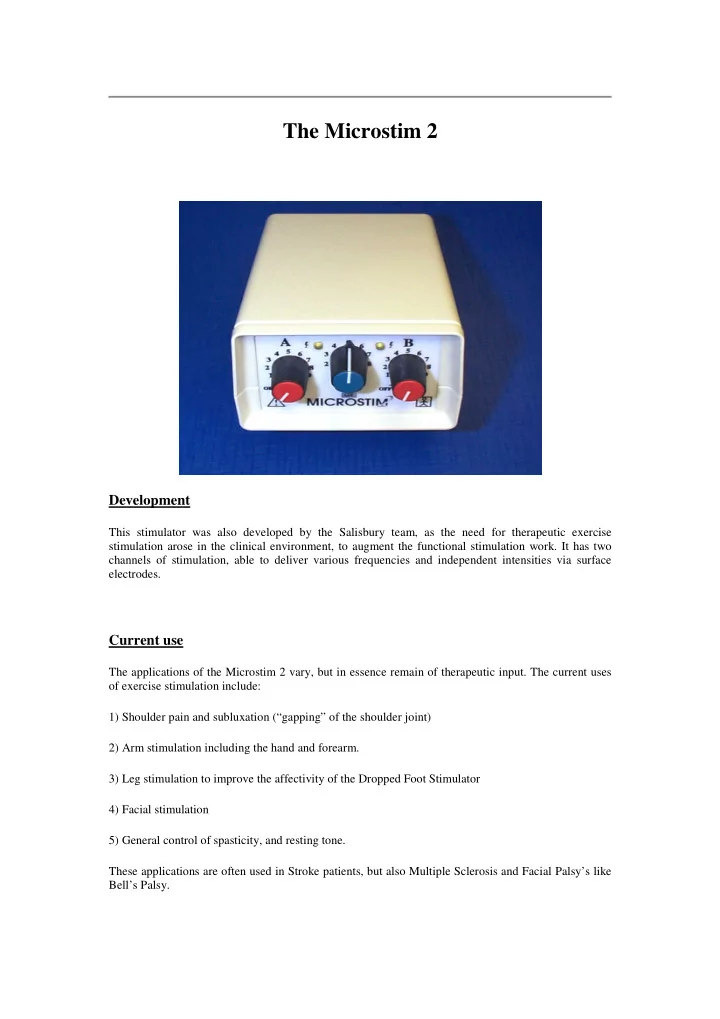
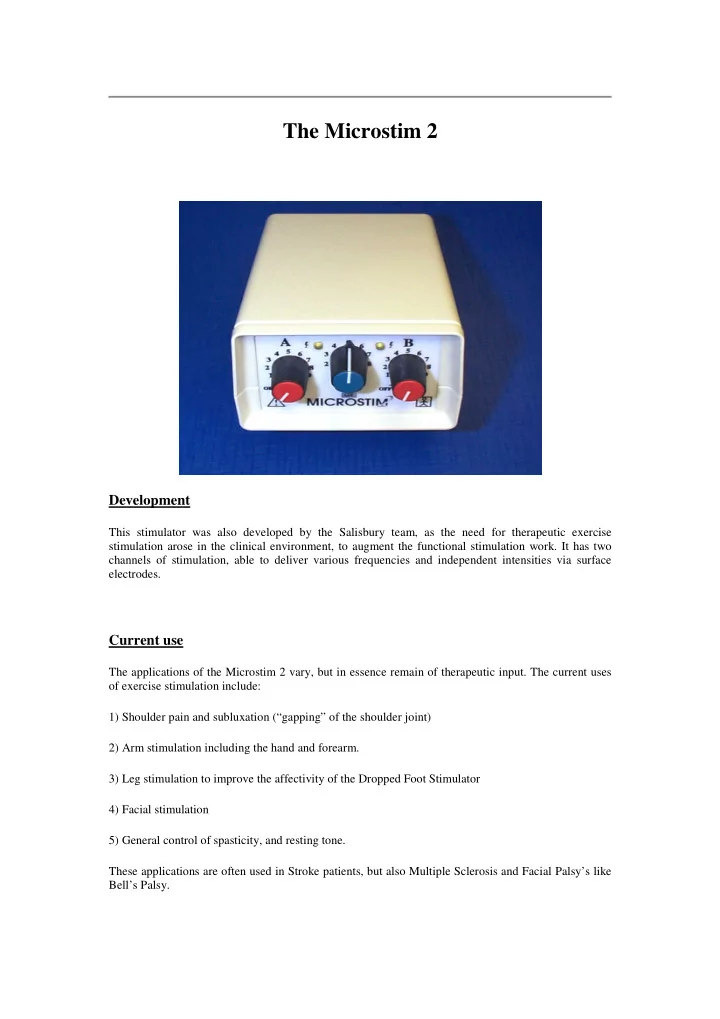
The Microstim 2 Development This stimulator was also developed by the Salisbury team, as the need for therapeutic exercise stimulation arose in the clinical environment, to augment the functional stimulation work. It has two channels of stimulation, able to deliver various frequencies and independent intensities via surface electrodes. Current use The applications of the Microstim 2 vary, but in essence remain of therapeutic input. The current uses of exercise stimulation include: 1) Shoulder pain and subluxation (“gapping” of the shoulder joint) 2) Arm stimulation including the hand and forearm. 3) Leg stimulation to improve the affectivity of the Dropped Foot Stimulator 4) Facial stimulation 5) General control of spasticity, and resting tone. These applications are often used in Stroke patients, but also Multiple Sclerosis and Facial Palsy’s like Bell’s Palsy.
What does using the system involve? Exercises are usually prescribed twice a day, slowly increasing the time of stimulation until stimulating for approximately 30 minutes twice daily. The electrodes will be applied only for this period, during which functional activities can be carried out as prescribed by a Physiotherapist. The mode setting on the stimulator allows for the integration of stimulating muscle groups, or individual alternating stimulation. Future developments This stimulator is also currently being redesigned, although there will be no technical changes to the current device. Functional Electrical Stimulation & Spinal Cord Injuries Incomplete injuries. The electrical stimulation parameters used in the Odstock range of stimulators allows for nerve stimulation only, and is therefore unable to induce any movement in denervated muscles. This denervation would occur as a result of a lower motor neuron injury. As a rough guideline, this occurs in patients with a spinal cord injury of the level of L1 (Lumber 1) and lower. When being used in patients with a lesion higher than this, in order to achieve any sort of functional improvement, there needs to be some element of incompleteness to the clinical picture. In other words there needs to be some specific element absent from an already moderately functioning lower limb, or arm. The patients usually seen are those mobile using some form of walking aid already, and are perhaps using an Ankle foot orthosis to improve the walking by keeping the foot in a semi lifted position. FES offers an alternative to conventional treatment, encouraging active movement of the foot, and by constantly taking the foot through full range of movement with walking, avoids stiffening up of the ankle. Improvements are reflected in objective tests, recording the speed of walking and the effort of walking by measuring the heart rate. Common reports are of walking being made easier, quicker, and safer, with patients feeling a lot more confident in walking about. Carry-over of these improvements is often found when looking at unstimulated walking too, indicating a training effect of stimulation. Other improvements are also found in decreasing calf tone and improving range of movement, and peripheral circulation. Improved standing symmetry is also encouraged due to the nature of the foot switch- stimulation relationship. Two channels of stimulation are also used at times, in order to integrate another set of muscles into the walking pattern. This might include the hamstring muscles to improve the knee bending when bringing the foot forwards, or to the gluteal muscles to bring the body over the effected leg when standing. The quadriceps muscles may also be stimulated to improve standing stability. Exercise stimulation may also be applied to the leg in order to improve the effect of the above- mentioned systems, or to the upper limb for therapeutic stimulation. This could be done using the 2- or 4-chnnel stimulator. 2
Tetraplegics Patients who have suffered from a cervical cord injury usually have limited upper limb function, and are wheelchair dependent for mobility. Conventional treatment involves physiotherapy and occupational rehabilitation, and tendon transfers may be done to improve hand function. NeuroControl, a company based in the USA has now developed the Freehand System", which involves the implantation of 8 electrodes into the muscles of the hand and forearm. These are stimulated via an external system by transmitting radio frequencies to an implanted receiver unit. This is often done together with tendon transfers, and enables the patient to perform tasks using a shoulder control to bring on different movements of the hand. The patient is then able to grasp objects, and manipulate them spatially. Selection criterion is strict, as some patients may benefit from tendon transfers alone. Usual candidates are C5/6/7 injured patients. Currently this surgery is not being performed in South Africa, but the Salisbury unit in the UK, others in Europe, Japan, Australia, Canada and the USA do. For more information, go to the NeuroControl website. Other possibilities include abdominal stimulation to improve respiratory function by improve coughing, and decreasing the occurrence of orthostatic hypotention (a lowering of the blood pressure in response to body position, resulting in dizziness/fainting). Publications 1. Taylor PN, Ewins DJ, Fox B, Grundy D, Swain ID. Limb blood flow, cardiac output and quadriceps muscle bulk following spinal cord injury and the effects of training for the Odstock Functional Electrical Standing System. Paraplegia 31 (1993) 303-310 2. Taylor PN, Burridge JH. Development and experience in use of an electronic stimulator for correction of dropped foot in early gait re-education of subjects following CVA. Therapy weekly 1993 3. Taylor PN, Fox BA, Ewins DJ, Swain ID, Exercise procedure and treatment routine for preparation of paraplegics prior to standing using FES. Ed. Cliford-Rose F, Jones R, Vrbova G. Neuromuscular Stimulation: Basic Concepts and Clinical Practice. Demos 1989 USA 4. Ewins DJ, Taylor PN, Crook SE, Lipcyznski RT, Swain ID. Practical low cost stands/sit system for mid-thoracic paraplegics. J.Biomed. Eng. 1988 10(2): 184-188 5. Burridge J, Taylor P, Hagan SA, Wood DE, Swain ID. The effect on the spasticity of the quadriceps muscles of stimulation of the Common Peroneal nerve of chronic hemiplegic subjects during walking. Physiotherapy vol. 83, no 2, pp 82-89 1997 6. Burridge, J. Taylor, P. Swain, I. (1997) Clinical Experience of the Odstock Drop Foot Stimulator. Artificial Organs 21 (3): 254-260 7. Burridge, J. Taylor, P. Hagan, S. Swain, I (1997) The effect of Common peroneal stimulation on the effort and speed of walking. A randomised controlled trial with chronic hemiplegic subjects. Clinical Rehabilitation 11: 201-210 8. Rushton DN, Barr FMD, Donaldson N de N, Harper VJ, Perkins TA, Taylor PN, Tromans AM. Selecting candidates for a lower limb stimulator implant programme: a patient-centred method. Spinal Cord (1998) 36 303-309 9. Burridge JH, Swain ID, Taylor PN Functional electrical Stimulation: a review of the literature published on common peroneal nerve stimulation for the correction of dropped foot. Reviews in Clinical Gerontology 1998 8: 155-161 3
Recommend
More recommend