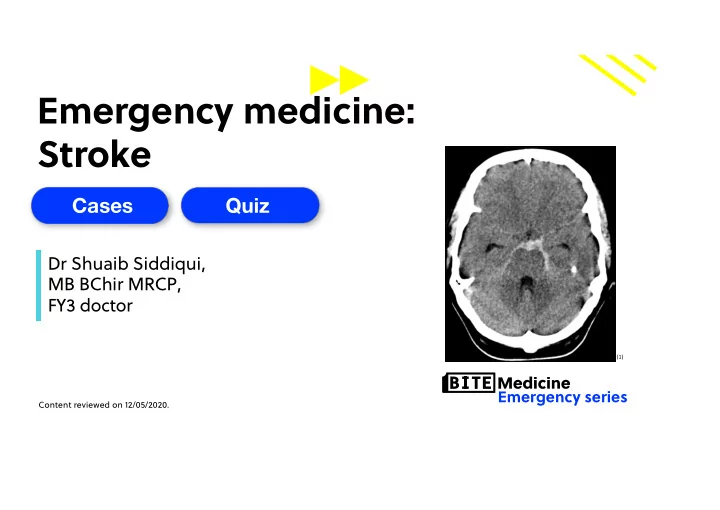
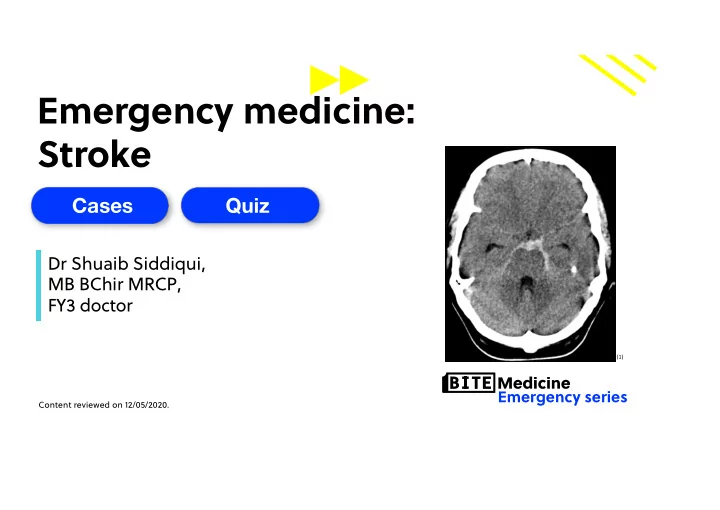
Emergency medicine: Stroke Cases Quiz Quiz Dr Shuaib Siddiqui, MB BChir MRCP, FY3 doctor (1) Emergency series Content reviewed on 12/05/2020.
Case 1 History You are working in A&E. You see a 70-year-old man who is brought in by ambulance after his son noticed he was slurring his speech. This started 3 hours ago. On examination, you note he has 3/5 power of both his left upper limb and 4/5 power of his left lower limb. Observations HR 90, BP 155/89 mmHg, RR 18, SpO2 97%, Temp 36.8 2
Question 1 3
Case 1 History You are working in A&E. You see a 70-year-old man who is brought in by ambulance after his son noticed he was slurring his speech. This started 3 hours ago. On examination, you note he has 3/5 power of both his left upper limb and 4/5 power of his left lower limb. Observations HR 90, BP 155/89 mmHg, RR 18, SpO2 97%, Temp 36.8 4
Question 2 5
Pathophysiology Definition: sudden onset of rapidly developing focal or global neurological disturbance which lasts more than 24 hours or leads to death (NICE) Pathophysiology Ischaemic (85%) Haemorrhagic (15%) Thrombotic Intracerebral • • Atherosclerosis Trauma • • Prothrombotic state HTN • Cerebral amyloid Embolic Subarachnoid • • AF Trauma • • Paradoxical embolus Berry aneurysm • • Infective endocarditis AVM Lacunar • HTN Hypoperfusion • Reduced blood pressure 6
Pathophysiology Definition: sudden onset of rapidly developing focal or global neurological disturbance Pathophysiology which lasts more than 24 hours or leads to death (NICE) Epidemiology • 11% of people die from a first stroke • Incidence of ~ 120,000 per year in the UK Risk factors • Age: risk doubles every decade after the age of 55 • Family history • Smoking • Diabetes • Hypercholesterolaemia • Carotid artery stenosis • Prothrombotic state 7
Stroke vs TIA Stroke TIA Pathophysiology Definition Sudden onset of rapidly developing Transient neurological symptoms focal or global neurological lasting less than 24 hours disturbance which lasts more than 24 hours or leads to death 8
Stroke vs TIA Stroke TIA Pathophysiology Definition Sudden onset of rapidly developing Transient episode of neurological focal or global neurological dysfunction caused by focal brain, disturbance which lasts more than spinal cord, or retinal ischaemia, 24 hours or leads to death without acute infarction Imaging Infarction No infarction Tissue Hypoxic damage No changes 9
Question 3 History You are working in A&E. You see a 70-year-old man who is brought in by ambulance after his son noticed he was slurring his speech. This started 3 hours ago. On examination, you note he has 3/5 power of both his left upper limb and 4/5 power of his left lower limb. Observations HR 90, BP 155/89 mmHg, RR 18, SpO2 97%, Temp 36.8 10
Question 4 History You are working in A&E. You see a 70-year-old man who is brought in by ambulance after his son noticed he was slurring his speech. This started 3 hours ago. On examination, you note he has 3/5 power of both his left upper limb and 4/5 power of his left lower limb. Observations HR 90, BP 155/89 mmHg, RR 18, SpO2 97%, Temp 36.8 11
Pathophysiology (2) 12
Pathophysiology (3) 13
Territory Signs Pathophysiology Anterior cerebral artery Contralateral hemiparesis and sensory loss • Lower limbs affected more than upper limbs Contralateral hemiparesis and sensory loss Middle cerebral artery • Upper limbs affected more than lower limbs Contralateral homonymous hemianopia Aphasia (dominant hemisphere) Hemispatial neglect (non-dominant hemisphere) 14
MCA infarct (4) 15
Hemispheric dominance Broca’s and Wernicke’s area: dominant hemisphere • Spatial processing: non-dominant hemisphere • (6) (5) 16
Hemispheric dominance Broca’s and Wernicke’s area: dominant hemisphere • Spatial processing: non-dominant hemisphere • (7) 17
Question 5 18
Territory Signs • Contralateral homonymous hemianopia with macular sparing Posterior cerebral Pathophysiology artery • Contralateral loss of pain and temperature due to thalamic infarction • Cerebellar signs - DANISH Vertebrobasilar artery • Reduced consciousness • Quadriplegia or hemiplegia 19
PCA infarct Pathophysiology (6) (8) 20
21
Vertebrobasilar infarct Pathophysiology (6) 22
ROSIER score Recognition of stroke in the emergency room • Score > 0 suggests possible stroke requiring further investigation • Feature Score Loss of consciousness or syncope - 1 point Seizure activity - 1 point New, acute onset: Asymmetric facial weakness + 1 point Asymmetric arm weakness + 1 point Asymmetric leg weakness + 1 point Speech disturbance + 1 point Visual field defect + 1 point 23
Investigations Bedside Blood glucose: rule out hypoglycaemia • ECG: assess for AF • Bloods U&Es: rule out hyponatraemia • Screen for risk factors: HbA1c, lipids, coagulation profile • Imaging Brain imaging: urgently within 1 hour • Non contrast CT head • CT angiogram • MRI head • CXR: if swallow compromised • Echocardiogram • Carotid doppler • 24
Question 6 History You are working in A&E. You see a 70-year-old man who is brought in by ambulance after his son noticed he was slurring his speech. This started 3 hours ago. On examination, you note he has 3/5 power of both his left upper limb and 4/5 power of his left lower limb. Observations HR 90, BP 155/89 mmHg, RR 18, SpO2 97%, Temp 36.8 25
Question 6 (9) 26
Management Thrombolysis: <4.5 hours of symptom onset • Alteplase • Must rule out intracranial haemorrhage prior to commencing • Aim for BP <180/110 Thrombectomy: <24 hours of symptom onset • Angiogram demonstrates proximal anterior or posterior circulation strokes • Limited infarct core on imaging Antiplatelets: all patients • Aspirin 300mg 2 weeks followed by clopidogrel 75mg lifelong • If the patient has had thrombolysis, commence antiplatelets on the following day Anticoagulation: only if the cause is AF • Commence Aspirin 300mg for 2 weeks • After 2 weeks, stop aspirin and consider anticoagulation 27
Management Absolute contraindication Relative contraindication Intracranial haemorrhage on CT Major surgery or serious non-head trauma in the previous 14 days Neurosurgery, head trauma or stroke in Recent lumbar puncture (usually in the past 3 months past 7 days ) History of intracranial haemorrhage History of major haemorrhage within the past 21 days Active internal bleeding Pregnancy Bleeding diathesis HTN >185 mmHg SBP or >110 mmHg DBP 28
Question 7 History You are working in A&E. You see a 70-year-old man who is brought in by ambulance after his son noticed he was slurring his speech. This started 3 hours ago. On examination, you note he has 3/5 power of both his left upper limb and 4/5 power of his left lower limb. Observations HR 90, BP 155/89 mmHg, RR 18, SpO2 97%, Temp 36.8 29
Management Risk factor modification • Smoking cessation • Statin: atorvastatin 80mg • Treat diabetes and HTN Driving • No driving for 1 month • HGV drivers must not drive for 1 year 30
Management 31
Management Haemorrhagic stroke • Admit to NCCU: consider need for intubation and hyperventilation • Control BP: aim for SBP 130-140mmHg (NICE) • IV hypertonic saline if evidence of raised ICP • Surgery 32
Management TIA • No need for CT imaging routinely • Do not use ABCD2 (NICE) • Commence on Aspirin 300mg • Review in TIA clinic within 24 hours if symptoms < 1 week ago, otherwise TIA clinic within 7 days • Echocardiogram • Carotid doppler • MRI brain • Lifelong clopidogrel 33
Complications Complication Pathophysiology DVT Aspiration pneumonia Neurological sequalae • Seizures • Weakness • Immobility • MCA syndrome Nutritional support 34
Question 8 (1) 35
Case 2 History A patient is brought in by ambulance. He is drowsy and was witnessed to have a tonic clonic seizure in the street. On examination you notice a significant right sided hemiparesis. He is struggling to maintain his airway but this improves upon a chin lift maneuver. 36
Top-decile question 37
Recap • Stroke results in neurological impairment with infarction Pathophysiology • TIA results in transient symptoms and is not associated with infarction • Urgent imaging must be performed within 1 hour • Thrombolysis should be commenced urgently if within 4.5 hours of symptom onset • Thrombectomy must be considered if presenting within 24 hours of symptom onset • Patients should be on aspirin 300mg for 2 weeks followed by lifelong clopidogrel 38
Further information We need your feedback and support! Release new lecture schedules every Saturday New, interactive website coming very soon Want to get involved? Contact us at opportunities@bitemedicine.com to get your information pack Stay up-to-date! • Website : www.bitemedicine.com • Facebook : https://www.facebook.com/biteemedicine • Instagram : @bitemedicine • Email : admin@bitemedicine.com 39
Recommend
More recommend