Historical Perspective - Federal • Custodial Care model – “ Death of the Asylum ” – 1950’s experimentation with novel aftercare programs (1400 state clinics) • Birth of the Federal Mental Health System: 1960-63 • De-institutionalization – Kennedy’s goal decrease census 50% in a decade 1956 – 558,239 beds (1294 state funded outpt clinics) – 340 beds/100K 1963-67 – decreased census 19,000/year 1969 – 399,152 ( 122 CMHC’s) (7% SOF discharges) 1976 – 170,619 (548 CMHC’s) (3.6% SOF discharges) 2010 – 35,000 beds – 11 beds/100K • CMHC’s 1966-79 – 789 centers ($2.7B ) 20 years Catchment areas – 75-200K 5 essential services: inpt beds, PHP beds, 24 hr crisis, outpt, C/L education • 1969 – IMD Exclusion in Medicaid 2
Historical – Indiana • 1960 – 6000 beds in 13 SOF’s ( 130 beds/100K) • 2010 – 880 licensed beds in 6 SOF’s (13 beds/100K) – $160M ($200,000/bed) – ALOS exceeds 2 years • 25 CMHC’s – Gatekeeper (1970’s) • Deinstitutionalization has become “ Transinstitutionalization ” – IDOC – 30,000 inmates (40% Axis I / 80% have SUD) – Police have become Crisis Mental Health workers – Municipal/County jails – detox/stabilize – ER’s – ECF’s – Homeless 3
Department of Corrections = New State Psychiatric System • Indiana: • 1970 = 5% prison population with SMI • 1980 = 10% • 1990 = 15% • 2012 = 40% 2006 Department of Justice study 24% County inmates have psychosis 26 days vs 51 days 41% of behavioral infractions 80% assaults on deputies $130/d vs $80/d for non-mentally ill 4
The mental health provider community and advocacy organizations have made it clear - INDIANA NEEDS A NEW MODEL OF PUBLIC MENTAL HEALTH CARE 5
Transformation of Public Mental Health in Indiana (FSSA Playbook) • Recognize the states role and responsibility in funding care and services – HIP 2.0 (370,00 enrolled in first year) – MC rates + legacy increases – Embrace MH/SUD Parity – expand services • No longer defer to the NIMH or CMS for direction • Reorganize our SOF’s as a system – “One Hospital System with 6 campuses” – Systems Integration Council – September 2014 • Modernize our public assets for the future of healthcare – NDI as hub – focus on Neurodiagnostics – Leveraging technology – Video Presence + Telepsychiatry – New model of care – rapid through-put, shorter LOS • Re-establish public continuum of mental health care – Hospital Systems + Private practices – Free-standing Psychiatric facilities – CMHC’s – SOF’s • Submit Federal waivers (1115) – increase Medicaid covered services – lift IMD Exclusion • Address Mental Health manpower needs 6
“New Model” • Focus on getting the Diagnosis Right – September Institute of Medicine Report (10% deaths) – Neurodiagnosticsand Genetic Testing + structured tools/interviews • Full Medical Integration – No longer remote - tertiary and specialty medical care – Attached to large ED • State-wide Center of Excellence – Tele-management – ECHO model of consultative care in home community • No longer require “Gatekeeping” – Eliminate/lessen need for commitments – Referrals from Health Systems • Rapid Through-put – ALOS 30 – 45 days – Build network of step-downs • Dedicated SNF units for medically ill • ECF for cognitive challenged • Residential • Home community-based programming 7
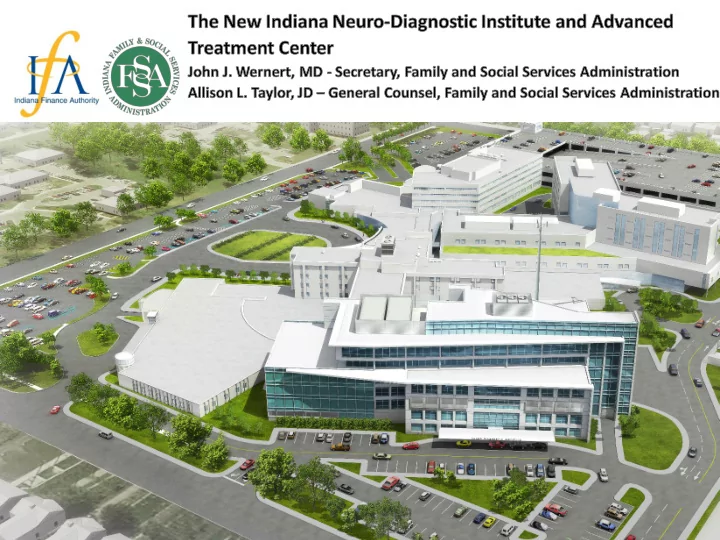
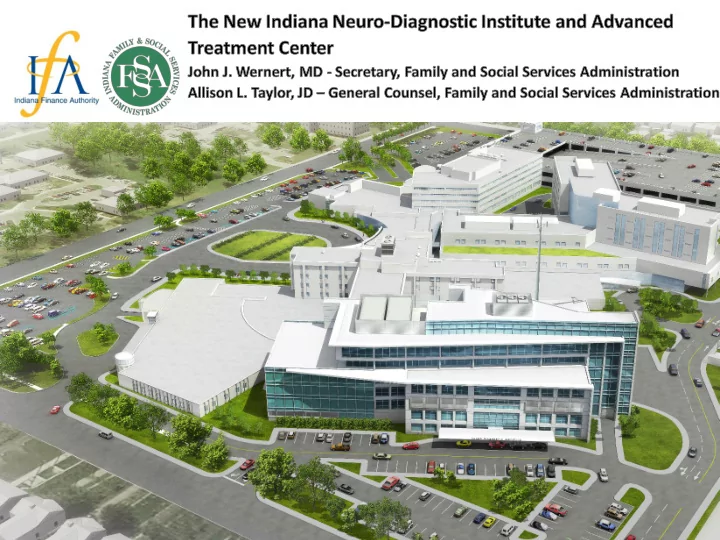
About NDI • New facility to replace LaRue D. Carter Memorial Hospital, titled the Neuro-Diagnostic Institute and Advanced Treatment Center (“NDI”) • Designed as a state-of-the-art facility to provide a modern model of advanced diagnosis and assertive mental health care in Indiana • First State Facility built in a generation 8
Business Case Patient • More than 100k adolescent and 260k adult Indiana residents are eligible for services. • There has been a steady decline of available mental health beds since Need 1950’s (6,000+ beds in 1950s vs. 800 today). Physical • Due to its age and historical register designation, LaRue D. Carter Memorial Hospital’s infrastructure is deteriorating and requires significant maintenance investment. Need • The physical layout of LaRue Carter is not conducive to anticipated treatment protocols (originally designed as a non-ambulatory hospital). Operational • Integrated patient care requires co-location with an acute care medical facility. • The 6 state owned facilities currently operate independently, without a Need central “hub”. 9
About Our Location and “Partner” • Partnership with Community Health Network , co-located on the campus of Community East Hospital in Indianapolis (co- located model addresses the need for access to a primary care facility) • Immediate and proximal acute medical intervention availability for NDI patients • Synergy of Community East’s campus redevelopment and Community Health Network’s exhibited commitment to mental health in Indiana 10
Patient Impact The NDI will substantially increase the number of patients treated & reduce the average length of stay (LOS). Better through- put modeling… Historical Budget Projected LaRue Carter Transition New Institute FY 2012 FY 2013 FY 2014 FY 2015 FY 2016 FY 2017 FY 2018 FY 2019 FY 2020 FY 2021 Patients Served 235 229 187 181 181 159 141 917 1,381 1,517 Average LOS 208.29 208.29 247.48 248.45 248.45 244.41 240.26 46.59 36.86 35.84 Patient Days 49,044 47,699 46,278 44,970 44,970 38,861 33,973 42,736 50,890 54,378 1,600 60,000 1,400 50,000 1,200 40,000 1,000 800 30,000 600 20,000 400 10,000 200 - - FY 2012 FY 2013 FY 2014 FY 2015 FY 2016 FY 2017 FY 2018 FY 2019 FY 2020 FY 2021 LaRue Carter Transition New Institute Patients Served Average LOS Patient Days 11
Positive Financial Impacts • Increased efficiencies and patient throughput will increase both access to services and quality of care without increasing overall costs and while driving down the impact to the State per patient day • Modern design reduces maintenance and operational costs • Potential for shared services and bulk collaborative buying influence serving full campus demand • Reduced and/or eliminated medical intervention transport and personnel costs from stand-alone Carter hospital • “Blank slate” opportunity to research best practices, outcomes based treatment decisions, and methods to reduce systemic costs State-wide 12
Impact per Patient Day The NDI will create relief from the impending rise in daily treatment cost to the State of Indiana to treat patients with mental health disease. One of the projections utilized to display the fiscal goals of our new SOF below: State Impact per Patient Day $800.00 $697.52 $700.00 $630.68 $602.23 $593.81 $543.91 $600.00 $479.17 $451.44 $459.99 $500.00 $445.78 $418.34 $508.40 $400.00 $414.20 $388.05 $300.00 $200.00 $100.00 $- FY 2012 FY 2013 FY 2014 FY 2015 2016 FY 2017 FY 2018 FY 2019 FY 2020 FY 2021 Budget LaRue Carter Transition New Institute LaRue Carter LaRue Projection Forecasted NDI 13
NDI Construction Cost, Financing Plan, High Level Timeline • Construction Budget Type Investment Soft Costs $16,100,000 Hard Costs $102,663,863 Grand Total $118,763,863 • Financing Plan $119M long-term bond issuance • 20-year bonds beginning July 2019 through FY 2039 • Appropriations limited to no more than $10.9M per year (annual debt service payment under this annually) • Timeline Pre-Design Due Design/ Construction Build/ Design/Engineering Diligence Bid Occupy Q3 2015 – Q3 2016 – Q2 2017 – Q2 2016 Q1 2017 Q4 2018 14
Patient Programs / Units – 159 beds total • Adolescent Unit (30 beds) – ages 13 – 17. (Early Onset Schizophrenia) • Child Unit (12 beds) – ages 6 – 12. (ASD) • Adult Severe Mental Illness (15 beds) • Forensic Unit (24 beds) • Research Unit (12 beds) • Assessment and Diagnostic Unit (15 beds) • Acute Adult Unit (15 beds) • ID/DD Dual Diagnosis Unit (12 beds) • SUD + SMI Dual Diagnosis Unit (12 beds) • Stabilization Unit (12 beds) 15
Legal Nuts and Bolts of NDI Project • Feasibility Phase • Pre-Development Phase - Imminent – Pre-development services agreement and license agreement – Pre-development vendor agreements (architects, engineers, construction manager) – Zoning approvals – Real estate documents for NDI Tower and Connector – Use and Occupancy – Connector Rights – Professional Services – Support Services Financing Documents • Construction and Development Phase • Operational Phase • + Legislative packages in 2017 and 2018 16
Q & A For more information, including architectural renderings of the proposed facility, please visit the FSSA website by following the link below: http://www.in.gov/fssa/dmha/2935.htm 17
Recommend
More recommend