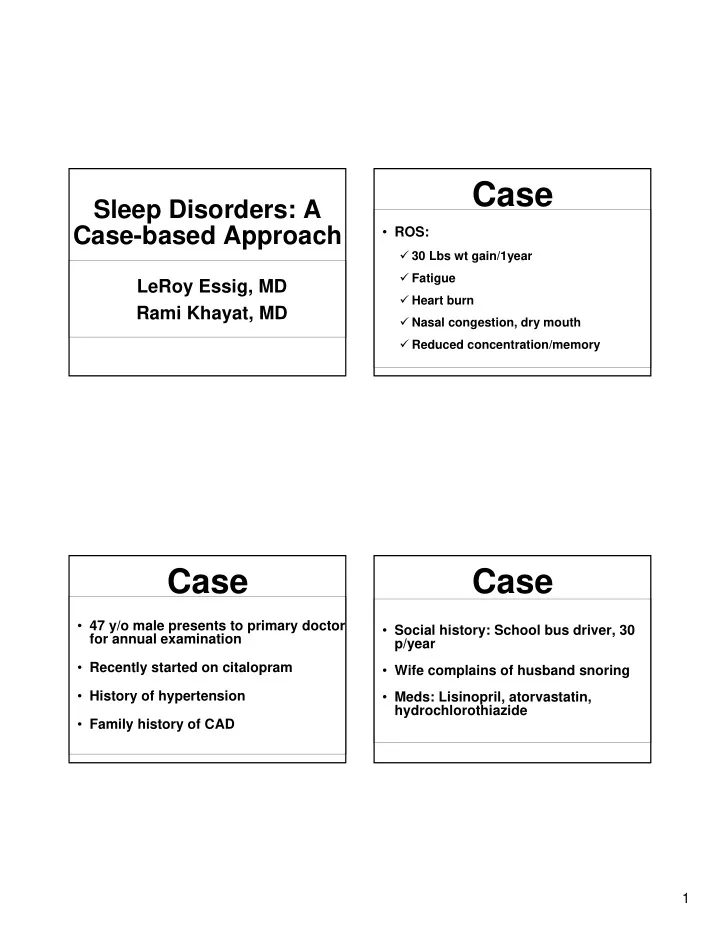
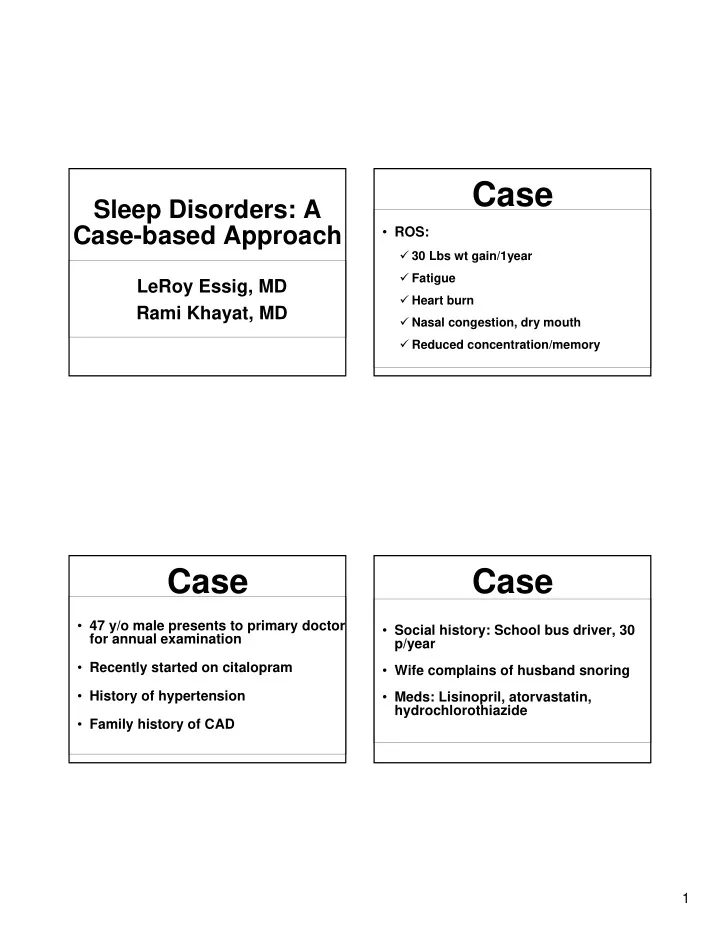
Case Sleep Disorders: A Case-based Approach • ROS: � 30 Lbs wt gain/1year � Fatigue LeRoy Essig, MD � Heart burn Rami Khayat, MD � Nasal congestion, dry mouth � Reduced concentration/memory Case Case • 47 y/o male presents to primary doctor • Social history: School bus driver, 30 for annual examination p/year • Recently started on citalopram • Wife complains of husband snoring • History of hypertension • Meds: Lisinopril, atorvastatin, hydrochlorothiazide • Family history of CAD 1
Sleep History Physical Examination • Exam: Weight 212, BMI 35, BP 147/87 • Struggling to stay awake during • Big uvula, nasal passages narrow, daytime “thick neck” • 6 hours of sleep per night with a 1 • Lungs clear hour nap in the early afternoon, 2-3 beers/night • Heart regular, no gallop, clear lungs • Watches TV in bed before sleep • No peripheral edema • Intact sensation and strength in LE’s Sleep History • Awakens 3-4 times at night to use rest room What problems did you • Persistent loud snoring identify in this patient? • Leg jerks and kicks, restless sleep • Wife “gradually” sleeping in another room 2
Problems • General: Arrange problems in � Poorly controlled HTN � Cardiovascular risk factors order of Importance � Heartburn Problems Problems in Order of Importance • Sleepiness • Sleep � Professional driver � Fatigue, depression • Poorly controlled hypertension � Snoring, sleepiness • Smoking � Restless sleep/legs • Obesity � Dissatisfied spouse • Depression • Restless legs 3
Daytime Sleepiness Differential Diagnosis • Inadequate sleep time • Sleep deprivation for 1 day or sleeping 2 hours less/day for a week resulted in the • Poor sleep hygiene same driving impairment as a blood alcohol level of 0.089 g/dL (Powell, 2001). • Obstructive Sleep Apnea • 2002 NHTSA survey of 4010 adult drivers • Periodic Limb Movement of Sleep/Restless Leg Syndrome • Of the 11% who admitted to nodding off while driving in the previous year, 2/3 stated they had ≤ 6 hours of sleep • Inadequately treated depression the previous night • Medication side effects Daytime Sleepiness Assessment of Sleepiness The Epworth Sleepiness Scale • 16% of adults experience excessive SITUATION CHANCE OF DOZING sleepiness that impairs daily functioning 1-Sitting and reading (Young, 2004). 2-Watching TV • More than 100,000 automobile accidents 3-Sitting inactive in a public place each year are due to drivers falling asleep (I.e. a theater or a meeting) 4- As a passenger in a car (National Highway Traffic Safety for an hour without break Administration). 5- Lying down to rest in the afternoon � 71,000 non-fatal injuries when circumstances permit 6-Sitting and talking to someone � 1500 fatalities 7-Sitting quietly after lunch without alcohol 8 -In a car, while stopping for a few minutes � 12.5 billion dollars in annual all-cause in traffic monetary loss 0 = Would never doze 1 = Slight chance of dozing 2 = Moderate chance of dozing 3 = High chance of dozing 4
Prevalence of Obstructive What is the most effective Sleep Apnea next intervention? • Evaluate for OSA! � Improved sleep hygiene and expanded sleep alone are unlikely to reduce sleepiness if OSA is untreated � OSA is linked to hypertension, cardiovascular disease, periodic limb movement and depression The Occurrence of Sleep-Disordered Breathing among Middle-Aged Adults The Wisconsin Sleep Cohort, NEJM 1993 Obstructive Sleep Symptoms of OSA Apnea • OSA- why should I care? • Snoring • Excessive daytime sleepiness • If I have to care, what should • Witnessed apneas I do about it? • Poor memory and concentration, irritability or personality changes • Other: Dry throat, morning headache, • Treatment of OSA and CSA in patients and nocturia with heart disease is a waste of time ! 5
Effects of Sleep Diagnosis on the Upper Airway • History and physical examination • Loss of tone in genioglossus, palatal, • Questionnaires and pharyngeal constrictor muscles • Pulse oximetry • Supine position and reduced lung • Portable sleep studies volumes • Polysomnography OSA-Imbalance between Dilating Physical Examination and Constricting Forces of the in OSA Upper Airway • Neck circumference • Dilating forces: � > 17 inches in males � pharyngeal muscle tone � > 16 inches in females � Lung volumes • Craniofacial anatomy • Constricting forces: � Inferiorly positioned hyoid bone � Negative inspiratory � Mandibular insufficiency pressure � Increased mid-facial height � Extra luminal fat • Nasal obstruction 6
Sleep Study- Why should this patient Polysomnography be treated urgently? • Professional driver with sleepiness LOC ROC • Poorly controlled hypertension Chin EMG C3-A2 • Cardiovascular risk O2-A1 EKG • Depression Nasal flow Chest Abdomen • Quality of Life SaO 2 Prospective Data From Case: Results of the Wisconsin Sleep Cohort Study (N=913) Sleep Study (Young et al, Sleep 20:608, 1997) Any MVA in 5 years (n=165) • Sleep Efficiency: 68% Increased Relative Risk Men Women • Wakefulness and arousal index: 37/hour No SDB Reference category = 1.0 Snorer, RDI <5 3.4* 0.9 • Respiratory disturbance index: 42/hour RDI 5-15 4.2* 0.8 RDI >15 3.4* 0.6 • Periodic Limb Movement Index: 32/hour *Significant increase compared to reference category INCREASED RISK OF CRASHES EVEN WITH MILD OSA 7
Derivation of Patient Population Relationship Between Severity pf Sleep Apnea and Crash Risk (N=460, OSA) Used in Study of CPAP and Crashes (George et al, Sleep 22:790, 1999) (George, Thorax 56:508, 2001) 0.14 Crash Rate (Number/Year) Confirmed OSA (n=740) p<0.01 0.12 0.1 0.08 Driving records available (n=582) 0.06 0.04 CPAP treatment (n=317) 0.02 0 Control RDI 10-25 RDI 26-40 RDI >40 Clinic follow-up for >3 years (n=210) Only increased risk RDI >40 Does Sleep Apnea Increase Association of OSA Crash Rates? and Depression Answer Yes • Different data about relationship between crash risk and severity of illness • Severe sleep apnea is a risk factor for ↑ crashes • Is mild-to-moderate sleep apnea a risk factor for ↑ crashes—Not clear • Does treatment reduce crash risk? Yes Peppard, P. E. et al. Arch Intern Med 2006;166:1709-1715. 8
The Cardiovascular Consequences of Sleep Apnea Increased Sympathetic Nerve Activity in OSA (Somers et al J Clin Invest 1995; 96:1897-1904) Components of the Increased Incidence of Coronary Artery Disease in OSA Cardiovascular Response to Apnea • Hypoxia • Increased sympathetic activity • Blood pressure surge • Increased respiratory effort • Arousal Pecker et al Eur Resir J 2006 9
Association of Hypertension and OSA Can Kill Patients with Sleep-Disordered Breathing -- Sleep Coronary Disease Heart Health Study 2.5 OR adjusted for age, sex, Respiratory Odds Ratio (OR) ethnicity 2 Disturbance Index: OR adjusted for age, sex an independent 1.5 ethnicity, and BMI predictor of mortality 1 n=6440 in coronary artery p=0.0001 for linear disease 0.5 trend 0 <1.5 1.5-4.9 5-14.9 15-29.9 >30 (Ref) RDI (episodes/hour) Nieto et al, JAMA 283:1829, 2000 Pecker et al. AJRCC 2005 OSA And Association Between Sleep Apnea and Incident Hypertension Hypertension During 4 Year Follow Up Period • 40% of patients with OSA have Hypertension at Follow-up 5 OR adjusted for baseline Odds Ratio (OR) for hypertension 4.5 hypertension status 4 OR for above + age, 3.5 • 50% of patients with hypertension gender, BMI, etc. 3 have OSA 2.5 Hypertension = BP of 2 at least 140/90 or use 1.5 • OSA patients were more likely to be of anti-hypertensive 1 medications nocturnal “non-dippers” 0.5 0 • Treatment of OSA reduces blood 0 (Ref) 0.1-4.9 5.0-14.9 >15 pressure Baseline AHI Peppard et al, NEJM 342:1378-1384, 2000 10
Obstructive Sleep Association of OSA and Type II Diabetes Reichmuth et al AJRCCM 2005 Apnea and Stroke Young et al AJRCC 2005 Association of OSA and Type II Diabetes Obstructive Sleep Apnea Reichmuth et al AJRCCM 2005 and Outcome of Stroke 4 year odd ratio of physician diagnosed DM over 4 year of follow up Mohsenin NEJM 2005 11
Association Between Severe OSA (AHI >30) OSA Can Cause Heart Failure and Arrhythmias in Sleep Heart Health Study (Mehra et al, AJRCCM, doi:10.1164/rccm.200509-1442OC) 5 Arrhythmia Type Unadjusted Odds Ratio* Odds Ratio* (95% 4.5 Odds Ratio (95% CI) CI) Adjusted for n=6,424 4 Adjusted for Age, Sex, BMI, 3.5 Age, Sex, BMI CHD 3 Non-sustained 4.64 3.72 3.40 OR 2.5 CHF ventricular (1.48-14.57) (1.13-12.2) (1.03-11.2) 2 tachycardia 1.5 1 Complex 1.96 1.81 1.74 0.5 ventricular (1.28-3.00) (1.16-2.84) (1.11-2.74) ectopy 0 I II III IV Atrial fibrillation 5.66 3.85 4.02 AHI Interquartile range (1.56-20.52) (1.00-14.93) (1.03-15.74) BMI=body mass index; CHD=coronary heart disease *Results of logistic regression analysis with SDB as the exposure; N=338 without SDB, N=228 with SDB E Shahar, et al, AJRCCM, 2001 Higher Prevalence of Predicted OSA in Sudden Cardiac Death in OSA Patients Presenting with AF Compared to General Cardiology Patients (Gami et al, Circ 110:364, 2004) N Engl J Med 2005;352:1206-14. 12
Recommend
More recommend