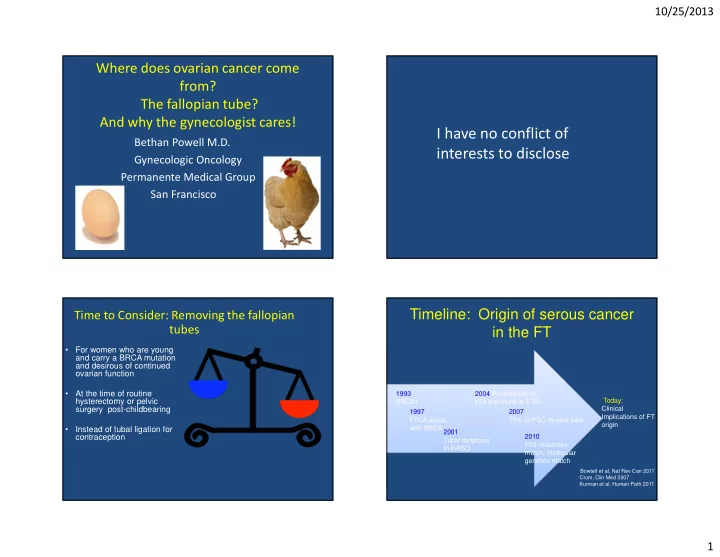
10/25/2013 Where does ovarian cancer come from? The fallopian tube? And why the gynecologist cares! I have no conflict of Bethan Powell M.D. interests to disclose Gynecologic Oncology Permanente Medical Group San Francisco Timeline: Origin of serous cancer Time to Consider: Removing the fallopian tubes in the FT • For women who are young and carry a BRCA mutation and desirous of continued ovarian function • At the time of routine 1993 2004 Progression of hysterectomy or pelvic Today: BRCA1 p53 signature to STIC surgery post-childbearing Clinical 1997 2007 Implications of FT FTCA assoc 70% of PSC involve tube origin with BRCA 2001 • Instead of tubal ligation for contraception 2010 Tubal dysplasia P53 mutations In RRSO match, molecular genetics match Bowtell et al, Nat Rev Can 2011 Crum, Clin Med 2007 Kurman et al, Human Path 2011 1
10/25/2013 Classic thinking…. Serous Pelvic Cancer: Old school Germ Cell Sex Cord-Stromal (3%-5%) (2%-3%) Ovarian peritoneal Fallopian tube Secondary (Metastatic) (5%) Figure modified from Gartner, L.P. & Hiatt, J.L. eds. In Color Atlas of Histology . 3rd ed. (2000) Lippincott Williams & Wilkins: Philadelphia, PA. 2
10/25/2013 Ovarian Cancer Risk Reduction in Early Stage Ovarian Cancer average risk women and mutation carriers • OCPs – 50% reduction in ovarian cancer risk • BTL – up to 40% reduction in ovarian cancer risk • Hysterectomy- 36% reduction in ovarian cancer risk for 15 years. • Increased risk with PID Microsectioning the tubes and ovaries Risk Reducing salpingo-oophorectomy for BRCA mutation carriers . 80- 90 % effective in reducing ovarian cancer 50% reduction in breast cancer if performed before age 50 Increase life expectancy 6.6-11.7 years for combined BSO, mastectomy ������������������������������������ 3
10/25/2013 Pathology Review of 163 RRSO Sectioning of RRSO Specimens Cases from UCSF Age Surgical specimen pathology Staging surgery Adjuvant treatment Outcome 1 44 OSC, 0.1cm Benign None Recurrent peritoneal CA @ 19mo. 2 44 Bilateral OSC, 1.3cm & Staged at RRSO, Taxol/Carboplatin x6 NED @ 47mo. 0.5cm Stage IIIC ovarian CA TSC, 0.6cm 3 67 STIC Stage IIC tubal CA, washings (+) Taxol/Carboplatin x6 NED @ 7mo. 4 52 TSC, 0.23cm Stage IC tubal CA, washings (+) Taxol/Carboplatin x6 NED @ 90mo. 5 52 STIC, 0.15cm Benign None NED @ 66mo. 6 49 OSC, 0.09cm Not performed None Recurrent peritoneal CA @ 81mo. 7 52 STIC, 1.1cm Stage IA tubal CA, washing (-) Taxotere/Carboplatin x6 NED @ 132mo. 8 59 OSC, 0.3cm Benign None NED @ 78mo. STIC, 0.3cm 9 50 STIC, 0.1cm Not performed None NED @ 66mo. 10 43 STIC, 0.2cm Not performed None NED @ 49mo. 11 61 STIC, 0.1cm Not performed None NED @ 6mo. OSC = ovarian serous carcinoma TSC = tubal serous carcinoma STIC = serous tubal in situ carcinoma or non-invasive tubal serous carcinoma RRSO summary of literature 14 RRSO series: 95 of 132 occult cancers (71%) originated in the fallopian tube. Reitma et al, Euro J Cancer, 2013 Leeper et al, Gynecol Oncol 2002 Mingels et al, Gyn Onc, 2012 Olivier et al, Br J Cancer 2004 Powell et all, Int J Gyn Onc 2011 Callahan et al, J Clin Oncol Manchanda et al, BJOG, 2011 Hermsen et al Int J Cancer 2006 Carcangiu et al, am J Surg Pathol 2006 Laki et al, Cancer 2007 Colgan et al Am J Surg Path 2001 Lamb et al, Am J obstet Gynecol 2006 Finch et al, Gynecol Oncol 2006 Lu et al, J Clin Oncol 2000 Carcangiu et al, am J Surg Pathol 2006 4
10/25/2013 STIC and cancer in proximity Stepwise Progression: Precursor Lesions Levanon JCO 2008, Lee et al Evidence compelling that HGPSC Tubal intraepithelial carcinoma originates in the fallopian tube TP53 Ki67 • Consistent with epidemiology TIC • Precursor lesion in tube • Mullerian molecular markers: PAX8, not calretinin • Molecular markers match, P53 mutation in >80% • STIC or tube involved in 70% of PSC in sporadic and BRCA related cancer. HGSC • Mouse model Köbel et al. Expert Rev Mol Med. 2008 Aug 1;10:e22 5
10/25/2013 New Model of Serous Carcinogenesis Serous Pelvic Cancer Fallopian tube peritoneal ovarian Crum CMR 2007, Levanon, J Clin Onc 2008, Crum CMR 2007, Vercellini: Incessant menstruation NCCN Guidelines for BRCA mutation Salphingectomy in women with BRCA carriers: Removal of tubes and mutations ovaries • After children or age 35-40 Hot flashes If a young woman is not • Uptake of RRSO: 60-70% ready for menapause Sexuality • Median age of RRSO = 44-51 What about removing the Menopause • Cardiovascular mortality increased tube first and removing for age 40-45 the ovaries at a later Osteoporosis CV disease time? • Many of these women will not be eligible for estrogen Cognitive impairment 6
10/25/2013 At Age 30, Risk of Ov Cancer Salpingectomy in mutation carriers AGE BRCA1 BRCA2 Pros Cons • Some cancer risk reduction • Two stages to surgery 40 2.2% <1% • Avoid premature • Delay of removing the menapause ovaries • Maintain option for IVF • May not be as effective 50 8.7% 1.9% pregnancy • No Breast cancer risk • Option for those reduction 60 22% 7.4% unwilling to have BSO Chen et al, JCO 2007 Oophorectomy reduces Cost Effectiveness Model Breast Cancer Risk • BRCA1 Average Avg Life Avg QALY Incremental Discounted Costs Expectancy Expectancy C-E Ratio (cost per (Can $) Gain Gain QALY) – < 40: OR 0.36, CI 0.20-0.64 BRCA1 – 41-50: OR 0.50, CI 0.27-0.92 BSO @ 40 $25,987 21.15 17.56 --- Tubes @ 40 $38,208 20.74 18.17 $20,050 – >50: OR 0.66, CI 0.21-2.09 Tubes @ 40, $41,577 20.83 18.26 $37,805 Ov @ 50 • BRCA2 BRCA2 – <40: OR 0.69, CI 0.25-1.95 BSO @40 $16,932 22.62 18.87 --- Tubes @ 40 $33,150 22.08 19.51 $25,658 – 41-50: OR 0.44, CI 0.15-1.24 Tubes @ 40, $37,686 22.14 19.56 $89,680 Ov @ 50 – >50: OR 1.00, CI 0.06-16.1 Delayed oophorectomy with the greatest QALY Eisen et al, J Clin Oncol, 2005 Kwon et al, Obstet Gynecol 2013 7
10/25/2013 When to consider removing Why leave the tube in women at the fallopian tube in average risk average risk? women? In US 30% women undergo hysterectomy, 50% have ovaries and fallopian tube left in situ Remove FT even if preserving ovaries at ~20% of women who develop ovarian cancer have time of hysterectomy had a prior hysterectomy Up to 20% of ovarian cancer patients have had a Consider in place of tubal ligation tubal ligation 24% of ovarian cancer patients have germ-line mutations Perform salpingectomy Walsh et al, PNAS 2011 with pelvic surgery Davis et al, J La Soc 2003 Salpingectomy Instead of tubal ligation Removal of the tube at hysterectomy or at time of any pelvic surgery Pros Cons • No detrimental effect on: • Decreased tubal pathology, • Requires surgery ovarian function • Decreased ectopic rate • May be difficult to access hormonal levels tube • Improved sterilization efficacy • Potential for bleeding blood supply to the ovary • Potential cancer risk • May require additional • If tube is left in situ, incidence of hydrosalpinx: 28%, reduction equipment/incision/cost requiring surgery 7.8% • Uncommon cancer Dar et al, 2000 Sezik et al, 2007Ghezzi et al, 2009, Morse et al, 2006 8
10/25/2013 Technique Removal of tube vs tube and ovary BRCA 1 or 2 mutation No known genetic risk • Preserve the utero-ovarian • Inspect entire abdomen tubes ligament • Peritoneal cytology • Remove or cauterize any uterus • Remove adjacent ovarian attachments to the ovary capsule (fimbria ovarica) • If the entire fallopian tube ovaries • Remove all the tube cannot be removed, consider removing the tubal • Place in an endoscopic bag fimbrial end • Pathology: microsectioning • Pathology: examine the 2 cm IP entire tubes fimbrae in 2-3 cassettes. 9
10/25/2013 Time to Consider: Removing the Caution: Limited data on impact of fallopian tubes Salpingectomy • For women who are young • Standard of care is risk and carry a BRCA mutation reducing salpingo- and desirous of continued • In average risk women: none oophorectomy ovarian function • In BRCA mutation carriers: Greene et al, Editorial (Am J Ob/Gyn 2011) • Use judgement in vaginal • At the time of routine Dietl et al, Opinion (Hum Reprod 2011) hysterectomy or pelvic surgery hysterectomy, poor access, post-childbearing low visibility, high risk. LeBlanc et al, feasibility of “radical fimbrectomy” (Gynecol Oncol 2011) Kwon et al, Markov model (ObGyn 2013) • In office procedures are lower • Instead of tubal ligation for contraception cost. Holman et al, FORCE survey (SGO 2013) Use judgement in PPTL, at Clinical trial currently enrolling/proposed ceasarian section. 10
Recommend
More recommend