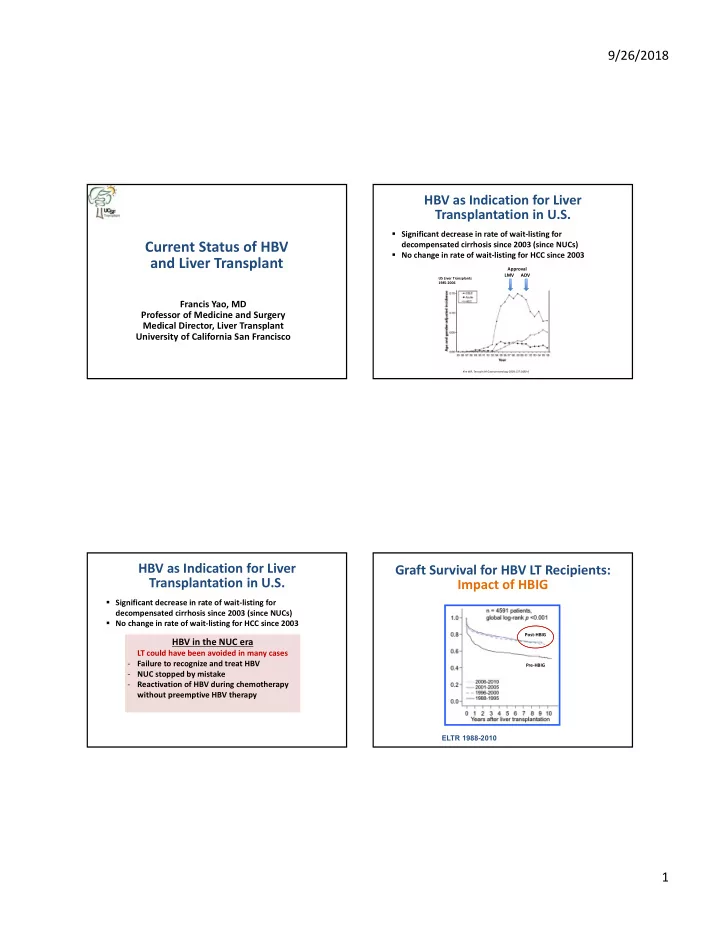
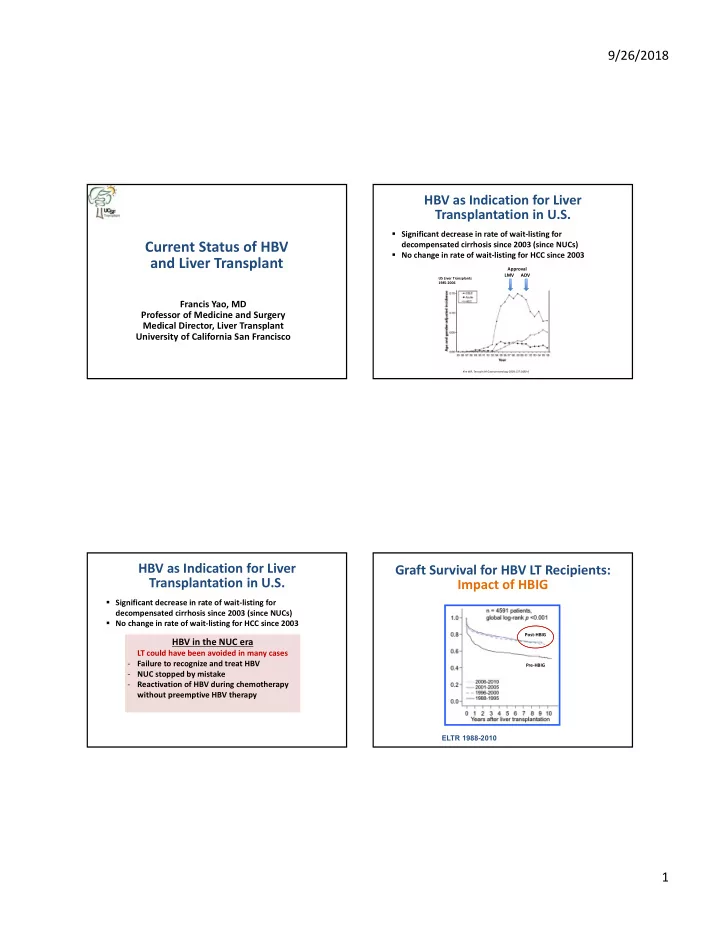
9/26/2018 HBV as Indication for Liver Transplantation in U.S. Significant decrease in rate of wait‐listing for Current Status of HBV decompensated cirrhosis since 2003 (since NUCs) No change in rate of wait‐listing for HCC since 2003 and Liver Transplant Approval LMV ADV US Liver Transplants 1985‐2006 Francis Yao, MD Professor of Medicine and Surgery Medical Director, Liver Transplant University of California San Francisco Kim WR, Terrault NA Gastroenterology 2009;137:1680‐6 HBV as Indication for Liver Graft Survival for HBV LT Recipients: Transplantation in U.S. Impact of HBIG Significant decrease in rate of wait‐listing for decompensated cirrhosis since 2003 (since NUCs) No change in rate of wait‐listing for HCC since 2003 Post‐HBIG HBV in the NUC era LT could have been avoided in many cases ‐ Failure to recognize and treat HBV Pre‐HBIG ‐ NUC stopped by mistake ‐ Reactivation of HBV during chemotherapy without preemptive HBV therapy ELTR 1988-2010 1
9/26/2018 Prevention and Treatment HBV of Post‐ Algorithm for Management of Patients Transplant With Cirrhosis Chronic hepatitis HBIG Entecavir Entecavir Acute hepatitis Plus Compensated Decompensated Tenofovir Tenofovir NUC Transplant Graft loss Any HBV DNA Any HBV DNA Prevent Prevent Level Prevent Level Listed infection cirrhosis graft or and graft infection hepatitis failure Treat Indefinitely Treat Indefinitely Refer for Liver Transplantation Pre‐Transplant Prophylactic Antiviral therapy Antiviral Therapies for recurrent Therapy disease Lifelong therapy needed Terrault NA, AASLD HBV Treatment Guidelines 2016 Preferred Treatments for Treatment of Tenofovir Alafenamide (TAF) for Chronic HBV HBV in Patients with Cirrhosis Mean ( ± SD) change in eGFR CG Renal Safety TAF TDF Antiviral Risk of (mL/min) Drug Name Side Effects -0.6 Potency Resistance p <0.001 -4.7 Entecavir (ETV) +++ Lactic acidosis (rare) Very Low* Tenofovir Lactic acidosis (rare) disoproxil +++ Some risk renal and bone None Spine and Hip BMD fumarate (TDF) toxicity Spine Hip Tenofovir Lactic acidosis (rare) P <0.001 2 Alafenamide +++ Minimal renal and bone None Mean (SD) % Change Change in Bone Mean (SD)% Change from Mineral Density (TAF)** toxicity from Baseline 0 -0.29 -0.88 Baseline P <0.001 -2 * Rate of resistance higher in patients who have prior lamivudine resistance -2.16 -2.51 **TAF has not been studied in patients with decompensated cirrhosis -4 -6 AASLD HBV Treatment Guidelines Week 0 24 48 Week 0 24 48 EASL HBV Treatment Guidelines Buti EASL 2016, Oral GS06; Chan, EASL 2016, Oral GS12 2
9/26/2018 Antivirals may Reverse Decompensation Maintained Virologic Response (MVR) Influences Transplant‐Free Survival and Prevent Need for LT N=295 HBV patients with decompensation initiated on antiviral therapy Compassionate access program for adefovir 1999‐2003 Median follow‐up 5.2 yrs; median survival 7.7 yrs N=100 CPS A=40%, B=40%, C=21% 36% 43% 21% Still Wait Listed Transplanted Removed from Wait List 86% Improved 14% Not Improved 50% Improved/Stabilized 14% Not Improved Highest mortality in first 6 months: 17.3% vs 25.3% between 6 mos 10 yrs 30% Death* MVR is key to better long‐term survival (HR 2.30) * All deaths occurred 2% No F/U Entecavir more likely to achieve MVR than Lamivudine survival difference within 24 weeks Schiff E et al, Liver Transplant, 2007 Jang JW, CGH 2018 Pre‐Transplant Management of Severity of Decompensation Strongly Patients with HBV Influences Short‐Term Survival All patients with cirrhosis should be maintained on Short‐Term Mortality 60 Multivariate Analysis of Predictors antiviral therapy life‐long 55.3 of Mortality within 6 Months ETV, TDF or TAF are preferred options 50 HR P Value If decompensated, highest risk of death/need for LT (95%CI) 40 in first 6 months Multiple 3.60 0.001 30 Complications (1.71‐7.55) % Maintenance of viral suppression important for MELD>20 8.32 <0.001 20 (3.98‐17.41) long‐term survival with and without LT 10.3 10 Monitor HBV DNA every 3‐6 months 0 MELD≤20 MELD≥20 Jang JW, CGH 2018 3
9/26/2018 Prevention and Treatment HBV of Post‐ HBV Prophylaxis in Liver Transplant Transplant Recipients Chronic hepatitis HBIG Entecavir Entecavir HBIG plus NUC is “ standard of practice ” in most LT Acute hepatitis Plus Tenofovir Tenofovir centers NUC Transplant Graft loss Efficacy ~95% with current NUCs + HBIG Prevent Prevent Prevent Listed infection Target anti‐HBs titer ~100 U/L cirrhosis graft or and graft infection Use of NUCs with high genetic barrier to hepatitis failure resistance Move towards minimization of HBIG in recent decade Pre‐Transplant Prophylactic Antiviral therapy Antiviral Therapies for recurrent Therapy disease Lifelong therapy needed Factors Influencing Practice Patterns in Efficacy of Prophylactic Regimens in HBV Prophylaxis Preventing HBV Recurrent Post‐LT Systematic review Limitations of HBIG Cost Median follow-up HBsAg positive % Recurrence 30 months ETV/TDF P<0.001 Availability (especially in Asia) 37 months LMV Inconvenient parenteral administration Availability of effective antiviral therapy P=0.51 (NUC) Many patients have undetectable HBV DNA levels at time of LT HBIG HBIG + HBIG HBIG +LMV ETV/TDF +TDF + ETV Total N: 1889 309 197 106 Cholongitas E, Am J Transplant 2013 4
9/26/2018 Prophylaxis for HBV Post‐Transplant: Stopping HBIG and Continuing NUC Discontinuation of HBIG Unique Features of Recurrence Systematic review: Median duration of HBIG before discontinuation= 24 months (range: 11–31) HBsAg may reappear but HBV DNA remains undetectable (especially if NUC(s) with high genetic barrier to resistance used) HBIG + ETV HBsAg may subsequently disappear spontaneously or HBIG + TDF with change in anti‐viral therapy HBsAg ETV /TDF with Lack of adherence frequently cited a cause for % HBIG D/C recurrence NUC resistance reported primarily in studies with LMV used as maintenance NUC Fox and Terrault, J Hepatol 2012 Cholongitas E, Am J Transplant 2013 Cholongitas E, Am J Transplant 2013 HBV Prophylaxis Using Short‐Course HBV Prophylaxis with NUC Alone Peri‐operative HBIG Plus NUC NUC with high barrier to resistance needed Single center study Early experience with LMV revealed high rates of N=46 consecutive patients Cumulative Incidence at 3 Years resistance prophylaxis failure with HBV DNA <1000 IU/mL 10 at LT (without HIV or HDV) Virologic failure in absence of rescue therapy 8 HBIG 5000 IU intraop and results in rapidly progressive disease and graft loss daily for 5 days plus life‐long 6 % Adherence to treatment is critical NUC 3.3 4 2.9 N=2 patients with ETV (if no prior LMV), TDF or TAF best options 2 recurrence of HBsAg Suppression of HBV DNA to low levels pre‐LT may N=1 N=1 positivity or viremia had 0 Recurrence improve success of NUC only strategy post‐LT HCC diagnosed within a HBsAg+ HBV DNA+ month of detection Perrillo R, Hepatology 2001;33:424-32 Nery J, Transplantation 1998;65:1615-21 Radhakrishnan K, Transplantation 2017 Fung J, Gastroenterology 2011;141:1121-9 5
9/26/2018 Individualize Prophylactic Therapy Prophylaxis with NUC Monotherapy Efficacy Measures by NUC Used Consider if high or low risk for recurrent HBV High Risk Low Risk NUC used N HBV DNA HBsAg + Survival* HDV or HIV coinfection HBV DNA undetectable to <100 relapse 3 yrs last f/u HBV DNA ≥10 4 IU/ml pre‐LT IU/mL pre‐LT (on antivirals) Wild‐type HBV LMV 176 17% 20% 87% (unrecognized or acute HBV) Drug‐resistant HBV Compliant ETV 142 0% 17% 92% Risks for non‐adherence Combo 44 7% 21% 93% Short duration HBIG (5 (mostly LMV+ADV) Combination HBIG and days-4 wks) + ETV or NUCs (possibly long-term) TDF/TAF long-term Median follow-up 4.4 yrs * No HBV-related deaths; 1 re-transplant for recurrent cholestatic Include combination NUCs ETV or TDF/TAF hepatitis with known efficacy against monotherapy drug-resistant HBV Fung J, Am J Gastroenterol 2013; 108(6):942-8. Terrault NA et al. AASLD HBV Guidance 2018 Prevention and Treatment HBV of Post‐ Treatment of HBV Recurrence Post‐LT Transplant Chronic hepatitis HBIG No role of HBIG Entecavir Entecavir Acute hepatitis Plus Tenofovir Tenofovir NUC Preferred antivirals are those with high Transplant Graft loss barrier to resistance: ETV, TDF or TAF Prevent Prevent Prevent Listed infection No convincing evidence that combination better cirrhosis graft or and graft than monotherapy if preferred drugs used infection hepatitis failure TDF/TAF preferred if prior LMV treatment Life‐long suppressive therapy needed HCC surveillance for those with advanced Pre‐Transplant Prophylactic Antiviral therapy Antiviral Therapies for recurrent fibrosis Therapy disease Lifelong therapy needed Terrault NA et al. AASLD HBV Guidance 2018 6
Recommend
More recommend