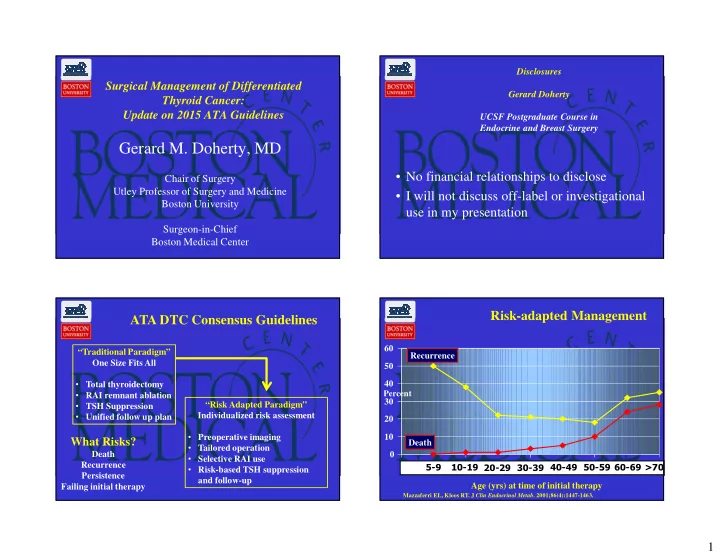
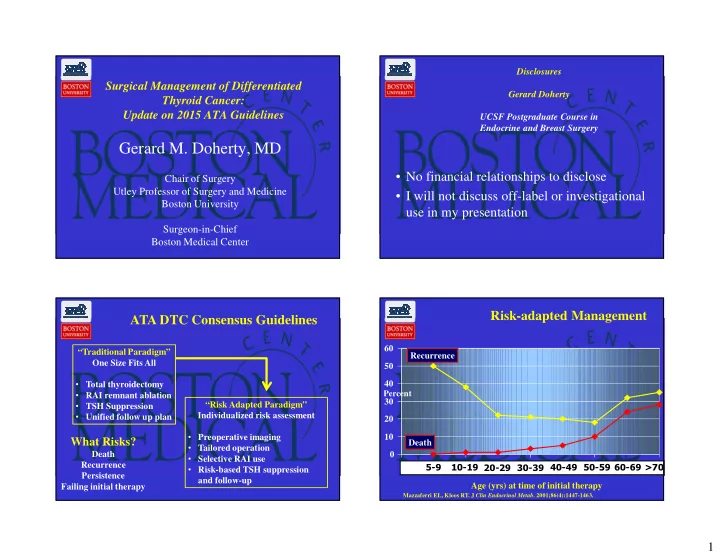
Disclosures Surgical Management of Differentiated Gerard Doherty Thyroid Cancer: Update on 2015 ATA Guidelines UCSF Postgraduate Course in Endocrine and Breast Surgery Gerard M. Doherty, MD • No financial relationships to disclose Chair of Surgery Utley Professor of Surgery and Medicine • I will not discuss off-label or investigational Boston University use in my presentation Surgeon-in-Chief Boston Medical Center Risk-adapted Management ATA DTC Consensus Guidelines 60 “Traditional Paradigm” Recurrence One Size Fits All 50 • Total thyroidectomy 40 Percent • RAI remnant ablation 30 “Risk Adapted Paradigm” • TSH Suppression Individualized risk assessment • Unified follow up plan 20 • Preoperative imaging 10 What Risks? Death • Tailored operation Death 0 • Selective RAI use Recurrence • Risk-based TSH suppression 5-9 10-19 20-29 30-39 40-49 50-59 60-69 >70 0 2 4 6 Persistence and follow-up Age (yrs) at time of initial therapy Failing initial therapy Mazzaferri EL, Kloos RT. J Clin Endocrinol Metab . 2001;86(4):1447-1463. 1
Risk of Structural Disease Recurrence Risk-adapted Management (In patients without structurally identifiable disease after initial therapy) FTC, extensive vascular invasion ( ≈ 30-55%) ATA Update - Estimating Risk of Recurrence pT4a gross ETE ( ≈ 30-40%) rmt1 pN1 with extranodal extension, >3 LN involved ( ≈ 40%) High Risk Intermediate Risk Gross extrathyroidal extension, PTC, > 1 cm, TERT mutated ± BRAF mutated* (>40%) incomplete tumor resection, distant metastases, Low Risk pN1, any LN > 3 cm ( ≈ 30%) or lymph node >3 cm • Microscopic ETE PTC, extrathyroidal, BRAF mutated*( ≈ 10-40%) • Classic PTC PTC, vascular invasion ( ≈ 15-30%) • Gross node mets or >5 micromets Intermediate Risk Clinical N1 ( ≈ 20%) Aggressive histology , minor extrathyroidal • No local or distant mets • Aggressive Histology extension, vascular invasion, pN1, > 5 LN involved ( ≈ 20%) or > 5 involved lymph nodes (0.2-3 cm) • N0 or <5 node micromets • Vascular invasion Intrathyroidal PTC, < 4 cm, BRAF mutated* ( ≈ 10%) • Complete resection pT3 minor ETE ( ≈ 3-8%) Low Risk pN1, all LN < 0.2 cm ( ≈ 5%) Intrathyroidal DTC • No tumor invasion High Risk ≤ 5 LN micrometastases (< 0.2 cm) pN1, ≤ 5 LN involved ( ≈ 5%) • No vascular invasion Intrathyroidal PTC, 2-4 cm ( ≈ 5%) • Macroscopic gross ETE • If given, no RAI uptake Multifocal PMC ( ≈ 4-6%) • Incomplete tumor resection pN1 with extranodal extension, ≤ 3 LN involved (2%) outside thyroid bed Minimally invasive FTC ( ≈ 2-3%) • Node met > 3 cm Intrathyroidal, < 4 cm, BRAF wild type* ( ≈ 1-2%) • Distant Mets Intrathyroidal unifocal PMC, BRAF mutated*, ( ≈ 1-2%) • Inappropriate Tg elevation Intrathyroidal, encapsulated, FV-PTC ( ≈ 1-2%) Unifocal PMC ( ≈ 1-2%) Initial Surgery Initial Surgery C) If surgery is chosen for patients with • A) For patients with thyroid cancer >4 cm, or with gross extrathyroidal extension (clinical • A) For patients with thyroid cancer >4 cm, or with gross extrathyroidal extension (clinical T4), or clinically apparent metastatic disease to nodes (clinical N1) or distant sites (clinical thyroid cancer <1 cm without T4), or clinically apparent metastatic disease to nodes (clinical N1) or distant sites (clinical M1), the initial surgical procedure should include a near-total or total thyroidectomy and M1), the initial surgical procedure should include a near-total or total thyroidectomy and gross removal of all primary tumor unless there are contraindications to this procedure. gross removal of all primary tumor unless there are contraindications to this procedure. extrathyroidal extension and cN0, the (Strong Recommendation, Moderate-quality evidence) (Strong Recommendation, Moderate-quality evidence) initial surgical procedure should be a • B) For patients with thyroid cancer >1 cm and <4 cm without extrathyroidal extension, and • B) For patients with thyroid cancer >1 cm and <4 cm without extrathyroidal extension, and without clinical evidence of any lymph node metastases (cN0), the initial surgical thyroid lobectomy unless there are clear without clinical evidence of any lymph node metastases (cN0), the initial surgical procedure can be either a bilateral procedure (near-total or total thyroidectomy) or a procedure can be either a bilateral procedure (near-total or total thyroidectomy) or a unilateral procedure (lobectomy). Thyroid lobectomy alone may be sufficient initial indications to remove the contralateral unilateral procedure (lobectomy). Thyroid lobectomy alone may be sufficient initial treatment for low risk papillary and follicular carcinomas; however, the treatment team treatment for low risk papillary and follicular carcinomas; however, the treatment team may choose total thyroidectomy to enable RAI therapy or to enhance follow-up based may choose total thyroidectomy to enable RAI therapy or to enhance follow-up based lobe. upon disease features and/or patient preferences. (Strong Recommendation, Moderate- upon disease features and/or patient preferences. (Strong Recommendation, Moderate- quality evidence) quality evidence) • C) If surgery is chosen for patients with thyroid cancer <1 cm without extrathyroidal • C) If surgery is chosen for patients with thyroid cancer <1 cm without extrathyroidal extension and cN0, the initial surgical procedure should be a thyroid lobectomy unless extension and cN0, the initial surgical procedure should be a thyroid lobectomy unless there are clear indications to remove the contralateral lobe. Thyroid lobectomy alone is there are clear indications to remove the contralateral lobe. Thyroid lobectomy alone is sufficient treatment for small, unifocal, intrathyroidal carcinomas in the absence of prior sufficient treatment for small, unifocal, intrathyroidal carcinomas in the absence of prior head and neck irradiation, familial thyroid carcinoma, or clinically detectable cervical head and neck irradiation, familial thyroid carcinoma, or clinically detectable cervical nodal metastases. nodal metastases. 2
Slide 6 rmt1 This "approximately 40%" was previously "38%". so I made it approximately 40% to make it seem less precise tuttler, 4/13/2014
Recommend
More recommend