Urodyn. 2002;21:167
Don’t Tell : Patients Don’t Ask: PCC Practice Guidelines: •Few women seek care: 20-30% History, diary, pelvic exam, stress cough test, •Not discussed with other women post void residual (PVR), U/A, 24 hr pad test •Treatments: lack knowledge, fear of surgery •U.S. PCC reality check : • Failed communication with provider −15 minute appointments −no pelvic exam tables −PVR not possible Too cumbersome for US primary care Shaw 2001; Roe 1999; Seim 1995; Mitteness 1995; Burgio 1994 Diagnostic Aspects of Incontinence Study (DAISy) 3 Incontinence Questions (3IQ) •Multi-center study (N=301) 1. During the last 3 months, have you leaked urine, even a small amount? If yes: •3 Incontinence Questions (3 IQ) vs. 2. Does the leak happen with: Extended Evaluation • Physical activity, coughing, sneezing, lifting, or exercise − US, UK, WHO: Clinical Practice Guidelines (Stress UI) • Urge, feeling need to empty but could not get to the − Extensive History toilet fast enough (Urge UI) − Exam: Neuro S2-S4, Pelvic exam • Don’t know (Other UI) − Tests: PVR, Cough Stress Test, UA 3. Type of UI MOST OFTEN : − 3-Day Diary • Categorize as Stress, Urge, Mixed (=), Other Brown JS et al. Annals Internal Med 2006;144:715 Brown JS et al. Annals Internal Med 2006;144:715 12
3 Incontinence Questions (3 IQ) Accuracy of 3 IQ Compared to 1. During the last 3 months, have you leaked urine, even a small Extended Evaluation amount? � Yes No � Questionnaire Completed. � Sensi- Speci- 2. During the last 3 months, did you leak urine: ( Check ALL that apply. ) PPV LR+ � When you were performing some physical activity such as coughing, tivity ficity sneezing, lifting or exercise? � When you had the urge or the feeling that you needed to empty your Urgency bladder but you could not get to the toilet fast enough? 0.75 0.77 0.79 3.26 UI � Without physical activity and without a sense of urgency? 3. During the last 3 months, did you leak urine most often: (Check only ONE) Stress UI 0.86 0.60 0.74 2.13 � When you were performing some physical activity such as coughing, sneezing, lifting or exercise? [ STRESS ] � When you had the urge or the feeling that you needed to empty your bladder but you could not get to the toilet fast enough? [ URGENCY ] > Similar to other diagnostic tests � Without physical activity and without a sense of urgency? [ OTHER ] � About equally as often with physical activity as with a sense of urgency? [ MIXED ] Brown JS et al. Annals Internal Med 2006;144:715 Patient Resources VALIDATION OF 3IQ National Association For Continence •3IQ: simple, inexpensive, feasible •www.nafc.org − Reproducible (kappa 70% for urge and stress) •Diagnostic quiz − Acceptable accuracy for classification of incontinence type •Disease state and treatment information •Include a urinalysis (UA) in the evaluation •FAQs, Q&A forum •Take Home Message •1-800-BLADDER − 3IQ is a good test for type of UI in women NIDDK − With 3IQ + UA, the risk of missed Dx and Rx is low � http://kidney.niddk.nih.gov/kudiseases/pubs/uiwomen/ Brown JS et al. Annals Internal Med 2006;144:715
Urinary Diary UI: Modifiable Contributing Factors � UTI � Simple form for recording voids, incontinent episodes, fluid intake � Constipation � Excellent education & intervention! � Obesity • � UI episodes by 25-45% � Diabetes � Very useful in planning therapy � Mobility impairment • fluid adjustment � Liquids, caffeine, EtOH • timing and type of medications � Drugs: diuretics, ACE inhibitors, sedatives, hypnotics Behavioral Treatment for UI Lifestyle changes 1. Fluids management 2. Avoid Caffeine, carbonated beverages, alcohol 3. Bedside commode, night light 4. Weight loss, diabetes control
Behavioral Treatment for UI Weight Reduction & UI 5. Pelvic Floor Exercises Program to Reduce Incontinence by Diet & - Squeeze your bottom like you are trying to hold back Exercise (PRIDE) gas (should feel around your vagina as well) • NIDDK-funded multi-site RCT - Hold for 2 seconds and relax for 2 seconds (increase • 338 obese women with UI each by 1 second each week until 10 seconds each) • 6-month lifestyle intervention vs. control 6. Timed voiding / bladder retraining 7. Bladder control strategies Intervention Control P-Value - Urge control: “Freeze and Squeeze” Weight -8.2% -1.8% <0.001 - Stress control: “Squeeze before you Sneeze” (lift, etc.) Total UI -46% -25% 0.04 Verbal and written instructions Weight Loss similar to medications for UI Burgio KL. 2002; Goode PS. 2003; Dumoulin C 2010; Fantyl 1991 Subak LL et al. N Engl J Med. 2009;360:481-90 Patient Information vs. Behavioral Rx Meta-analysis: PFMT vs. no Rx •222 women with Urge UI: RCT � 12 RCT’s with 672 women • moderate to high risk of bias Improvement • variation in interventions used, study •Self-help booklet 59% populations, and outcome measures •Verbal/vaginal instruct 69% � � report of cure or improvement with PFMT •Biofeeback 63% • better continence specific quality of life • less leakage on office pad test. Not statistically different • longer training period α greater benefit Bottom line: Educate & Empower! Dumoulin C, Hay-Smith J. Cochrane Database Syst Rev 2010 Burgio KL. JAMA. 2002;288:2293
Medication 25 Holroyd-Leduc JM et al. JAMA 2004;291:986-95 26 OAB Medications OAB Medications Anticholinergic/Antimuscarinic mechanism � Relax the bladder Adverse effects: dry mouth/eyes � Symptom relief constipation, urinary retention confusion, anxiety, somnolence � Patient-Directed headache, dizziness Balance: nausea, dyspepsia tachycardia, palpitations Contraindications: narrow angle glaucoma hepatic/renal disease Holroyd-Leduc JM et al. JAMA 2004;291:986-95
Pharmacologic Therapies Indicated for Cochrane Review: OAB with or without UUI OAB Drug Effectiveness 61 RCTs; 12,000 adults; 9 meds � Medication vs. placebo RR (95% CI) • Cure or improvement 1.39 (1.28, 1.51) • UI episodes/dy 0.54 (0.41, 0.67) • Voids/dy 0.69 (0.54, 0.84) • Improved QOL • � Dry mouth 3.00 (2.70, 3.34) • No increase in withdrawal Mirabegron (Myrbetriq, Astellas Pharmaceuticals) 25, 50 mg by mouth once daily Nabi G et al. Cochrane Database Syst Rev 2006 Nygaard I. N Engl J Med 2010;363:1156-1162 Mirabegron (Myrbetriq) Meta-analyses: Antimuscarinic Efficacy: � Mirabegron: selective β 3-adrenoceptor agonist � Placebo controlled trials � Systematic review and meta-analysis • ~ all meds better than placebo • Randomized double-blind, placebo-controlled trials • UI episodes, urgency, voids, volume voided • Four publications, N=5,761 patients � A ctive comparator trials Variable (per 24 hours) Std Mean Difference • UI episodes : oxybutynin ER 10mg > tolterodine ER 4mg • Urgency: solifenacin 5-10 mg > tolterodine IR 4 mg UI Episodes -0.4 (-0.6, -0.3) • Void frequency: solifenacin 10 mg > tolterodine IR 4 mg Voids -0.6 (-0.8, -0.4) Volume voided 13 ( 10, 16) Quality of Life • ~ all meds greater improvements in QOL than placebo Urgency episodes -0.6 (-0.8, -0.4) Nocturia -0.1 (-0.2, -0.01) Most common AE = dry mouth • No increased risk: htn, arrythmia, retention, • � incidence and severity vs. placebo discontinuation 2 o AE • � incidence and severity oxybutynin IR Nabi G et al. Cochrane Database Syst Rev 2006; Chapple et al. Eur Urol 2005 Cui Y . Int J Nephrol. 2013
Recommend
More recommend