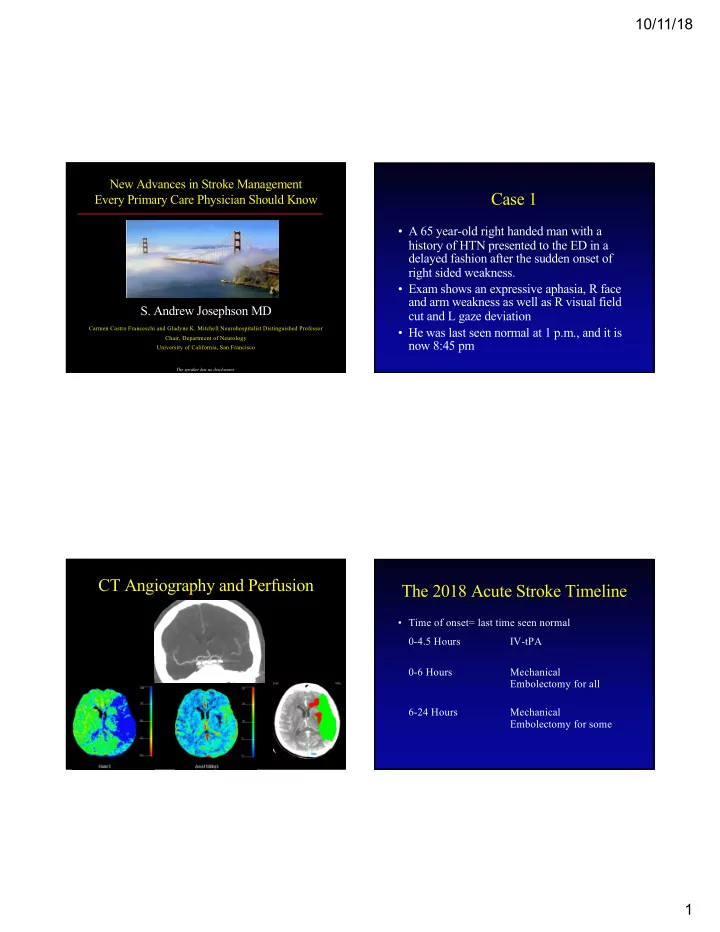
10/11/18 New Advances in Stroke Management Case 1 Every Primary Care Physician Should Know • A 65 year-old right handed man with a history of HTN presented to the ED in a delayed fashion after the sudden onset of right sided weakness. • Exam shows an expressive aphasia, R face and arm weakness as well as R visual field S. Andrew Josephson MD cut and L gaze deviation Carmen Castro Franceschi and Gladyne K. Mitchell Neurohospitalist Distinguished Professor • He was last seen normal at 1 p.m., and it is Chair, Department of Neurology now 8:45 pm University of California, San Francisco The speaker has no disclosures CT Angiography and Perfusion The 2018 Acute Stroke Timeline • Time of onset= last time seen normal 0-4.5 Hours IV-tPA 0-6 Hours Mechanical Embolectomy for all 6-24 Hours Mechanical Embolectomy for some 1
10/11/18 The 2018 The 2015 Endovascular Revolution Second Revolution • Five major positive trials of endovascular • DAWN and DEFUSE3 Trials therapy all published in 2015 in NEJM • Select patients with LVO treated up to 24 • Trial design somewhat differed, but hours based on CT perfusion selection common to each: – Automated CT software widely available – 1. Used newer-generation devices • Has led to major reexamination of triage – 2. Selected patients who were eligible via CTA – 3. IV t-PA in those who were eligible followed by and ED/hospital protocols embolectomy – 4. Typically a 6 hour time window Nogueira R et al: N Engl J Med 378:11, 2018 Albers GW, et al: N Engl J Med 378:708, 2018 What do we do given this data? What do we do given this data? • 1. All patients eligible for IV t-PA should • 4. If the patient has a LVO and presents receive it (quickly) between 6-24 hours, CT perfusion is required and selects patients who should • 2. Patients within 6 hours should receive a receive endovascular therapy CTA to look for a large vessel occlusion (LVO) • 5. Consider IV tPA for some outside of the 4.5 hour window with MRI selection • 3. If LVO present, endovascular therapy should occur, even following IV t-PA regardless of perfusion data 2
10/11/18 Wait! Case 2 What about tPA Out of the Window? • A 76 year-old man with a history of • A substantial number of patients wake up smoking presents with 3 days of R hand with a stroke or can’t tell us their time of weakness onset • Examination shows a R pronator drift and • Some will have had a stroke in the last few hours and therefore IV tPA may work slowed movements of the R hand • Important positive trial used MRI to select • The patient takes aspirin 81mg daily as well these patients (+DWI but –FLAIR) as lisinopril Thomalla et al: N Engl J Med 379:611, 2018 Which of the following is not part of Standard Large-Vessel Stroke Workup the standard stroke workup? • Cardioembolic: afib, clot in heart, A. Echocardiogram paradoxical embolus B. Extended cardiac telemetry • 1. Telemetry • 2. TEE with bubble study C. Lipid panel • Aortic Arch D. B12, TSH, RPR, ESR • 2. TEE with bubble study • Carotids E. Carotid evaluation • 3. Carotid Imaging (CTA, US, MRA, angio) • Intracranial Vessels • 4. Intracranial Imaging (CTA, MRA, angio) And evaluate stroke risk factors 3
10/11/18 Atrial Fibrillation TEE vs. TTE Detection • 231 consecutive TIA and stroke patients of • EKG unknown etiology underwent TTE and TEE • 48 Hours of Telemetry • 127 found to have a cardiac cause of emboli, 90 of • Long-term cardiac event monitor (>21d) which (71 percent) only seen on TEE – 15-20% of patients with cryptogenic stroke • TEE superior to TTE for: LA appendage, R to L otherwise unexplained had afib detected shunt, examination of aortic arch – Clearly changes management • More recent study: TEE found additional findings – Probably cost effective in 52% and changed management in 10% De Bruijn S et al: Stroke 37:2531, 2006 Gladstone D et al: N Engl J Med 370:2467, 2014 Katsanos AH, et al: Neurology 87:988, 2016 Shrinking Indications for Approach to Stroke Treatment Anticoagulation in Stroke 1. Atrial Fibrillation Acute Stroke Therapy? 2. Some other cardioembolic sources No – Thrombus seen in heart – ?EF<35 Anticoagulants? – ?PFO with associated Atrial Septal Aneurysm 3. Vertebral or Carotid dissection No 4. Rare hypercoagulable states: APLS Antiplatelets 4
10/11/18 The “Absolute Mess” New Data: N Engl J Med 2017 of PFO in Stroke RESPECT RE Gore REDUCE Go CLOSE CL Stroke attributed to PFO + • Around 20-25% of all patients have a PFO Cryptogenic stroke within Cryptogenic stroke within atrial septal aneurysm OR Inclusion Criteria past 270 days + PFO past 180 days + PFO large PFO • PFO alone is not necessarily associated with Participants 980 participants 644 participants 663 participants higher risk of recurrent stroke Intervention Arm PFO closure PFO closure + antiplatelet PFO closure + antiplatelet – Higher risk: Larger PFO, associated atrial septal Antiplatelet or Arm 1: antiplatelet aneurysm, perhaps younger age Medical Rx Arm Antiplatelet anticoagulation Arm 2: anticoagulation • Three previous negative trials of closure Less recurrent clinical and Less recurrent stroke with Less recurrent stroke with clinical+radiographic stroke Results PFO closure (NNT 42) PFO closure (NNT 20) devices but cardiologists pre-2017 were still with PFO closure (NNT 28) performing these procedures widely What now? Rules of the Road “Let’s close all these PFOs!” • DO NOT close all these PFOs • Consider PFO closure if: – The patient is younger than 60 years old • DO screen patients for PFO (?how) – AND you can be sure the PFO is the most • It is sensible to discuss with your likely etiology after a thorough workup cardiologists some “Rules of the Road” – AND the qualifying event is a stroke (not TIA) • At the end of the day, this is an exciting that appears embolic (not lacunar) advance for some (young) people with – Likely concentrate on large PFOs or those with stroke that can make a substantial impact on an atrial septal defect recurrence rates • Cardiologists new task: start counting bubbles 5
10/11/18 The Excitement Over the Risks to Discuss With Your Patients Demise of Warfarin • Atrial Fibrillation rates higher • Oral direct thrombin and Xa inhibitors will • No great data beyond 5-10 years hopefully lead to more patients with afib being anticoagulated • Antiplatelet regimens variable but most • Stroke-specific concerns include duals for some time and then monotherapy – Little acute data for secondary prevention – Contraindications to tPA – And what if AF develops? – Reversal now less of a concern • Major risk for stroke is up front rather than spread throughout subsequent years • Medical management: Options appear equal Stroke workup is unrevealing. Case 3 Your Treatment? • A 70 year-old man with a history of DM, A. Increase ASA to 325mg daily smoking presents 10 hours after the onset of B. Add Plavix to ASA slurred speech and mild right arm weakness. C. Stop ASA, start Plavix • The patient is on ASA 81mg daily D. Stop ASA, start Aggrenox E. Anticoagulate 6
10/11/18 Approach to Stroke Treatment Antiplatelet Options Acute Stroke Therapy? • 1. ASA – 50mg to 1.5g equal efficacy long-term No • 2. Aggrenox – 25mg ASA/200mg ER Dipyridamole Anticoagulants? • 3. Clopidogrel (Plavix) No – Multiple secondary prevention studies (CHARISMA, SPS3) show no long-term Antiplatelets benefit in combination with ASA PRoFESS Trial Antiplatelet Options • Randomized, double-blind trial of Aggrenox • If on no antiplatelet medication versus Plavix in over 20,000 patients with – Plavix vs. Aggrenox (or ASA) ischemic stroke • If already on ASA • Recurrent 4-year event rates basically identical – Switch to Plavix vs. Aggrenox between the two medications • If already on Plavix or Aggrenox – HR for Aggrenox 1.01 (95% CI, 0.92-1.11) – Composite of stroke, MI, vascular death: 13.1% in each – ??? – Major hemorrhagic events higher in Aggrenox group Sacco RL et al: N Engl J Med 359:1238, 2008 7
10/11/18 Clopidogrel + ASA: When to use Dual Antiplatelets Ever A Winning Combination? • POINT trial • NOT all the time! • Select those with only minor or no deficits • After minor stroke or TIA for only 90 days (NIHSS 3 or less or ABCD2 of 4 or more) • After a fresh carotid or coronary stent • Nearly 5000 TIA or Minor Stroke patients • With severe intracranial atherosclerosis (>70%) assigned to 90d of daily ASA + Placebo versus and stroke/TIA in that territory for only 90 days daily ASA + Clopidogrel following 600mg load • Modestly improved efficacy (1.5%) • Minimally (0.5%) more hemorrhage Johnston SC et al: N Engl J Med 379:215, 2018 Other Acute Stroke Management Permissive Hypertension • Statins for (almost) all • National Guidelines – SPARCL (NEJM 8/06), 80mg atorvastatin in stroke and – To at least 220/120 TIA if LDL>100 – After IV tPA: less than 185 systolic for 24 hours • Tight Glucose and Fever control • We typically stop all meds except half-dose • Enoxaparin for DVT prophylaxis β -blockers – PREVAIL trial (Lancet 2007) – CLOTS trial 1 (Lancet 2009): Compression Stockings 8
Recommend
More recommend