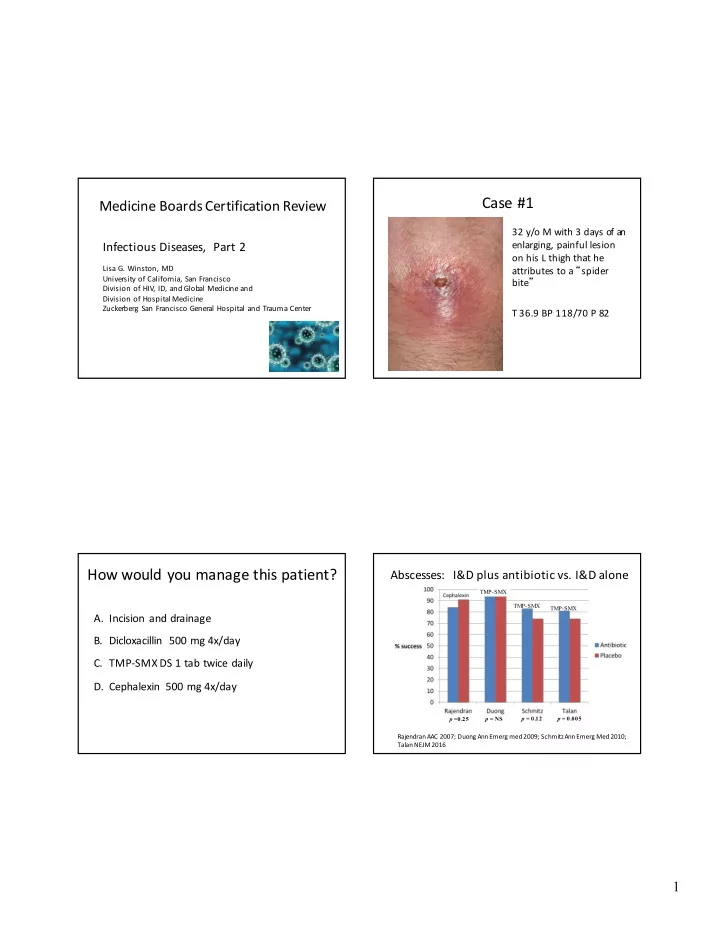
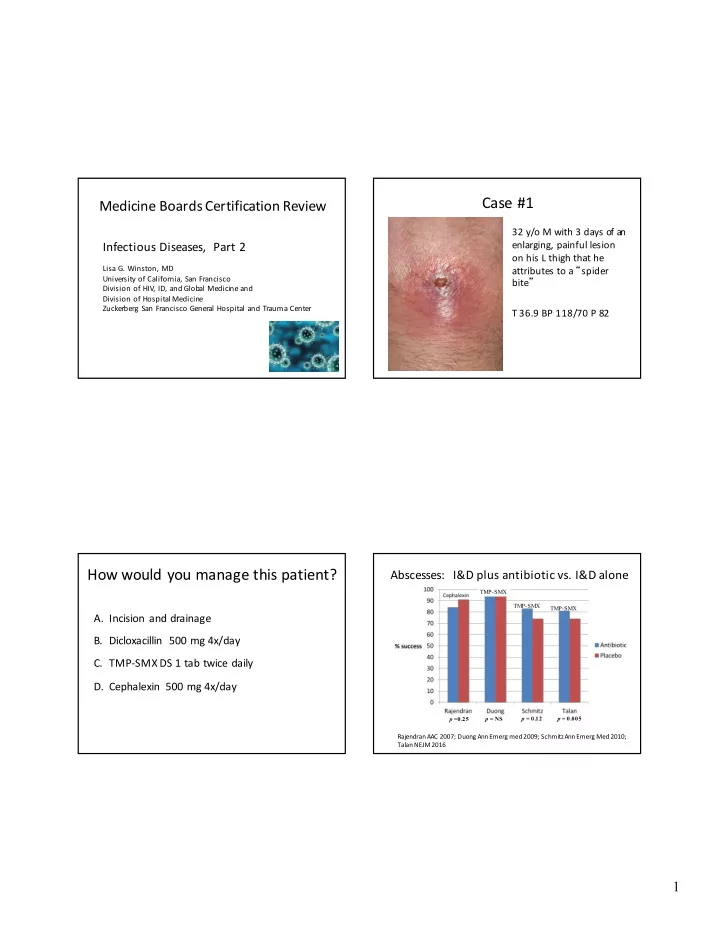
Case #1 Medicine Boards Certification Review 32 y/o M with 3 days of an Infectious Diseases, Part 2 enlarging, painful lesion on his L thigh that he Lisa G. Winston, MD attributes to a “ spider University of California, San Francisco bite ” Division of HIV, ID, and Global Medicine and Division of Hospital Medicine Zuckerberg San Francisco General Hospital and Trauma Center T 36.9 BP 118/70 P 82 How would you manage this patient? Abscesses: I&D plus antibiotic vs. I&D alone TMP-SMX TMP-SMX TMP-SMX A. Incision and drainage B. Dicloxacillin 500 mg 4x/day C. TMP-SMX DS 1 tab twice daily D. Cephalexin 500 mg 4x/day p = 0.12 p = 0.005 p =0.25 p = NS RajendranAAC 2007; Duong Ann Emerg med 2009; Schmitz Ann Emerg Med 2010; Talan NEJM 2016 1
Antibiotic therapy recommended for abscesses Abscesses: I&D plus antibiotic vs. I&D alone associated with: • Benefits to antibiotics • Severe disease – Slightly higher cure rates • Signs or symptoms of systemic illness – Decrease in new skin infections (short-term) • Immunosuppression – T alan 2016 study also showed lower rate subsequent surgical drainage and decreased • Extremes of age infections in household members • Difficult to drain area (face, hand, genitalia) • Failure of prior I&D Liu C. Clin Infect Dis . 201 1 Oral antibiotic treatment for Microbiology of Purulent SSTIs purulent SSTI Drug Adult Dose TMP/SMX DS 1-2 tab twice daily 100 mg twice daily Doxycycline, Minocycline Clindamycin 300-450 mg 3x/day Linezolid 600 mg twice daily *Rifampin is NOT recommended for routine treatment of SSTIs Moran NEJM 2006 2
Case #2 How would you manage this patient? 28 y/o woman presents A. Watch closely for self-resolution with erythema of her left foot over past 48 hrs B. Cephalexin 500 mg 4x/day No purulent drainage, C. Cephalexin 500 mg 4x/day plus TMP-SMX 1 exudate, or fluctuance. DS twice daily D. Admit for IV vancomycin with rapid transition T 37.0 BP 132/70 P 78 to oral antibiotics when improved Clindamycin vs. TMP-SMX for Cephalexin vs. Cephalexin + TMP-SMX in patients with Uncomplicated Cellulitis uncomplicated skin infections N=146 n = 160 n = 280 p = 1.00 p = 0.38 Miller NEJM 2015 Pallin CID 2013; 56: 1754-1762 3
Empirical treatment of complicated Treatment of uncomplicated non-purulent skin and soft tissue infections cellulitis • Admitted to floor with abscess or cellulitis Drug Adult Dose – I&D abscess Cephalexin 500 mg 4x/day – Vancomycin or alternative antibiotic (consider Dicloxacillin 500 mg 4x/day cefazolin for cellulitis) • Alternative: daptomycin, linezolid, tedizolid, Clindamycin* 300-450 mg 3x/day dalbavancin, oritavancin, telavancin, ceftaroline TMP-SMX* (new) 1-2 DS twice daily – No need for Gram negative coverage • Patient admitted to ICU / necrotizing fasciitis Linezolid* 600 mg 2x/day – Vancomycin or alternative + Gram negative *Activity against MRSA coverage + clindamycin Case #3: Case #3: A. Ciprofloxacin for 3 days An 85 year-old woman is admitted to the hospital B. Ciprofloxacin for 10 days with a CHF exacerbation. Other co-morbid C. Trimethoprim-sulfamethaxazole for 3 days conditions include diabetes and chronic kidney D. Fosfomycin for 1 day disease (creatinine = 2.5 mg/dL). A urinalysis shows 10 – 20 WBC/HPF. A urine culture is sent E. Nitrofurantoin for 7 days and grows pan-sensitive E. coli > 100,000 cfu/mL. F. No antibiotics The patient denies specific urinary symptoms. Which is the best course of action? 4
Urinary Tract Infections Urinary Tract Infections • Uncomplicated cystitis • Recurrent cystitis in women (> 3x/year) • Women, pre-menopausal, non-pregnant, no urologic – Daily or 3x weekly prophylaxis abnormalities – Post-coital prophylaxis • Escherichia coli 70-90% – Self-treatment for symptoms • > 35% ampicillin resistance • Self diagnosis accurate • > 20% trimethoprim/sulfametho xazole resistance in man y areas – Other measures • Nitrofurantoin (5 days) is generally reliable • Discontinue diaphragm and/or spermicide • IDSA guidelines recommend avoiding fluoroquinolones • Topical estradiol in post-menopausal women • ? Cranberry juice Gupta et al. Clin Infect Dis 2011;52(5):e103-120 Urinary Tract Infections Urinary Tract Infections • Pyelonephritis • Imaging (U.S. or CT) – Obtain urine culture • Not better in 72 hours – Outpatient initial rx: fluoroquinolone • Multiple episodes – Hospitalize • Lower threshold in men • Inadequate p.o. intake • Severe disease/underlying illness • Tip: remember not to use moxifloxacin for • Pregnancy UTIs – Initial rx in hospital: fluoroquinolone; aminoglycoside; extended-spectrum cephalosporin (ceftriaxone); extended-spectrum penicillin; carbapenem • May switch to TNP-SMX if susceptible 5
Case #4: Case #4: 60 y.o. woman with HTN presents with 3 days of cough A. Oral antibiotics at home with green sputum, dyspnea on exertion, fever, B. Hospitalize for IV antibiotics initially; when pleuritic chest pain. She otherwise has no past afebrile, switch to oral antibiotics and discharge medical history. home Exam: C. Hospitalize for IV antibiotics initially; when • 38.5º 145/90 100 18 95% RA afebrile, switch to oral antibiotics and discharge • Chest: crackles at left base after 24 hours observation Data: WBC: 15,500 CXR: LLL infiltrate D. Hospitalize for minimum of 7 days of IV • What is the most appropriate treatment? antibiotics Pneumonia Severity Index Pneumonia Severity Index Examination Demographic Mental status (+20) Class PSI score Mortality Triage Age (+1 point/yr , -10 if woman) Pulse > 125 (+20) Nursing home (+10) Resp rate > 30 (+20) I Age < 50, no comorbidity, 0.1% outpatient SBP < 90 (+15) stable vital signs Comorbidities T emp < 35 or > 40 (+10) II ≤ 70 0.7% outpatient Cancer (+30) Labs Liver disease (+20) III 71-90 3% consider CHF (+10) pH < 7.35 (+30) BUN > 30 (+20) admission Cerebrovascular dz (+10) Na < 130 (+20) Renal disease (+10) IV 91-130 8% admission Glucose > 250 (+10) p02 < 60 (+10) Hct < 30 (+10) V > 130 29% ? ICU Don’t memorize this! Pleural effusion (+10) 6
Admission for community- CAP: When to Discharge acquired pneumonia? Inpatient: Safe to discharge when afebrile, • Outpatient: hemodynamically stable, not hypoxic, and – Doesn’t meet outpatient – Younger tolerating PO treatment criteria – No cancer or end- No minimum duration of IV therapy needed organ disease – Hypoxia • – No severe vital sign – Active coexisting condition No need to watch in-hospital on oral antibiotics • abnormalities – Unable to take oral meds For most patients with CAP, 7 total days of • – No severe laboratory – Psychosocial issues antibiotic treatment is adequate abnormalities Case #5: Case #5: A. Cefuroxime IV 82 y.o. man presents with 5 days of productive cough and dyspnea. His past medical history is notable for B. Levofloxacin IV COPD. Denies recent travel or hospitalization. Exam: C. Piperacillin / tazobactam (Zosyn) IV + 39º 110/90 110 24 85% RA • Chest: crackles at right base vancomycin IV • Data: CXR: Right lower & middle lobe infiltrates D. Cefepime IV + tobramycin IV • Labs: WBC 12,000, BUN=38, otherwise normal • What is the most appropriate treatment? 7
Empirical Treatment for Outpatients Etiology of CAP No comorbidity or recent • Macrolide or • Clinical syndrome and CXR not predictive of antibiotics • Doxycycline organism – Streptococcus pneumoniae – Haemophilus influenzae Comorbid condition(s) (age § b -lactam (e.g. – Mycoplasma pneumoniae > 65, EtOH, CHF, severe liver o r amoxicillin) + either – Chlamydophila pneumoniae renal disease, cancer, etc.) macrolide or Covered by – Legionella or doxycycline usual regimes – (Enteric Gram negative rods) Antibiotics in last 3 months or • Respiratory Not covered by – Viruses fluoroquinolone* usual regimens – Staphylococcus aureus (many) * NOT Ciprofloxacin Empirical Treatment for Inpatients Diagnostic Testing in CAP § b -lactam + either macrolide or Inpatient Chest radiography: • doxycycline non-ICU Indicated for all patients with suspected pneumonia – or Cannot distinguish atypical vs. typical pathogen – • Respiratory fluoroquinolone Blood culture: • § b -lactam + either azithromycin or Inpatient ICU respiratory fluoroquinolone Recommended for some inpatients, based on – severity of illness (before antibiotics) (Penicillin allergy: fluoroquinolone + aztreonam) Sputum exam: • • Antipseudomonal b -lactam or Healthcare Recommended for some inpatients – carbepenem + either fluoroquinolone associated Most helpful if single organism in large numbers – or aminoglycoside pneumonia Molecular testing increasingly available • (Controversial and still being revised) MRSA concern • Add vancomycin or linezolid to above 8
Recommend
More recommend