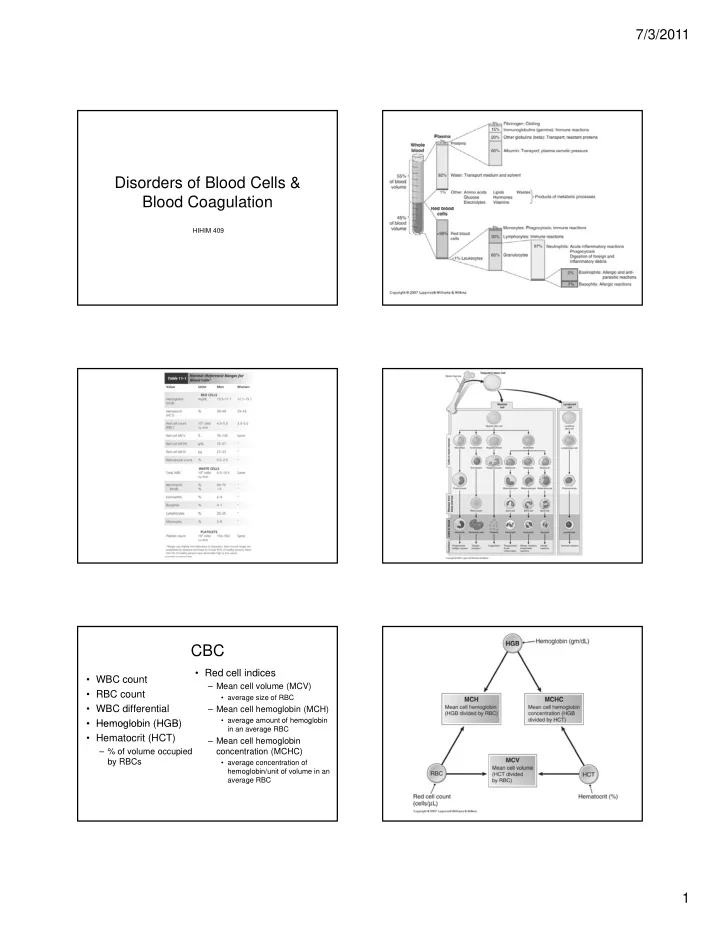
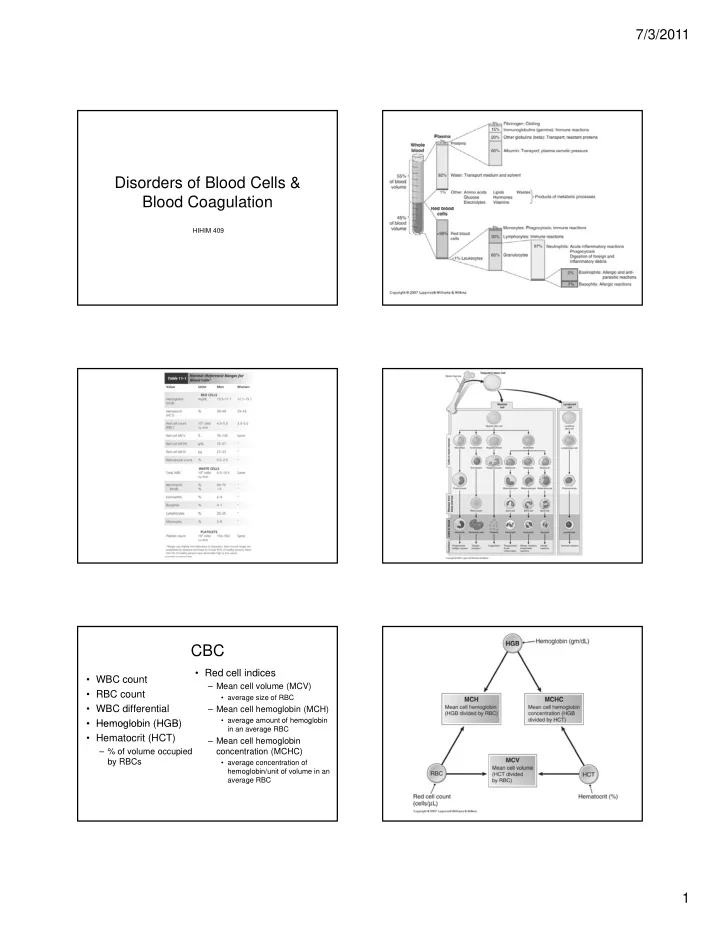
7/3/2011 Disorders of Blood Cells & Blood Coagulation g HIHIM 409 CBC • Red cell indices • WBC count – Mean cell volume (MCV) • RBC count • average size of RBC • WBC differential – Mean cell hemoglobin (MCH) • average amount of hemoglobin g g • Hemoglobin (HGB) • Hemoglobin (HGB) in an average RBC • Hematocrit (HCT) – Mean cell hemoglobin – % of volume occupied concentration (MCHC) by RBCs • average concentration of hemoglobin/unit of volume in an average RBC 1
7/3/2011 Major Determinants of Disease Anemia • Blood cells have a short life span & require continuous replacement • Abnormally low hemoglobin • Most diseases of blood cells feature too many or too few cells because of an imbalance in the production or loss of cells • Caused by • Hemoglobin must be properly assembled & produced for effective O 2 transport – decreased numbers of RBCs • White blood cells are critical in the defense against infection • • Diseases of lymphoid cells differ importantly from diseases of Diseases of lymphoid cells differ importantly from diseases of – decreased amount of hemoglobin d d t f h l bi myeloid cells • Malignancies of myeloid cells are associated with circulation of – both malignant cells in the blood (leukemia) • Malignancies of lymphoid cells are associated with malignant cells in • Sign of an underlying condition the blood (leukemia) or masses in lymph nodes & other tissue (lymphoma) • Diagnose • Most diseases that affect platelets cause a low platelet count – CBC Hemorrhage • Loss of O 2 carrying capacity • Loss of iron • Most common cause of iron deficiency anemia is chronic blood loss – abnormal menstrual bleeding – intestinal bleeding • IRON DEFICIENCY ANEMIA IN A MAN OR IN A POST-MENOPAUSAL WOMAN IS TO BE CONSIDERED BLEEDING FROM GI CANCER UNTIL PROVEN OTHERWISE Hemolytic Anemia Hereditary Spherocytosis • Associated with • Disorder of a structural protein in – active, hypercellular bone marrow the cell membrane – high reticulocytes – increased LDH increased LDH • Results in splenic • Results in splenic hemolysis – low blood haptoglobin – increased bilirubin • Genetic & non-genetic causes 2
7/3/2011 G6PD Deficiency Sickle Cell Anemia • Lacking enzyme • Hemoglobin S that protects the • Sickling precipitated by RBC from oxidation – low O 2 tension 2 – infections – dehydration – acidosis Thalassemias • Molecularly correct but not enough produced • Several varieties – thalassemia major is most j severe – most common type is a severe microcytic hypochromic anemia • stimulates iron absorption • can lead to hemachromatosis Non-Genetic Hemolytic Anemia Iron Deficiency Anemia • About 80% of iron is in hemoglobin with the rest stored as ferritin & • Immune hemolytic hemosiderin anemia • Plasma ferritin levels vary directly with the amount of ferritin in bone marrow – antibodies directed against • Transferrin transports iron RBC antigens – TIBC measures total transferrin • Mechanical hemolytic y – % saturation of TIBC is measuring how much iron is actually bound to – % saturation of TIBC is measuring how much iron is actually bound to the transferrin anemia • TIBC is high – hemolyzed as they pass • Plasma iron is low through mechanical • % saturation is low devices such as artificial • Most common cause is chronic blood loss heart valves – menstrual abnormalities • Associated with malaria – GI bleeding 3
7/3/2011 Macrocytic Anemia • aka megaloblastic anemia • Due to vitamin B 12 or folic acid deficiencies – needed for DNA synthesis • Hyperactive, hypercellular bone marrow • Most common cause is defective intestinal absorption Most common cause is defective intestinal absorption – intrinsic factor – gastrectomy – surgical resection of ileum – inflammatory bowel disease • Pernicious anemia – autoimmune disease – associated with chronic atrophic gastritis Aplastic Anemia • Failure to produce all blood cells • Idiopathic • Results in pallor & fatigue • Thrombocytopenia • Low WBC count • Hypocellular bone marrow Myelophthisis • Bone marrow replaced by tumor or fibrosis • Fibrosis usually due to radiation but could be a manifestation of a myeloproliferative syndrome syndrome 4
7/3/2011 Polycythemia Leukopenia • Too many RBCs • Low WBC count • Relative • Caused by – low plasma volume such as in dehydration – hypersplenism – “stress polycythemia” – autoimmune disease autoimmune disease • Absolute – sepsis – primary – bone marrow problem • polycythemia vera – secondary • Agranulocytosis • due to – severe neutropenia – hypoxia from chronic lung disease – caused mostly by drugs – high altitude Leukocytosis • Too many WBCs • Can be reactive or malignant Leukemias Reactive Leukocytosis • Neutrophilia • Acute • Chronic – bacterial infections – immature cells – mature cells – leukemoid reaction if count > 50,000 – aggressive – less aggressive • Lymphocytosis – short course – longer course – viral infections – abrupt onset abrupt onset – insidious onset insidious onset • Eosinophilia – symptoms include – symptoms include – allergic reactions or parasitic infections • anemia • fatigue • “Bands” • infections • pallor – when demand is great • bleeding • night sweats • bone pain • infections – “shift to the left” • enlarged lymph nodes • splenomegaly • hepatomegaly 5
7/3/2011 Infectious Mononucleosis Lymph Node Response • Acute, self-limited • Infection • Atypical lymphocytes • Malignancy • Epstein-Barr virus • Immune reactions – infects B cells – heterophile antibodies • Autoimmune disease • Signs/symptoms – fever – sore throat – enlarged lymph nodes • Monospot test Lymphadenopathy Acute Lymphocytic Leukemia • Enlarged nodes • ALL – tender = infectious • Uncommon – non-tender = malignant – mostly in children & young • Lymphadenitis adults – lymph node is infected l h d i i f t d • Immature B cells • Reactive hyperplasia • Abrupt onset – acute • Results in • dental infections, sore throat, genital infections – bone pain – chronic – lymphadenopathy • TB – hepatosplenomegaly Chronic Lymphocytic Leukemia • CLL • B cells • About 1/3 of all leukemias • Difficult to distinguish from small cell lymphocytic lymphoma • Mostly in adults • Slow developing 6
7/3/2011 Plasma Cell Dyscrasias • Activated B cells • Make too much of a particular antibody • On electrophoresis, appears as a dark band called an M-spike b d ll d M ik • Light chains can pass through glomerulus & into urine – Bence-Jones proteins Multiple Myeloma • Malignant cells appear as nodular masses in bone marrow Multiple Myeloma • Malignant cells appear as nodular masses in bone marrow • “punched out” lesions in skull & spine 7
7/3/2011 Multiple Myeloma • Malignant cells appear as nodular masses in bone marrow • “punched out” lesions in skull & spine • Hypogammaglobinemia H l bi i • Susceptible to infections • Elderly most commonly affected Lymphomas Hodgkin Lymphoma • EBV • Characteristic cell is Reed- Sternberg (RS) cell • Most common neoplasm between 10 30 yrs old 10-30 yrs old • Usually have poor T cell immunity • Arises in a single lymph node or chain of nodes & spreads in an orderly manner • Rarely involves anything but lymph nodes • Neoplasms of lymphocytes or lymphoblasts that grow as nodular masses usually in lymph nodes Non-Hodgkin Lymphomas • Usually painless, non- • B cells tender enlarged lymph • Aggressive node in neck • Weight loss • Usually in advanced stage when • Night sweats • Night sweats diagnosed di d • Fever • 1/3 arise in organs other than lymph nodes • Fatigue • Tend to spread widely • Infection • Good survival but at risk for other malignancies 8
7/3/2011 Follicular Lymphoma Diffuse Lymphomas • About 50% • About 50% • Less aggressive • No follicles • Painless, enlarged lymph nodes • Usually over 60 except for childhood lymphomas & those in AIDS l h & th i AIDS • Appear quickly & grow rapidly • Lethal unless treated Acute Myelocytic Leukemia • AML • Myeloblasts • Usually in middle age & older adults • Sudden onset • Marrow failure Marro fail re – anemia – infection – bleeding – bone pain – lymphadenopathy – hepatosplenomegaly Chronic Myeloproliferative Chronic Myelocytic Leukemia Disorders • 2 features occur to some degree in each disorder • CML • Myelofibrosis • Granulocytes – bone marrow replaced by fibrous tissue – due to fibrogenic factors released by megakaryocytes • Middle-aged adults usually • Extramedullary hematopoiesis – blood cell production outside of the marrow blood cell production outside of the marrow • About 15% of adult leukemias • About 15% of adult leukemias • Slow onset but progressively worsens • > 100,000 cells • May end in a “blast crisis” 9
Recommend
More recommend