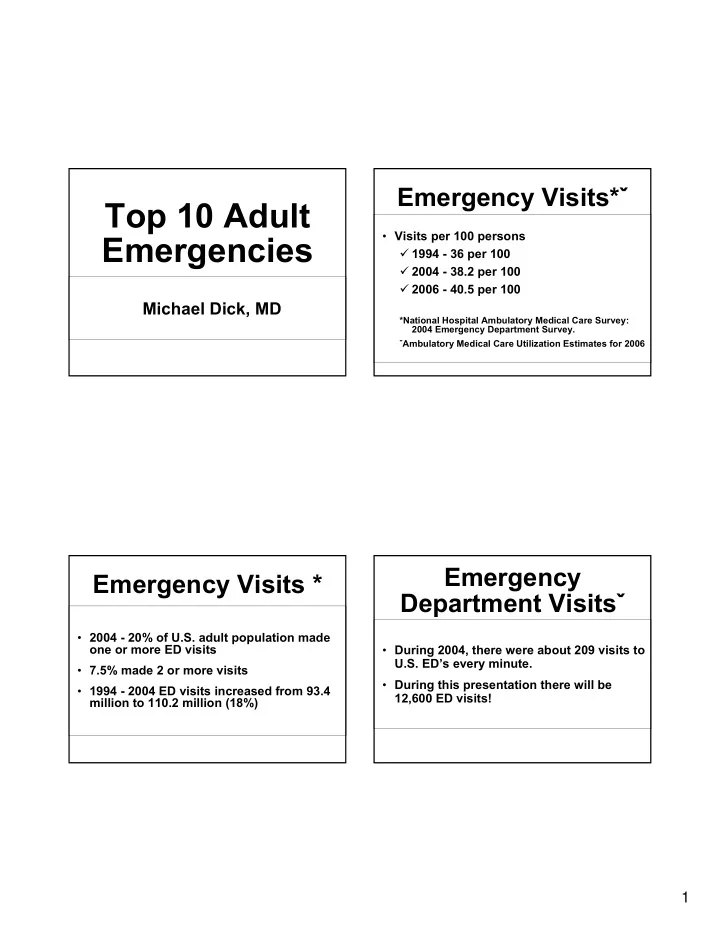
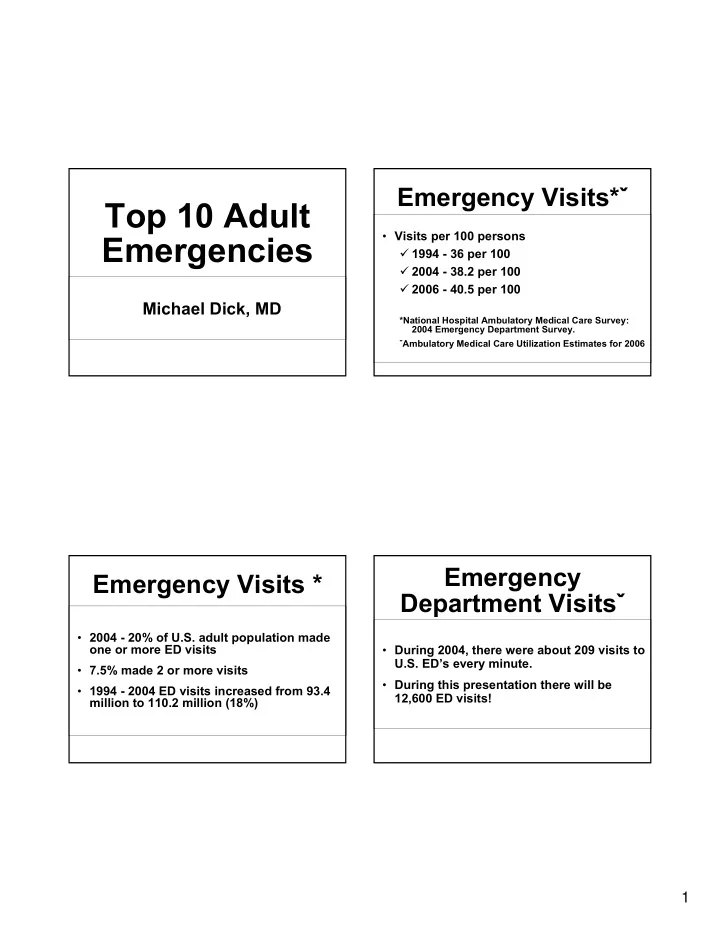
Emergency Visits* ˇ Top 10 Adult • Visits per 100 persons Emergencies � 1994 - 36 per 100 � 2004 - 38.2 per 100 � 2006 - 40.5 per 100 Michael Dick, MD *National Hospital Ambulatory Medical Care Survey: 2004 Emergency Department Survey. ˇ Ambulatory Medical Care Utilization Estimates for 2006 Emergency Emergency Visits * Department Visits ˇ • 2004 - 20% of U.S. adult population made one or more ED visits • During 2004, there were about 209 visits to U.S. ED’s every minute. • 7.5% made 2 or more visits • During this presentation there will be • 1994 - 2004 ED visits increased from 93.4 12,600 ED visits! million to 110.2 million (18%) 1
Most Common Chest Pain Presentations • Cardiac • Most frequent principle reasons for visit � ACS, MI, Pericarditis, Aortic Dissection � Abdominal pain • Pulmonary � Chest pain � Pulmonary Embolism, Pneumonia, � Fever Pneumothorax � Musculoskeletal symptoms • Musculoskeletal � Digestive symptoms • Gastrointestinal � Respiratory symptoms � Reflux, Esophageal rupture Acuity STEMI • 12.9% Emergent • 37.8% Urgent • 21.8% Semiurgent • 12.5% Nonurgent • Age >65 higher proportion of Emergent • 13% Admitted 2
STEMI - PCI STEMI • Transfer arrangements • Aspirin • STEMI patients presenting to hospital with • Clopidogrel 600 mg loading dose PCI capability should be treated within 90 (<75 yrs of age)* minutes of first medical contact • Beta blockers � Note: first medical contact = EMS to • Unfractionated Heparin- 60u/kg, 4000u max balloon • No Drips * Cuisset, Frere, et al, J.Am. Coll. Cardiol. 2006,48;1339-1345. STEMI Guidlines STEMI • STEMI patients presenting to a hospital • Focused Update of the ACC/AHA Guidelines for Management of Patients With ST-Elevation Myocardial without PCI capability, and who cannot be Infarction ( Journal of the American College of Cardiology) transferred to a PCI center and undergo � http://content.onlinejacc.org/cgi/content/full/j.jacc.200 PCI within 90 min of first contact, should be 7.10.001 treated with fibrinolytic therapy within 30 The full-text guidelines are also available on the Web • minutes of hospital presentation. sites: � ACC/AHA 2007 STEMI Guidelines � ACC - www.acc.org and, AHA - www.americanheart.org 3
Aortic Dissection Aortic Dissection • Ripping or tearing pain • Type A = ascending (Debakey I & II) • Abrupt onset � Surgical treatment • Pain location may vary • Type B = no ascending involvement (III) • Neurologic symptoms/findings in up to 20% of patients • Mortality can approach 50% at 48 hours in those untreated • Hypertension • Pressure differential ≥ 20mmHg Aortic Dissection Aortic Dissection • Male:female 3:1 • Peak age 50-65 yrs • ECG may show ST elevation or depression • Risk factors • D-dimer (?) � Connective tissue disease • Chest radiograph � Hypertension • CT angiography, Echocardiography, MRI � Pregnancy � Syphilis � Cocaine 4
Aortic Dissection Aortic Dissection Aortic Dissection Aortic Dissection • Aggressive control of heart rate and BP � 100-120 mmHG � 60-80 beats per minute � Monitor end organ perfusion • Urgent surgical evaluation for Type A • Pain control 5
Aortic Dissection Pulmonary Embolism • Pharmacologic agents • Kline JA, et al. Clinical Criteria to Prevent Unnecessary diagnostic testing in emergency � Beta blockers department patients with suspected pulmonary • Esmolol embolism. J. Thromb Heamost 2004;2: 1247-55 • Labetalol • Prospective multicenter evaluation of the • Metoprolol pulmonary embolism rule out criteria. J Thromb Heamost 2008; 772-80 � Nitroprusside Dr. Michael DeBakey Pulmonary Embolism 1908-2008 • PERC Criteria � Age < 50 � Pulse < 100 � Sa02 >94% � No unilateral leg swelling � No recent surgery � No prior PE or DVT � No oral hormone use 6
Abdominal Aortic Pulmonary Embolism Aneurysm • PERC criteria • 13th leading cause of death in U.S. � When physicians had a low clinical gestalt, the sensitivity of 97.45 • Males 7x more often than females � Defined those patients in whom NO additional testing was needed. • 75% are > 60 years old Abdominal Pain AAA • Asymptomatic until expand or rupture • Aortic Abdominal Aneurysm • Expanding AAA may cause sudden, severe back, abdominal, groin, or flank pain • Ectopic Pregnancy • Rupture AAA present with shock • Ovarian Torsion • 65-70% die prior to hospital 7
AAA AAA • Initial vital signs may be normal if rupture • Bedside ultrasound good for is contained screening and can detect free fluid • Pulsatile mass is seen in less than 1/2 • Pain with hypotension, shock, and mass in only 30-50 of cases CT scan is study of choice • Initial misdiagnosis of 20-40% • High index of suspicion AAA Ectopic Pregnancy • Treat hypotension • Assume all females with abdominal pain � Target blood pressure are pregnant • 19.7 per 1000 pregnancies Reverse any coagulopathy • Most occur in women 25-34 Immediate surgical consultation • Higher incidence in those on fertility drugs 8
Ectopic Pregnancy Ectopic Pregnancy • Quantitative HCG • Pain- abdominal, pelvic, shoulder � Discriminatory level • Syncope or near syncope � Approximately 1000 mIU/ml • 30% have no vaginal bleeding • Beware heterotopic pregnancy � 1 in 3,000 pregnancies Ectopic Pregnancy Ovarian Torsion • Sudden or gradual onset of lower • Quantitative hcg abdominal pain • CBC � Radiation to back is common • Ultrasound � Pain may be bilateral � May demonstrate IUP � Nausea and vomiting in 70% � May demonstrate extra uterine mass • Ovary is abnormal in over 50% of � May demonstrate free fluid cases 9
Ovarian Torsion Stroke • Consider stroke in any patient with • Pregnancy test neurologic deficit or altered level of consciousness. • Ultrasound with color Doppler • When was the patient last seen normal? • Beware of mimics - seizure, metabolic, toxic, infectious, trauma Ischemic Stroke Stroke • Physical exam • Leading cause of disability in the U.S. � Signs of trauma • Third leading cause of death � Signs of infection • One third of stroke patients < 65 yo � NIH Stroke Scale • “Time is Brain” • 0-42 points • Roughly 4% of patients with stroke • ≥ 10 correlates with visible lesions on receive rt-PA angiography 10
Stroke Stroke • Non- contrast CT is imaging modality • Key Thrombolytic criteria of choice � Measurable deficit • MR may be considered but should not � Not spontaneously clearing delay treatment � Not minor and isolated • CBC, chemistries, coagulation, tox Stroke Stroke • Key Thrombolytic Criteria • Key Thrombolytic criteria � If on anticoagulant - INR < 1.7 � With in 3 hours of symptom onset � Blood pressure < 185 mmHg Systolic � European Cooperative Acute Stroke Study III, 2008 - may extend window up � Blood pressure < 110 mmHg Diastolic to 4.5 hours � Seizure is not absolute contraindication 11
Stroke Infectious • Blood pressure control • Epidural abscess � If not eligible for thrombolytics • MRSA � Systolic ≤ 220, diastolic ≤ 120 observe • Sepsis � Systolic >220, diastolic 122-140 • Labetalol or nicardipine � Diastolic >140 • Nitroprusside Stroke Epidural Abscess • Musculoskeletal complaints very common • No role for heparin or other • Red flags anticoagulants in acute phase of care � Fever � Neurologic deficit � Risk factors 12
Spinal Epidural Abscess Spinal Epidural Abscess • Although rare, incidence has doubled in the • Co-morbidities - predisposing factors past 2 decades. � Diabetes, alcoholism, HIV • Classic triad is � Spinal abnormality - instrumentation, djd, � Back pain - 75% trauma, injections � Fever - 50% � Source of infection -skin, urine, catheter � Neurologic deficit -33% � IV drug use, tattooing � All three present in a minority of patients Spinal Epidural Abscess Spinal Epidural Abscess • Diagnosis • Symptoms often progress � Clinical findings � Back pain � Leukocytosis 2/3rds patients � Nerve root pain � Elevated ESR, CRP (non-specific) � Motor weakness, sensory deficit, bladder/bowel dysfunction • Imaging � Paralysis � MRI with contrast 13
MRSA Spinal Epidural Abscess • Treatment - Antibiotics - cover MRSA (vancomycin) and gram negative bacilli - Surgery - decompressive laminectomy - Neurologic symptoms present for less than 24-36 hours - Facilitate treatment by draining abscess Skin Infections MRSA • Community acquired � Patients have NOT been in hospitals • “Abscessologist” � Genetically UNRELATED to H-MRSA • MRSA - hospital acquired vs. � Genomic sequencing - USA300-0114 community acquired � Arginine Catabolic Mobile Element (ACME) � Prevalent in S. epidermidis � More effective cutaneous colonization 14
C-MRSA C-MRSA • Moran, et al NEJM, August 2006 • Risk factors? • Study - August 2004 � “Over crowding” (prisoners) • 11 University Affiliated EDs � Close contact - athletes • 59% skin and soft tissue infections = � IV drug users (?) CMRSA • 97% USA300-0114 Close Contact! C-MRSA • OSU - 75% + cultures of skin and soft tissue from ED are MRSA 15
Recommend
More recommend